Introduction
Malignant ascites (MA), which can develop through various pathological mechanisms, poses a significant challenge in terminal cancer patients [1-3]. Once MA develops, survival times are short, and the patient’s quality of life decreases markedly [1]. MA can cause several physiological symptoms, including abdominal bloating and discomfort, shortness of breath, decreased appetite, fatigue, nausea, pain, reduced mobility, and peripheral edema. Additionally, it can lead to psychological symptoms such as mood disorders [3,4]. Given its impact not only on the patient but also on their caregivers, effective management of MA is essential. However, the absence of large-scale, randomized, and controlled studies has left a gap in establishing a standardized treatment protocol.
The curative treatment for MA is the treatment of the underlying disease; however, this is often not feasible in terminal-stage malignancies. As a result, the approach primarily focuses on palliative solutions. The first option that comes to mind is diuretic therapy, but it is often insufficient. Repeated large-volume paracentesis (RLVP) is a commonly used method for symptomatic relief, but the rapid reaccumulation of ascites necessitates frequent procedures [5]. These repeated invasive interventions increase the frequency of hospital visits and complications such as pain and bleeding [5]. Peritoneo-venous shunt (PVS) placement is another option, but its high cost and significant risk of major complications limit its use [3]. Additionally, its contraindication in gastrointestinal cancers, which are among the most common causes of MA, further restricts its applicability [3]. Although studies on tumor-targeted therapies are promising, there is no standard tumor-targeted therapy yet [6,7].
The use of pigtail peritoneal catheters in MA treatment has become increasingly widespread. While the literature reports high procedural success rates, there is variability in the incidence of complications and catheter dwell times. Most studies have been small in scale, focusing primarily on procedural success and complication rates, without examining factors such as treatment indication and follow-up processes, or their impact on major complications. Our study, which includes the largest retrospective cohort in the literature, was designed to investigate the effects of pigtail catheter application on major complications in patients with symptomatic, refractory MA when done with the correct indication and follow-up [8-11].
Material and methods
Inclusion and exclusion criteria
Between January 2017 and December 2022, patients with solid cancer diagnoses and diuretic-resistant symptomatic ascites, who had previously required at least one paracentesis, were included in the study. All patients were treated with pigtail peritoneal catheters in the Interventional Radiology Unit of our center.
Clinical and demographic data of the patients, relevant laboratory values, comorbid conditions, technical procedural success rates, complications occurring during and after the procedure, overall survival, and catheter dwell times were retrospectively collected from the patients’ medical oncology and interventional radiology records.
Patients were excluded from the study if they met any of the following criteria: catheter care training was not provided to at least one of the patient’s caregivers by the catheter care nurse; the palliative drainage indication for malignant ascites was given by a non-medical oncologist, such as a surgeon or internist; the catheter placement was not performed by an interventional radiologist; the patient was under 18 years old; the ascites was due to hematologic malignancy or non-malignant causes; or the patient was lost to follow-up after the procedure.
Pigtail peritoneal catheter application
In our study, pigtail peritoneal catheter applications were performed under ultrasound guidance by an interventional radiologist with at least 10 years of experience in the interventional radiology department of our center. Before and/or after the procedure, the catheter care nurse provided catheter care training to at least one of the patient’s caregivers. This training included detailed instructions on potential complications and when to consult a doctor. The intervention was performed percutaneously under ultrasound guidance using the Seldinger technique, targeting the area where the ascites level was most pronounced. At the drainage site, 1% lidocaine was injected subcutaneously. A 19-gauge Chiba needle was used to enter the peritoneal cavity. Once fluid was observed, a guidewire was advanced, and the needle was removed. After making a small incision in the skin, dilation was performed, and the pigtail catheter was placed into the abdomen under ultrasound guidance. The catheter was secured to the skin with sutures.
Definition of complications and technical procedural success
Complications were classified into major and minor categories based on the Society of Interventional Radiology Clinical Practice Guidelines [12]. Technical procedure success was defined as the correct placement of the catheter in the intraperitoneal position and the successful drainage of ascites following the procedure.
Data analysis
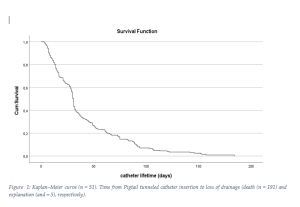
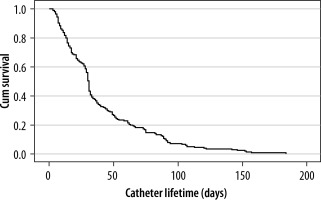
Data were analyzed using SPSS Statistics, version 27 (IBM Corp., Armonk, NY). The correlation between complication rates and other variables was assessed using Pearson’s c2 test, with statistical significance determined at a 95% confidence interval; p-values less than 0.05 were considered statistically significant. Catheter survival curves were created using the Kaplan-Meier method.
Results
Patient characteristics
Of the 196 patients included in the study, 102 (52%) were female. The median age was 66.5 years. The most common cause of ascites was gastric adenocarcinoma (n = 54), followed by colorectal adenocarcinoma (n = 33) and serous ovarian cancer (n = 22). Among comorbid conditions, hypertension was the most prevalent (n = 34), followed by diabetes mellitus (n = 24). Thirteen patients had impaired renal function tests, but none required renal replacement therapy. Among 10 patients with decreased ejection fraction on echocardiography performed within the last 3 months, none exhibited heart failure beyond stage 2. The majority of patients were in the terminal stage and receiving palliative care (best supportive care – BSC). Twenty-five patients were still receiving active cancer treatments, and due to these treatments, 12 patients had grade 1 anemia, and 10 patients had grade 1 neutropenia. General patient characteristics are shown in Table 1.
Table 1
General patient characteristics (N = 196)
Procedural success and complications
The technical procedural success rate was 100%. No procedure-related deaths or major complications (major bleeding, peritonitis) occurred. Out of 152 minor complications, the most common one was catheter blockage in 78 patients, which required catheter revision. Local cellulitis developed in 15 patients, only two of whom required oral antibiotic treatment, and recovery occurred without issues (Table 2). There was no statistically significant relationship between complication development and cancer type, comorbid conditions, age, or gender (p > 0.05). However, patients with comorbid conditions had a statistically significantly higher rate of complications (p = 0.042) (Table 3).
Table 2
Complications related to the procedure
| Factor | n | % |
|---|---|---|
| Major complications | 0 | 0 |
| Minor complications | ||
| Blockage | 78 | 39.8 |
| Cellulite | 15 | 7.7 |
| Leakage | 59 | 30.1 |
Catheter dwell time
The median catheter dwell time was 31 days (range: 3 to 184 days). There was no statistically significant relationship between catheter dwell time and cancer type, gender, or age (p > 0.05). The most common reason for catheter removal was death, followed by cessation of ascites production. Only 3 patients requested early removal of the catheter due to comfort concerns (Figure 1).
Discussion
Recurrent MA is a common clinical issue in patients with advanced cancer. Despite the availability of various medical and interventional treatment options, there is no standardized, evidence-based guideline for the management of malignant ascites. In our study, which represents the largest case series to date consisting entirely of patients with solid malignancies, our catheter placement success rate was 100%, consistent with the existing literature [4,8,13]. Considering that most patients in our study were in the terminal phase, the absence of procedurerelated mortality further confirms the safety of this method. Similarly, the zero rate of major complications, such as peritonitis, severe bleeding, and infections requiring intravenous antibiotics and/or hospitalization, supports the procedure’s safety. The lower rate of major complications compared to many other studies may be attributed to the fact that all patients included in the study had their catheter implantation indications jointly determined by a medical oncologist and an interventional radiologist, thus avoiding unnecessary and risky procedures [4]. On the other hand, our rate of minor complications, such as cellulitis, ascitic leakage, blockage, and catheter dysfunction, appears relatively high compared to similar studies in the literature; however, no minor complications progressed to major ones [8]. The sensitivity of our minor complication criteria may explain the high rate and the lack of progression to major complications due to early intervention.
As an alternative to pigtail peritoneal catheters, a PVS, such as the Denver shunt, can be considered. However, studies on this procedure are limited by small sample sizes, and major complications in these studies, such as pulmonary edema, pulmonary embolism, disseminated intravascular coagulation, and infection are reported at rates as high as 40% [14,15]. Furthermore, a mortality rate of over 30% directly related to the shunt procedure raises concerns about its safety [16]. Although there are no head-to-head prospective studies, it can be concluded that pigtail peritoneal catheters are safer and more effective than PV shunt procedures.
RLVP, frequently used in the treatment of malignant ascites, is the most significant alternative to pigtail peritoneal catheters [17]. The minimal invasiveness, effectiveness, safety, and easy accessibility of this method make it attractive [17]. However, cost-effectiveness studies have shown that pigtail peritoneal catheters are more costeffective than RLVP in both malignant and non-malignant ascites cases [18-20]. Studies have also been conducted on tumor-targeted therapies in the treatment of malignant ascites. Although intraperitoneal administration of hyperthermic chemotherapy and monoclonal antibodies such as bevacizumab and catumaxomab has shown promise in treating malignant ascites, particularly associated with ovarian cancer, these approaches have not yet become standard clinical practice [6,7,21].
A review of the literature reveals that the median catheter dwell time ranges from 23 to 113 days, with significant heterogeneity [8,10,22-24]. This heterogeneity is also evident within studies, with wide variations in minimum and maximum dwell times. Our study’s median catheter dwell time of 31 days is consistent with the literature. The catheter dwell time in our study ranged from 3 to 181 days and, as in the literature, it was heterogeneously distributed. The most plausible explanations for these heterogeneities are the differences in study designs and the inclusion of cases with different tumor types and varying treatment characteristics.
The main limitation of our study is that it is a retrospective, single-center cohort study. Additionally, the lack of evaluation of changes in symptoms, quality of life, and the need for paracentesis before and after the procedure is another limitation. There is a need for prospective studies with larger patient populations that compare the methods used in the treatment of malignant ascites. However, the most significant strength of our study is that it presents a relatively homogeneous and large cohort consisting entirely of refractory ascites cases due to solid malignancies, which contrasts with the more diverse populations often found in the literature.
Conclusions
The pigtail peritoneal catheter placement procedure emerges as an easily applicable method in experienced centers for the palliative treatment of refractory ascites in end-stage cancer patients. The high technical success rate, coupled with precise indications, thorough patient and caregiver education, and effective monitoring, contribute to its safety and efficacy.