Introduction
Chylous ascites is a rare condition resulting from leakage of intestinal lymph from the lymphatic system. Iatrogenic chylous ascites caused by surgery is uncommon but difficult to treat in cases with unsuccessful conservative treatment [1]. Although conservative treatment has a high cure rate for mild chylous ascites, conservative treatment is often ineffective for chylous ascites with a higher drainage volume. Furthermore, the subsequent loss of protein, vitamins, and immunoglobulins may lead to cachexia, an impaired immune system, and sepsis, which may lead to higher perioperative mortality and poor prognosis [2]. Therefore, identifying an appropriate diagnostic and treatment approach for chylous ascites is crucial. This study explores the clinical value of intranodal lymphangiography in diagnosing and treating chylous ascites after abdominal surgery by reviewing patients with refractory chylous ascites after abdominal surgery.
Material and methods
Data collection
We collected clinical data from patients who were diagnosed with chylous ascites after undergoing surgery at Zhongshan Hospital, Fudan University, between January 2022 and November 2023, and who did not respond to conservative treatments such as a medium-chain triglyceride diet, total parenteral nutrition, and negative pressure drainage. The group consisted of 8 males and 2 females, aged 42-71 years, with an average age of 52. All were diagnosed with chylous ascites, with the following breakdown: 6 cases were due to partial hepatectomy, 3 cases from liver transplantation, and 1 from radical gastrectomy for gastric cancer. The primary lesions included intrahepatic cholangiocarcinoma (5 cases), hepatocellular carcinoma (3 cases), hepatic neuroendocrine carcinoma (1 case), and gastric adenocarcinoma (1 case). Prior to lymphangiography, chylous ascites persisted for a duration ranging from 7 to 118 days, during which all patients had abdominal drainage tubes inserted. The average daily drainage volume, as depicted in Table 1, ranged from 386 to 1802 ml. Inclusion criteria for patients were: 1) diagnosed with chylous ascites; 2) have undergone abdominal surgery; 3) ineffectiveness of conservative treatment. Exclusion criteria were: 1) allergy to iodized oil; 2) chylous ascites caused by non-surgical factors.
Table 1
Characteristics of each patient in whom lymphangiography was performed and the course of chylous leakage after lymphangiograph
Lymphangiography
Percutaneous lymphangiography was performed after obtaining informed consent from each patient. Bilateral inguinal lymph nodes were detected by ultrasound, and the puncture site was determined according to its size. Under ultrasound guidance, a 22 G puncture needle (YAKO Sangyo Co., Ltd. Japan) was used to puncture the central lymphatic vessels of inguinal lymph nodes. Depending on the patient’s condition, one side or both sides of the groin were injected with poppy iodinated oil injection (Jiangsu Hengrui Pharmaceuticals Co., Ltd.), with a total volume of no more than 10 ml. The upward flow of lipiodol was observed during the lymphangiography, and the location of lipiodol leakage was identified by lymphangiography or by post-lymphangiographic computed tomography.
Post-lymphangiographic follow-up
The basic situation of the patients, the amount of lipiodol used during the lymphangiography, the detection rate of lymphatic leakage on abdominal computed tomography (CT) images after lymphangiography, the time from the day of lymphangiography to the disappearance of chylous ascites, whether other surgical methods were performed after lymphangiography and the volume of chylous ascites per day after lymphangiography were followed up regularly. Intraoperative complications, such as allergic reactions to contrast agents and lipiodol, were recorded. Serious complications, such as alveolar hemorrhage, pulmonary vascular lipiodol embolism, cerebral infarction and other adverse reactions, were closely monitored. After discharge, patients were regularly checked for chylous ascites recurrence and the need for retreatment, as well as the effectiveness of such treatments.
Results
A total of 12 lymphangiographies were performed on 10 patients, one of whom experienced surgical treatment failure before lymphangiography. Among them, 2 patients (cases 6 and 8) underwent 2 lymphangiographies. Of the 12 lymphangiographies, 11 were technically successful. One attempt failed because the inguinal lymph nodes could not be detected again under ultrasound for puncture. Among the 11 successful procedures, in 10 cases it passed through the right inguinal lymph vessels, and in 1 case it passed through the bilateral inguinal lymph vessels.
One patient (case 10) had cardiac arrest about 2 days after surgery, and another (case 6) suffered a cerebral infarction 7 days after surgery. However, after careful discussion by an expert panel of neurologists, cardiologists, surgeons, interventional radiologists, and radiologists, these symptoms of the two patients were considered unrelated to lymphangiography. The average amount of iodized oil used was 4.5 ml, with individual doses in the range 3.5-7.0 ml.
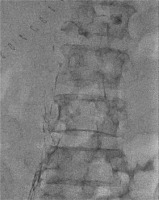
In three patients (cases 2, 5, and 9), the site of leakage was successfully identified during the lymphangiography. The remaining five patients (cases 3, 4, 6, 7 and 8) were not sought to find the leakage site during lymphangiography; however, after the completion of lymphangiography, they underwent abdominal CT scans, which successfully identified the leakage site. In another two patients, the site of leakage was not found through either lymphangiography or abdominal CT scans. Figure 1 shows the lymphangiography image of case 9, and Figure 2 shows the computed tomography image of case 5.
Figure 2
A) Computed tomography image of case 5 before lymphangiography. B) Computed tomography image of case 5 three days after angiography. C) Computed tomography image of case 5 eleven days after angiography
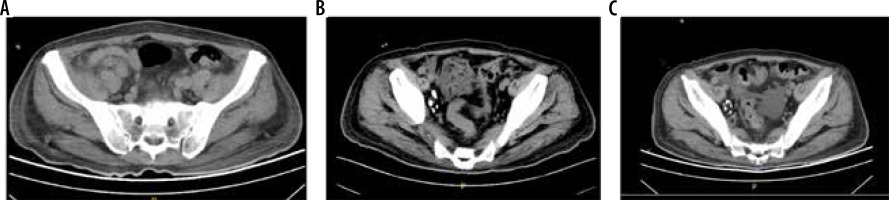
Six of the 10 patients (cases 1, 2, 4, 5, 6 and 9) had a significant reduction in daily drainage volume, and in 4 cases (cases 1, 2, 5 and 9) the chylous ascites resolved within 2 weeks. The drainage volume of the remaining 4 cases (cases 3, 7, 8, 10) did not change significantly. Eventually, cases 2 and 7 stopped having chylous ascites, and case 10 showed a temporary decrease in drainage volume but suffered respiratory and cardiac arrest two days after the procedure. Although resuscitated successfully, the patient developed septic shock, and relevant drainage data were lost. In case 8 chylous ascites has not stopped so far and relevant data were also lost because an attempt to clamp the drainage tube was made after lymphangiography failed to provide therapeutic benefit.
Discussion
Although the phenomenon of spontaneous healing of chylous ascites after lymphangiography was discovered in 2005 [3], it was previously carried out by pedal lymphangiography. With ultrasound-guided intranodal lymphangiography first proposed in 2011 [4], the limitations of previous pedal lymphangiography techniques were technically addressed, making lymphangiography more convenient and efficient [5]. In previous studies, the overall success rate of therapeutic lymphangiography in patients with failed conservative treatment was 51% [6]. The reason for the relief of chylous ascites after lymphangiography may be related to the hydrolysis and saponification of fat, the accumulation of lipiodol, the inflammatory reaction of lipiodol, and the high viscosity of lipiodol [6-9].
There are many reasons for development of chylous ascites. The underlying etiologies for chylous ascites have been classified as traumatic, congenital, infectious, neoplastic, postoperative, cirrhotic, or cardiogenic. Although malignancy and cirrhosis account for about two-thirds of all cases of CA in Western countries [10], lymphatic vessel damage and infection after abdominal surgery are also among the main causes in adults [11]. Patients with ascites caused by postoperative chylous leakage are often in a state of high energy expenditure and protein requirements due to traumatic stress (Figure 3). Chylous ascites may lead to decreased blood volume, malnutrition, and a compromised immune system, severely affecting post-operative recovery, prolonging the length of stay, and even increasing mortality [12]. It has been reported that the incidence of chylous ascites after liver transplantation is 0.6-4.7% [13] and the incidence of chylous ascites after oncological abdominal surgery is 7.4% [14]. Unlike many previous studies on chylous ascites, 10 patients in this study underwent abdominal surgery, and 90% of them underwent liver-related surgery. The reported therapeutic efficacy of lymphangiography for postoperative lymphatic leakage is 46-89% [6,7,15-18] according to relevant reports in the literature, which corresponds well to our 60% therapeutic success rate of observation following lymphangiography. However, a lower success rate was observed in liver transplantation, possibly due to higher rates of leakage and the complexity of surgical procedures. Therefore, we need to consider other treatment methods, such as platelet-rich plasma (PRP) and fibrin glue (FG) [19].
After the review by the expert panel, none of the 10 patients experienced lymphangiography-related complications. Although one patient had cardiac arrest two days after lymphangiography, this individual had low blood pressure beforehand and relevant bacteria were detected in the pleural effusion. At the same time, the relevant bacteria were detected in the pleural effusion before the lymphangiography. Therefore, after the discussion of the expert panel, they determined that the cardiac arrest was unrelated to lymphangiography. In another case, a second lymphangiography was performed 11 days after the first, with a new cerebral infarct appearing five days later. We did not find any signs of lipiodol-related cerebral infarction in the brain by careful comparison with previous head CT scans. Therefore, although two patients had unexpected symptoms during the perioperative period, we believe that lymphangiography is relatively safe. However, the number of lymphangiographies carried out globally is relatively small compared with other interventional procedures, so it is still necessary to be alert for the occurrence of related complications.
We also noted interesting phenomena such as the slow metabolism of lipiodol in lymphatic vessels, with residues remaining in lymph nodes for up to 17 months (Figure 4). Lipiodol not only ascends from the inguinal lymph nodes but also descends to the scrotum in some cases (Figure 5). Although our elderly patients no longer require fertility, the potential impact on reproductive function due to lipiodol deposition in scrotal lymph nodes remains unclear. This requires further study to understand the long-term effects of lipiodol residues in lymphangiography. In one case, a second lymphangiography was performed after the therapeutic failure of the first lymphangiography. The drainage volume was significantly reduced after the second lymphangiography, which proved that if the first lymphangiography failed therapeutically, the second lymphangiography could still be effective.
This single-center retrospective study had a limited sample size, underscoring the need for further systematic research to confirm the therapeutic efficacy of lymphangiography for postoperative chylous ascites.
Conclusions
Our study suggests that ultrasound-guided intranodal lymphangiography may aid in both the diagnosis and potential treatment of chylous ascites following abdominal surgery. For patients with chylous ascites unresponsive to conservative treatment, this procedure appears to be safe and has shown promise in clinical practice.