Introduction
In the last 50 years, the computed tomography (CT) scan has been increasingly used in Western countries [1]. This has been particularly evident in emergency departments (EDs), where CT is often used as the first imaging approach in patients with acute abdominal pain (AAP) in place of ultrasound (US) [2]. The sensitivity and specificity of abdominal CT for acute AAP is about 80-100%, but its use implies a significant ionizing radiation dose [2,3]. Therefore, it is of utmost importance to follow the Euratom radiation protection directive legislation DE 59/2013 [4] and the principles of optimization and justification before performing an abdominal CT scan, particularly in young patients.
In patients with AAP, CT outperforms US in terms of sensitivity (89% vs. 70%, respectively) for the diagnosis of the aetiology. However, due to radioprotection issues, US should be considered the first-line imaging approach in young patients, while CT should be performed only if strongly recommended [5,6]. Nowadays, as recently highlighted by Tonolini et al. [7], young adult patients are often exposed to follow-up CT imaging to monitor urogenital, intestinal, hepatobiliary, and pancreatic diseases that do not require surgical management and to assess post-surgical complications of abdominal emergencies. This results in an excessive ionizing radiation exposure, the long-term effects of which cannot be reliably predicted but may potentially result in an increased tumour burden or presentation of tumours at a younger age than now [8]. Therefore, the aim of this study was 3-fold.
The primary objective was to assess the frequency of appropriateness of CT for AAP in the Emergency Department.
The secondary aim was to compare the accuracy of US and CT in the diagnosis of the aetiology of AAP for disease whose diagnosis can be reached by US.
The third objective was to assess the extent to which inappropriate CT examinations for AAP result in ionizing radiation exposure.
Material and methods
This retrospective, single-institution study was conducted according to the criteria set by the declaration of Helsinki. The authors had control of the data and the information submitted for publication. There was no industry support for this study.
Study design and population
We retrospectively searched the departmental electronic database at our academic Institution for consecutive patients who underwent abdominal CT examinations between 1 January 2016 and 31 December 2016 and were referred for AAP by the Emergency Department. The search yielded an initial target population of 3364 consecutive patients who were deemed eligible for inclusion in the study. Then, we included patients aged between 15 and 46 years. Patients were then excluded if (i) aged 47 years or older (n = 2778); (ii) if the aetiology of AAP was traumatic (n = 69), neoplastic (n = 59), or vascular (n = 8); or (iii) if clinical data were incomplete or not available (n = 6). In addition, patients examined with other scan apparatus (in the case of maintenance or failure of the Emergency Department CT apparatus) were excluded to reduce apparatus-related dose variability. We arbitrarily decided to exclude from the study population the incidental findings detected in CT examination, which may turn to “appropriate” some CT examination when performed for different reasons. Patients with repeated admittance in the Emergency Department with eventual repeated CT or US examinations were also excluded.
Of note, children younger than 15 years old are not admitted to our Emergency Department.
Data collection
By using our institution’s electronic data repository, the medical records of the patients included in the study were reviewed to assess patient information, US, and CT data. We collected patient-related variables (i.e. patient’s gender and age), clinical information (i.e. referral motivation, clinical indication, diagnosis at discharge, and/or diagnosis for emergency hospitalization), and imaging data (i.e. US and CT reports, and CTDI and DLP from CT dose report). All data were collected in a computerized database using Microsoft Office Excel 2007.
Ultrasound and computed tomography equipment
US exams were performed with 2 dedicated apparatus MyLab Twice (Esaote Biomedica, Genoa, Italy) or iU22 unit (Philips Ultrasound, Bothell, WA, USA), both provided with a multi-frequency convex array probe.
CT scans were performed with a 16-row multislice CT (Light-Speed 16, General Electric Medical System, Milwaukee, WI, USA, the dedicated CT apparatus of the Emergency Department). In 529 patients the performed examinations were non-contrast CT scans, whilst in 34 patients the examinations were performed before and after contrast media (CM) administration, with non-contrast phase and portal venous phase (performed 70 seconds after CM administration), using different CM brands (Ultra-vist® 370, Bayer SPA, Iomeron® 400, Bracco, Xenetix® 370, Guerbet).
Dose estimation
Estimated effective total dose and per-organ dose was calculated using CT-EXPO® software version 2.2 (Hannover, Germany). This software provides estimates of effective dose, doses to the other organs, and values of DLP (dose-length product) and CTDI (CT dose index). This software uses as input various acquisition parameters such as the tension (kV), current (mA), duration of the exam, pitch, collimation, part of body exposed, and patient gender. To estimate the effective dose (i.e. kscanner x DLP), we used the DLP of each exam and the k scanner obtained through the CT-EXPO® software. Of note, this software estimates doses on standard “models” of male and female patients. Because real patients do not match exactly the features (in terms of weight and height) of standard patients the dose values obtained through this analysis are only estimates of the real doses absorbed by patients.
Statistical analyses
Patients’ demographic, histological, and imaging data were reported in an Excel document (Microsoft Corp., Redmond, WA). Summary statistics are presented as mean for continuous measures while binary variables were summarized as frequency (n) and percentages (%).
First, we compared clinical suspicion and CT imaging findings with appropriateness criteria according to Iguide® to investigate whether indication of CT examinations for AAP was crucial, possibly appropriate, or inappropriate. The appropriateness ranking scale is an ordinal scale that uses numbers from 1-9, grouped into 3 categories: usually not appropriate – 1, 2, or 3; may be appropriate – 4, 5, or 6; and usually appropriate – 7, 8, or 9 (Table 1).
Table 1
Score of appropriateness according to IGuide (ESR iGuide 2017)
Second, we measured and compared the sensitivity of US and CT for the identification of the aetiology of AAP for diseases whose diagnosis can be reached by US. For this analysis, we first excluded 96 patient who had undergone CT but not US examination, or US only, and then we selected patients (n = 152) whose diagnosis could potentially be reached only by US but who underwent CT scan after US.
Third, we recorded the mean CTDIvol and DLP and measured the ED. The mean ED was calculated with the 75th percentile of the total DLP using is the tissue sensitivity factors.
We first evaluated ionizing radiation exposure based on the aetiology of AAP, and then specifically in the cohort of patients inappropriately submitted to CT. Thereafter, we divided the study population into 3 different age groups (from 15 to 26 years old, from 27 to 36 years old, and from 37 to 45 years old) based on radiation sensitivity, and we evaluated the burden of exposure for these 3 groups based on gender.
Results
Patient population
Our final study population consisted of 586 patients aged between 15 to 46 years (mean age: 31.7 years), who were submitted to abdominal CT exams in the Emergency Department in 2016, including 309 men and 277 women. The characteristics of the study population, including patient-related variables, clinical information, and imaging data, are summarized in Figure 1.
Appropriateness of computed tomography for acute abdominal pain
According to appropriateness criteria of Iguide [6] and based on the clinical suspicion of CT requests, CT examination was considered crucial in 264 (45.05%) of patients. 322 patients had a referral reason for the CT scan that could be considered “possibly appropriate” according to Iguide criteria (4, 5, 6 scoring) [6]. Of these, 135 had an inappropriate CT request according to images findings, whilst 187 had an appropriate request based on CT findings (i.e appendicitis in acute right flank pain).
Diagnostic accuracy of ultrasound and computed tomography
We analysed the clinical suspicions of all the 586 patients and noted that even if in 152 of them the diagnosis could be performed using US: urolithiasis (n = 79), non-complicated appendicitis (n = 38), non-complicated Crohn’s disease (n = 19), cholelithiasis (n = 5), and symptomatic adnexal masses (n = 11), only in 84 patients, was this technique performed prior to CT, and the aetiologies of AAP were urolithiasis and cholelithiasis.
Among 79 patients with urolithiasis, 40 (50.6%) lacked hydroureteronephrosis or showed only type I hydroure-teronephrosis, while 39 (49.4%) had type II-IV hydroure-teronephrosis. In these 2 groups of patients, US failed to detect the obstructing urinary stones in 18 (45%) of 40 patients and in 11 (28.2%) of 39 patients, respectively.
Among 5 patients with cholelithiasis, all had biliary tract lithiasis associated with and thickened gallbladder walls and free fluids, who underwent CT in order to evaluate any other associated conditions such as acute cholecystitis, bilioenteric fistula, or pancreatitis. In none on these patients were the gallstones detected in the successive CT, due to the lack of calcific components within the calculus.
Ionizing radiation exposure
The mean ED was calculated with the 75th percentile of the total DLP using is the tissue sensitivity factors (Table 2) [7,8].
Table 2
Effective dose calculated using computed tomography dose Expo considering tissue conversion factor in the different subgroups
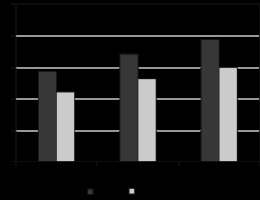
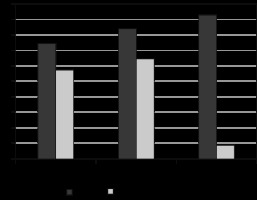
Data on ionizing radiation exposure based on gender and age showed that in 277 of 586 women, the estimated mean ED was 11.1 ± 5.2 mSv in the 99 patients aged from 15 to 26 years, 13.2 ± 8.7 mSv in the 86 patients aged from 27 to 36 years, and 15.0 ± 9.7 mSv in the remaining 92 patients aged from 37 to 45 years (Figure 2); in 309 of 586 men the estimated mean ED was 11.5 ± 11.9 mSv in the 96 patients aged from 15 to 26 years, 12.9 ± 9.9 mSv in the 109 patients aged from 27 to 36 years, and 14.2 ± 11.5 mSv in the remaining 104 patients aged from 37 to 45 years (Figure 3).
Discussion
CT scan rates have increased significantly in the last 2 decades, in the general population and in young patients, due to higher availability and greater efficiency of available CT technologies, especially in emergency situations [9].
A significant change has occurred in recent years, with a plateau forming around 2008, at which point there was a significant reduction in the use of CT in favour of equally diagnostic and potentially less harmful methods such as US or MR [10].
While this increased availability of advanced imaging has been associated with improved patient outcomes for some diseases, there are growing concerns about the possibility of inappropriate utilization of imaging because of its potential contribution to general population radiation exposure [8,10].
Our study was conducted with the aim of evaluating the rate of appropriateness of abdominal CT scans performed for AAP in the Emergency Department and comparing relative findings with alternative imaging tools, such as US, especially in young patients.
Young adult patients were considered in our court as younger 46 years old, admitted for AAP in the Accident and Emergency Department of the Polyclinic Hospital Paolo Giaccone.
In routine clinical practice, for AAP referred to the Accident and Emergency Department, the first requested diagnostic examination was CT scan, even in young patients, and even if the diagnosis could have been reached using US, according to Iguide®.
For every patient included in our dataset, we compared the referral diseases with the most appropriate dia-gnostic tool according to the Iguide® guidelines [6] based on ACR appropriateness criteria.
The overall analysis of patients whose diagnosis could be potentially performed through US (i.e. uncomplicated appendicitis, urolithiasis, Crohn’s disease, cholelithiasis, or symptomatic adnexal masses) gave as a result 152 patients, and showed that only in 55.2% of the patients had a US study been performed prior to CT, and of note all of them were referred for urolithiasis or cholelithiasis only.
US has a variable sensibility (44-98%) and specificity (47-95%) in appendicitis diagnosis [11], high sensibility (88%) and specificity (80%) in cholecystitis [12], and variable sensibility (12-93%) in urolithiasis [13,14], because of its reduced sensitivity in the identification of the ureteral stones. Indeed, in the case of suspected urolithiasis, even if US has poor sensitivity in the detection of ureteral stones and can potentially be substituted by CT in these cases, it can easily confirm the presence of associated hydroureteronephrosis. This could also explain why the sub-group of patients with urolithiasis were more frequently submitted to US prior to CT scan.
Inflammatory bowel diseases (IBD), and particularly Crohn’s disease (CD) patients, are often referred to EDs not because of the disease itself but because of intestinal complications. They often undergo CT examinations without any abdominal ultrasound performed, but as some studies have shown that [15,16], ultrasound represents a valid radiological examination for the detection of indirect sign of complications and, in selected cases, for follow-up, especially in young patients [15-18]. But the detection of the complication itself requires a CT scan; indeed, the most common complication of CD is stricture. US sensitivity in detecting small bowel stenosis is about 79%, while the specificity is 92% [18]; CT enterography (CTE) sensitivity for stenosis detection is estimated at 92% and specificity at 100% [19].
US can provide useful information in 56-65% of patients with acute abdominal pain, but it has some intrinsic limitations that are not included in this retrospective analysis, and thus in some cases CT imaging assessment may be required. Among the main limitations of US, the most important are the operator dependency, poor or absent patient collaboration, presence of artefacts, and/or constitutional habitus of the patient (overweight patients) [20,21].
In our study, of the 586 patients taken into consideration, in 264 patients the CT referral reason was crucial according to Iguide® and therefore proved to be significant for the final diagnosis.
In 322 patients, the defined appropriateness was “possible”, but in 58% of cases (187 patients), despite CT has not confirmed the proposed referral reason, had an appropriate request based on the CT findings, whilst in 135, they had an inappropriate CT request according to images findings (i.e. renal colic in patient without detected stone in CT).
These data are of particular concern if we consider that our study was performed just in patients younger than 46 years old, who represent a possible “sensible population”.
The harmful effects of ionizing radiation are widely recognized. Greater radiation sensitivity has been reported for young adults and particularly for the female population [8,22]. However, the specific negative effects of radiation especially at low doses such as those used in routine X-ray diagnostics are the subject of great controversy [22,23].
Computed tomography (CT) represents about 9% of all radiological exams, but it is responsible for 47% of the total dose of medical radiation [22]. According to Raja et al., the intensity of abdominal imaging, measured as the number of abdominal imaging studies performed per 1000 ED visits, increased significantly during their 20-year study period. However, the imaging modality of choice has changed, as CT replaced X-ray as the preferred method of imaging the abdomen in emergency patients [10]. Their results clearly confirm ours; in our institution, CT has become the predominant method of imaging ED patients. It should be the focus of future studies to help guide evidence-based strategies for abdominal imaging, especially in ED patients.
Radiation protection is governed by the European Council Directive 97/43/Euratom, Ionizing Radiotherapy Regulation (Medical Exposure) 2000 (IRMER) based on the use of radiation-based methods used on the principle of “as low as reasonably achievable” (ALARA) [24], i.e. every radiation exposure must be kept as low as reasonably achievable on the basis of both economic and social considerations.
The principle’s implication is of paramount importance in cases where exposure limits are not defined on the basis of a threshold, but on the basis of an ‘acceptable risk’ (that could be accepted if the clinical indication is appropriate and the CT scan result has an impact on patient treatment).
The potential risk that ionizing radiation can cause to patients suffering from recurring diseases (such as urolithiasis or chronic intestinal diseases), especially if young, who undergo repeated CT investigations, raises many concerns [25]. Indeed, the scientific community agrees that there is a risk to public health for this kind of patient, even minimal, given the large amount of CT surveys that are carried out every year [26].
Patient history, clinical symptoms and laboratory exams should guide clinicians and radiologists in choosing the correct examination. The appropriate choice of imaging examination has potentially different impacts: it could reduce ionizing radiation exposure and the waste of economic and time resources.
Nevertheless, we must consider that the results of our study have the potential limitation of the impossibility of finding crucial information such as patients’ BMI, because it is a retrospective study. BMI indeed affects US examinations, because overweight patients are difficult to examine, and CT scans because the administered dose is related to the patient’s size.
The ionizing radiation dose (IRD) from CT imaging is expressed in terms of effective dose (ED), which corresponds to the sum of the individual doses to each exposed organ multiplied by organ-specific weighting factors, and it is commonly used as a convenient way to compare different exposures.
Other dose descriptors in CT scans are the volume CT dose index (CTDI volume), which is the average dose within a scan volume relative to a standardized CT phantom, and the dose length product (DLP), which is the integrated dose along the scanned region and is equal to the CTDI volume multiplied by the scan length in centimetres [27-29] measured according to the European guidelines on quality criteria for CT (EUR16262) [30].
Other limitations of this study include the following: the study population was not randomized and possibly for rare diseases it is difficult to understand the impact of CT in patient management.
Although the use of radiological investigation is often justified by clinical benefits for the patients, in order to counterbalance the modest risk due to radiation, it should be remembered than even the smallest dose of radiation is not entirely without risk.
Because of our inclusion criteria, our results may represent only “the tip of the iceberg” of the CT exposure problems in EDs.
Conclusions
The use of CT for abdominal pain has increased particularly in the EDs. This increase is due to the high specificity and sensibility of CT in the diagnosis of the pathologies responsible for acute abdomen [30,31] and the rapid time of scan acquisition, resulting in a prompt therapy whenever needed. Well-orchestrated strategies are needed to reduce unnecessary diagnostic imaging. A fundamental question is whether these strategies work and how best to determine whether they do without compromising patient well-being [32].
CT has changed the therapeutic approach, addressing patients directly to the correct medical or surgical treatment [33-35], but it should be used only according to guidelines.