Introduction
Perianal fistula is disease characterized by an inflammatory process that results from anal gland infections creating an abnormal tract between the anal canal and the perianal skin [1]. It starts with a primary opening that may give rise to more than one secondary tracts. It is typified by a persistent, purulent discharge or cyclic pain during abscess reaccumulation, followed by intermittent, spontaneous decompression [2].
Although the prevalence of perianal fistula is 0.01%, which is not very common, it has a substantial morbidity rate [3]. Some fistulas have a high recurrence rate of about 25% to 30% [4]. Secondary tracts that are not detected during the operation are the main cause of fistula recurrence and therefore incomplete cure [5].
Patients eventually have surgery because medical therapy is of little value in treatment. The preoperative assessment directly affects the surgical outcome [6].
It is commonly known that the findings of magnetic resonance imaging (MRI) and proper characterization of fistula and its complications impact the surgical approach and reduce the recurrence rate [7,8].
Fistula type, extent, and co-existing pathologies together with the radiological classification based on MRI findings are significant factors. Consequently, the appropriate medical treatment and surgical procedures should be planned accurately by the treating physician, encouraging total healing and eventually reducing the recurrence rate [9].
Although various imaging modalities such as fistulography and endo-cavitary ultrasonography have been employed to assess perianal fistulas, MRI continues to be the modality of choice. It has been determined that T2-weighted (T2-W) MRI sequences are the best sequences for obtaining a thorough anatomical view of the pelvis for evaluation of the anal canal. Additionally, these sequences enable the evaluation of perianal fistulas [10]. Unfortunately, T2-weighted (T2-W) MRI sequences are susceptible to motion artifacts associated with intestinal and respiratory motion and vascular pulsation that degrades the images and can obscure important findings [11].
Newly developed three-dimensional (3D) MRI sequences provide high soft tissue contrast. They gather information in an isotropic voxel format, resulting in multiplanar reconstruction images of superior quality. These sequences help to provide images in different axial, coronal and sagittal planes. As reformatting datasets can be done in any orientations, these sequences have the benefits of better image analysis and reduced imaging time [12].
These sequences such as 3D VISTA in Philips (Volume ISotopic Turbo spin echo Acquisition), provide near isotropic resolution and high image quality as they acquire thin slices without slice-to-slice gaps to obtain multiplanar image reformatting with high spatial resolution, enabling better anatomical structures analysis with short acquisition times [13,14].
The aim of the study was to determine the diagnostic performance of the new 3D MRI sequence VISTA, in depiction and characterization of perianal fistula compared with the routinely used T2 TSE pulse sequence with (CE) 3D T1 sequence THRIVE (T1-weighted high-resolution isotropic volume examination) as the standard reference.
Material and methods
Patients
This prospective study was approved by the institutional review board (IRB) and written informed consent was taken from all patients before the MRI examinations. Between January 2021 and August 2022, 40 patients who underwent MR examination were included in our study according to the following inclusion criteria: patients who had presented to our hospital with perianal tenderness, fever, pain, discharge and redness; their examination findings obtained by the outpatient clinic surgeon were consistent with the presence of perianal fistula. Ten patients were excluded, and exclusion criteria were: patients who had previous history of perianal fistula surgery within the last three months, patients who had contraindications for MRI examination such as pacemaker history, and claustrophobic patients. Finally, 40 adult patients (26 males and 14 females) with a mean age of 32 years (range 18-57 years) were included in our study. Patient symptoms and information were noted by a radiologist before the MRI examinations.
Magnetic resonance imaging
MRI examinations of the perianal region were done using a 1.5 tesla scanner (Ingenia; Philips Medical Systems; Best, The Netherlands) and a transmit/receive body coil; patients were in a supine position. T2 TSE and contrast-enhanced (CE) 3D T1 THRIVE sequences with addition of the new 3D MRI VISTA sequences were obtained. As there is forward tilt in the anal canal, the scan extent and field of view were obtained using a sagittal T2 TSS image while the central line was parallel with the anal canal, then coronal and axial images were obtained in relation to this central longitudinal axis of the anal canal. VISTA is a 3D sequence added to the previously routinely used T2 TSE and (CE) 3D THRIVE (Table 1 shows sequences parameters).
Table 1
Magnetic resonance imaging pulse sequences used in this study
Assessment of magnetic resonance images
After conducting MRI examination for all patients, images obtained from MRI examination were studied and compared by two radiologists with body imaging experience separately and independently with no clinical information provided by the referral surgeon. The radiologist (reader 1) with 12 years’ experience in body imaging assessed the perianal region for the presence of perianal fistula, its type (Table 2) [15], and its grade (Table 3) [16], and the presence of any associated complications such as abscess on MR images while the other radiologist (reader 2) with 10 years’ experience in body imaging assessed the MR images of the perianal region to test the inter-reader reliability.
Table 2
Park’s classification of perianal fistula [15]
Table 3
St. James’s University Hospital MRI classification system [16]
Images were assessed by the two radiologists and compared regarding the images’ quality and visibility of the anatomical details of the perianal region and perianal fistula. A three-point scale was used for the degree of visibility and clarity of anatomical details. Some structures were used as a refence, such as the levator ani muscle, the anal sphincter, ischioanal and ischiorectal fossa. This scale scores from 1 to 3 as follows: 1 – blurred (not well visualized), 2 – acceptable and 3 – excellent. Also, another five-point scale was used for presence and degree of artifacts; this scale scores from 1 to 5 as follow: 1 – marked artifacts, 2 – moderate, 3 – mild, 4 – minimal, and 5 – no artifacts. The results were considered a false negative result if there was under-scoring and a false positive result if there was over-scoring.
Then comparison between T2 FSE and 3D VISTA sequences was done for the depiction and characterization of perianal fistula using (CE) 3D T1 sequence THRIVE as a reference. Each sequence sensitivity, specificity and accuracy were calculated by both readers.
Statistical analysis
The sensitivity, specificity, and accuracy of 3D VISTA and T2 FSE sequences were calculated for both readers with CE 3D THRIVE sequences as a standard of reference. Values were calculated for depiction and characterization of perianal fistula, and multiple comparisons for the sensitivity, specificity, and accuracy differences were performed using Cochran’s Q. Cohen’s κ test was used to assess the inter-reader reliability of positive findings and κ statistics were conducted according to Landis and Koch [17]. The inter-reader agreement for perianal fistula classification, site of the internal opening, and presence of perianal abscess was evaluated.
Statistically significant p-values were considered to be p-values < 0.05 and analysis was performed using the software package SPSS Statistics 19.0 and 24.0.
Results
The mean age of the patients in the study was 32 years (range, 18-57 years) with mean duration of perianal symptoms such as pain and discharge of 1 year and 2 months (range, 7 months to 3 years).
A total of 40 perianal region MRI studies from patients had perianal symptoms. The sensitivity and accuracy of 3D VISTA for depiction and characterization of perianal fistula were higher than those of T2 TSE, while regarding specificity no statistically significant differences were found between the two pulse sequences (all p < 0.05).
The presence of abscesses was identified in 12 patients out of 40 and the remaining 28 patients did not have any abscesses. Also branching fistula was detected in only 5 patients out of 40 and 35 patients did not have any complex or branching fistula. The presence of abscesses and branching fistula was detected in all three sequences.
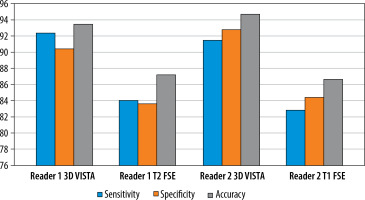
Accuracy, sensitivity, and specificity of 3D VISTA and T2 TSE MRI sequences are summarized in Table 4. The diagnostic sensitivity, specificity and accuracy of 3D VISTA were higher than those of T2 TSE: for reader 1, sensitivity 92.5% vs. 84.1%, specificity 90.5% vs. 83.9%, and accuracy 93.6% vs. 87.3%; and for reader 2, sensitivity 91.5% vs. 82.9%, specificity 92.8% vs. 84.5%, and accuracy 94.8% vs. 86.7%.
Table 4
Sensitivity, specificity and accuracy for 3D VISTA and T2 FSE in detection and characterization of perianal fistula
| 3D VISTA | 2 FSE | p-value | |
|---|---|---|---|
| Sensitivity (reader 1) | 92.5% | 84.1% | 0.004* |
| Specificity (reader 1) | 90.5% | 83.7% | – |
| Accuracy (reader 1) | 93.6% | 87.3% | 0.003* |
| Sensitivity (reader 2) | 91.5% | 82.9% | – |
| Specificity (reader 2) | 92.8% | 84.5% | 0.003* |
| Accuracy (reader 2) | 94.8% | 86.7% | –0.002* |
Discussion
MRI is a valuable tool in improving the outcome of perianal fistula surgery because it can show the pelvic structures anatomy, the primary fistula tract, secondary extensions and whether there are hidden areas of sepsis or abscesses [18,19].
T2-WI sequences play an important role in MRI in detection and characterization of perianal fistula. However, they are liable to more motion artifacts because they have a long acquisition time [11].
Advances in 3D MRI sequences enabled high spatial resolution isotropic 3D data acquisition, which is crucial for mapping perianal fistulas’ depiction and characterization. Compared to 2D sequences, the primary benefits of 3D sequences include operator independence, increased signal-to-noise ratio (SNR) attained with shorter imaging times, coverage of a larger area with thinner sections without intersection gaps, and free slab positioning. Every manufacturer has its own 3D sequences, including Philips (THRIVE, VISTA), GE (LAVA), and Siemens (VIBE, SPACE) [19,20].
The 3D VISTA sequence uses parallel imaging techniques to make up for the shortcomings of the 2D T2 sequence. These sequences employ a long echo time (TE) and a small flip angle, and as a result there is an increase in signal to noise ratio [14]. The 3D VISTA sequence shows promise in reducing motion artifacts that mask significant imaging findings and in shortening patient time in the MRI scanner bed [21].
In this study we compared a 3D MR technique (VISTA) with the routinely used T2-TSE sequences, using contrast-enhanced 3D (THRIVE) sequences as the standard reference for the depiction and characterization of perianal fistula.
We found that 3D VISTA sequences had higher sensitivity for depiction and characterization of perianal fistula than those of T2 TSE without a decrease in specificity or accuracy. When we compared the use of 3D VISTA sequences and T2-W TSE sequences in patients who had a perianal fistula we found that 3D VISTA produced images with clearer anatomical visualization and with fewer artifacts, resulting in higher image quality (Figures 1-3). In addition, it shortened the imaging duration, which helped to maintain patient comfort in a short scan.
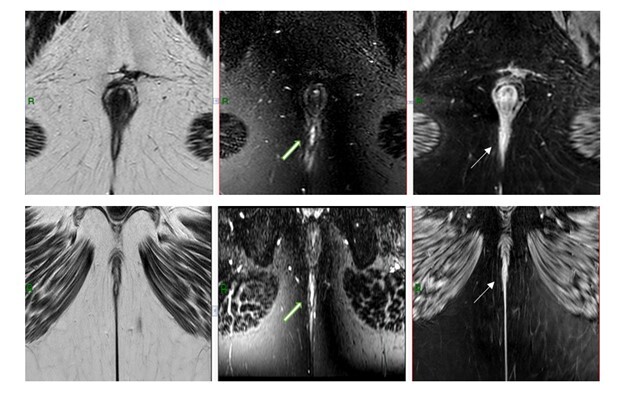
Figure 1
38-year-old male patient with severe perianal pain associated with purulent discharge with MRI of the perianal region. Each row represents T2 TSE, 3D VISTA and CE 3D THRIVE respectively, first row axial images and second row coronal images. There is a non-branching fistulous tract seen extending from the posterior subcutaneous soft tissue upward and piercing the posterior aspect of the external anal sphincter to the inter-sphincteric space then abutting the internal anal sphincter at 6 o’clock, with no abscess or collections. This tract is not clearly seen in T2 TSE and well depicted in 3D THRIVE images (open arrow) and in CE 3 D THRIVE images (arrows)
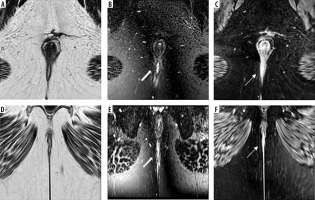
Figure 2
42-year-old female patient with perianal pain with MRI of the perianal region. Images represent axial T2 TSE, 3 D VISTA and CE 3D THRIVE respectively. Narrow, non-branching fistulous tract seen extending from the left perianal subcutaneous tissue and extending, piercing the posterior aspect of the external anal sphincter to end in the inter-sphincteric space at 6 o’clock, with no abscess or collections. This tract is not clearly seen in T2 TSE and well depicted in 3D THRIVE images (open arrow) and in CE 3 D THRIVE images (arrows)

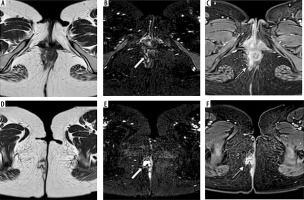
Figure 3
24-year-old male patient with Crohn disease and perianal pain with MRI of the perianal region. Each row represents axial T2 TSE, 3 D VISTA and CE 3D THRIVE respectively, first row axial images at the level of internal anal sphincter and second row just below this level. The right-branching interhemispheric fistulous tract is identified. It has three external opening at the right side, one posterior at 6 and 7 o’clock with multilocular abscess. The fistula then extends anterosuperiorly; it is seen branching in the inter-sphincteric space with an internal opening at 11 o’clock with small abscess collection. These branching fistulous tracts and abscess are not clearly seen in T2 TSE and well depicted in 3D THRIVE images (open arrow) and in CE 3 D THRIVE images (arrows)
In our study we used the CE 3D THRIVE sequence as the standard reference as a common finding from studies of various designs is that CE 3D T1 sequences have a higher accuracy than CE 2D T1WI sequences when evaluating perianal fistulas, whether simple or complex fistulous tracts.
A prior study revealed that recently used novel MRI sequences such as VIBE and THRIVE sequences, which are 3D T1 FAT SAT sequences, result in thinner image slices, which leads to a high spatial resolution in depiction of tissue abnormalities in soft tissue and cartilage [22].
In our study, regarding the sensitivity of the two sequences, the 3D VISTA sequence was higher than T2 TSE as it was 92.5% in 3D VISTA and 84.1% in T2 TSE for one reader and 91.5% in 3D VISTA and 82.9 % in T2 TSE for the other reader. Also, the specificity and accuracy of 3D VISTA were higher than those of T2 TSE as they were 90.5% and 93.6% respectively for one reader and 84.5% and 86.7% respectively for the other one (Figure 4).
Prior studies have evaluated the role of novel MRI sequences in evaluation of perianal fistula using MRI 3D sequences. Sahnan et al. [23] evaluated the role of these 3D MRI images and reported that with such images they could easily reveal the anatomy of complex fistulas by labeling the levator plate, the sphincter complex and the fistula.
In this study, the supra-levator region was clearly visible using the 3D VISTA sequence, particularly in coronal plane images. Better image quality with lack of endoanal coil application that cannot be tolerated by many patients and a short scan time would allow patient comfort during the preoperative assessment for perianal fistula.
Our study has a few limitations. Firstly, evaluation of the T2 TSE and 3D VISTA images was based on qualitative evaluation of the quality of the images with no quantitative measurements performed. Secondly, there was no comparison between the diagnostic performance of 3D VISTA and CE 3D THRIVE sequences in the current study. Further studies may be needed regarding that. Thirdly, diagnosis of fistula was made with reference to contrast-enhanced 3D THRIVE sequence images and without reference to surgery, as surgery was done for about 8 patients within 2 weeks of MRI. The remaining patients started antibiotics, and it was done outside the hospital. Due to low volume we could not depend on surgery results as a reference standard; instead we used CE 3D THRIVE, which is more accurate than CE 2D T1 sequences, and finally, only adult patients made up our patient sample. However, we speculate that the pediatric age group can gain benefit from the application of the 3D VISTA sequence as it ensures better image quality in a short scan time.
From the practical point of view, with its high diagnostic value and short scan time, it is highly recommended to add 3D VISTA sequences to the routinely used MRI protocol for perianal fistula, which routinely includes T2 and CE 3D T1 sequences, as that helps in better depiction and characterization of perianal fistula. 3D VISTA is a reasonable sequence for daily routine practice together with T2 TSE sequences.
Conclusions
3D VISTA sequences had higher diagnostic efficacy than the routinely used T2 TSE for depiction and characterization of perianal fistula. It offers significant advantages, such as a reduced imaging time and significantly reduces images artifacts, and it is clinically promising for the diagnosis of perianal fistulas. It is highly recommended to be added into the routinely used MRI protocol in such cases to improve the diagnostic sensitivity and accuracy, and that will help the treating surgeons in adjusting the best medical or surgical plan for those patients.