HEAD AND NECK RADIOLOGY / ORIGINAL PAPER
Assessing the accuracy of artificial intelligence in mandibular canal segmentation compared to semi-automatic segmentation on cone-beam computed tomography images
1
Department of Diagnostics, Chair of Practical Clinical Dentistry, Poznan University of Medical Sciences, Poznan, Poland
2
Doctoral School, Poznan University of Medical Sciences, Poznan, Poland
3
Kazimierczak Private Medical Practice, Bydgoszcz, Poland
4
Neuro Musculo Skeletal Lab (NMSK), Institut de Recherche Expérimentale et Clinique (IREC), Université Catholique de Louvain (UCLouvain), 1200 Brussels, Belgium
5
Oral and Maxillofacial Surgery Lab (OMFS Lab), NMSK, IREC, Université Catholique de Louvain (UCLouvain), 1200 Brussels, Belgium
6
Department of Oral and Maxillofacial Surgery, Cliniques Universitaires Saint-Luc, 1200 Brussels, Belgium
7
Department of Perioperative Dentistry, L. Rydygiera Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
These authors had equal contribution to this work
Submission date: 2025-02-25
Final revision date: 2025-02-28
Acceptance date: 2025-03-01
Publication date: 2025-04-10
Corresponding author
Julien Issa
Department of Diagnostics, Chair of Practical Clinical Dentistry, Poznan University of Medical Sciences, 70 Bukowska St., 60-812 Poznan, Poland
Department of Diagnostics, Chair of Practical Clinical Dentistry, Poznan University of Medical Sciences, 70 Bukowska St., 60-812 Poznan, Poland
Pol J Radiol, 2025; 90: 172-179
KEYWORDS
TOPICS
ABSTRACT
Purpose:
This study aims to assess the accuracy of artificial intelligence (AI) in mandibular canal (MC) segmentation on cone-beam computed tomography (CBCT) compared to semi-automatic segmentation. The impact of third molar status (absent, erupted, impacted) on AI performance was also evaluated.
Material and methods:
A total of 150 CBCT scans (300 MCs) were retrospectively analysed. Semi-automatic MC segmentation was performed by experts using Romexis software, serving as the reference standard. AI-based segmentation was conducted using Diagnocat, an AI-driven cloud-based platform. Three-dimensional segmentation accuracy was assessed by comparing AI and semi-automatic segmentations through surface-to-surface distance metrics in Cloud Compare software. Statistical analyses included the intraclass correlation coefficient (ICC) for inter- and intra-rater reliability, Kruskal-Wallis tests for group comparisons, and Mann-Whitney U tests for post-hoc analyses.
Results:
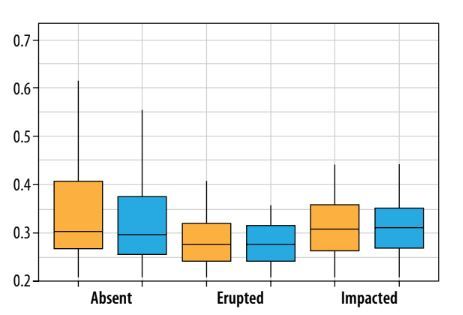
The median deviation between AI and semi-automatic MC segmentation was 0.29 mm (SD: 0.25-0.37 mm), with 88% of cases within the clinically acceptable limit (≤ 0.50 mm). Inter-rater reliability for semi-automatic segmentation was 84.5%, while intra-rater reliability reached 95.5%. AI segmentation demonstrated the highest accuracy in scans without third molars (median deviation: 0.27 mm), followed by erupted third molars (0.28 mm) and impacted third molars (0.32 mm).
Conclusions:
AI demonstrated high accuracy in MC segmentation, closely matching expert-guided semi-automatic segmentation. However, segmentation errors were more frequent in cases with impacted third molars, probably due to anatomical complexity. Further optimisation of AI models using diverse training datasets and multi-centre validation is recommended to enhance reliability in complex cases.
This study aims to assess the accuracy of artificial intelligence (AI) in mandibular canal (MC) segmentation on cone-beam computed tomography (CBCT) compared to semi-automatic segmentation. The impact of third molar status (absent, erupted, impacted) on AI performance was also evaluated.
Material and methods:
A total of 150 CBCT scans (300 MCs) were retrospectively analysed. Semi-automatic MC segmentation was performed by experts using Romexis software, serving as the reference standard. AI-based segmentation was conducted using Diagnocat, an AI-driven cloud-based platform. Three-dimensional segmentation accuracy was assessed by comparing AI and semi-automatic segmentations through surface-to-surface distance metrics in Cloud Compare software. Statistical analyses included the intraclass correlation coefficient (ICC) for inter- and intra-rater reliability, Kruskal-Wallis tests for group comparisons, and Mann-Whitney U tests for post-hoc analyses.
Results:
The median deviation between AI and semi-automatic MC segmentation was 0.29 mm (SD: 0.25-0.37 mm), with 88% of cases within the clinically acceptable limit (≤ 0.50 mm). Inter-rater reliability for semi-automatic segmentation was 84.5%, while intra-rater reliability reached 95.5%. AI segmentation demonstrated the highest accuracy in scans without third molars (median deviation: 0.27 mm), followed by erupted third molars (0.28 mm) and impacted third molars (0.32 mm).
Conclusions:
AI demonstrated high accuracy in MC segmentation, closely matching expert-guided semi-automatic segmentation. However, segmentation errors were more frequent in cases with impacted third molars, probably due to anatomical complexity. Further optimisation of AI models using diverse training datasets and multi-centre validation is recommended to enhance reliability in complex cases.
REFERENCES (35)
1.
Carter JB, Stone JD, Clark RS, Mercer JE. Applications of cone-beam computed tomography in oral and maxillofacial surgery: an overview of published indications and clinical usage in United States academic centers and oral and maxillofacial surgery practices. J Oral Maxillofac Surg 2016; 74: 668-679.
2.
Schulze RKW, Drage NA. Cone-beam computed tomography and its applications in dental and maxillofacial radiology. Clin Radiol 2020; 75: 647-657.
3.
Kaasalainen T, Ekholm M, Siiskonen T, Kortesniemi M. Dental cone beam CT: an updated review. Phys Med 2021; 88: 193-217.
4.
Agbaje JO, de Casteele EV, Salem AS, Anumendem D, Lambrichts I, Politis C. Tracking of the inferior alveolar nerve: its implication in surgical planning. Clin Oral Investig 2017; 21: 2213-2220.
5.
Shankland WE 2nd. The trigeminal nerve. Part IV: the mandibular division. Cranio 2001; 19: 153-161.
6.
Jacobs R, Quirynen M, Bornstein MM. Neurovascular disturbances after implant surgery. Periodontol 2000 2014; 66: 188-202.
7.
Sarikov R, Juodzbalys G. Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res 2014; 5: e1. DOI: 10.5037/jomr.2014.5401.
8.
Li Y, Ling Z, Zhang H, Xie H, Zhang P, Jiang H, Fu Y. Association of the inferior alveolar nerve position and nerve injury: a systematic review and meta-analysis. Healthcare (Basel) 2022; 10: 1782. DOI: 10.3390/healthcare10091782.
9.
Poort LJ, van Neck JW, van der Wal KG. Sensory testing of inferior alveolar nerve injuries: a review of methods used in prospective studies. J Oral Maxillofac Surg 2009; 67: 292-300.
10.
Li Y, Ling Z, Zhang H, Xie H, Zhang P, Jiang H, Fu Y. Association of the inferior alveolar nerve position and nerve injury: a systematic review and meta-analysis. Healthcare (Basel) 2022; 10: 1782. DOI: 10.3390/healthcare10091782.
11.
organ N, Meeus J, Shujaat S, Cortellini S, Bornstein MM, Jacobs R. CBCT for diagnostics, treatment planning and monitoring of sinus floor elevation procedures. Diagnostics (Basel) 2023; 13: 1684. DOI: 10.3390/diagnostics13101684.
12.
Xiang B, Lu J, Yu J. Evaluating tooth segmentation accuracy and time efficiency in CBCT images using artificial intelligence: a systematic review and meta-analysis. J Dent 2024; 146: 105064. DOI: 10.1016/j.jdent.2024.105064.
13.
Zheng Q, Gao Y, Zhou M, Li H, Lin J, Zhang W, Chen X. Semi or fully automatic tooth segmentation in CBCT images: a review. PeerJ Comput Sci 2024; 10: e1994. DOI: 10.7717/peerj-cs.1994.
14.
Najjar R. Redefining radiology: a review of artificial intelligence integration in medical imaging. Diagnostics (Basel) 2023; 13: 2760. DOI: 10.3390/diagnostics13172760.
15.
Waller J, O’Connor A, Rafaat E, Amireh A, Dempsey J, Martin C, Umair M. Applications and challenges of artificial intelligence in diagnostic and interventional radiology. Pol J Radiol 2022; 87: e113-e117. DOI: 10.5114/pjr.2022.113531.
16.
Abesi F, Jamali AS, Zamani M. Accuracy of artificial intelligence in the detection and segmentation of oral and maxillofacial structures using cone-beam computed tomography images: a systematic review and meta-analysis. Pol J Radiol 2023; 88: e256-e263. DOI: 10.5114/pjr.2023.127624.
17.
Naufal MF, Fatichah C, Astuti ER, Putra RH. Deep learning for mandibular canal segmentation in digital dental radiographs: a systematic literature review. IEEE Access 2024; 12: 76794-76815. DOI: 10.1109/ACCESS.2024.3406342.
18.
Issa J, Olszewski R, Dyszkiewicz-Konwińska M. The effectiveness of semi-automated and fully automatic segmentation for inferior alveolar canal localization on CBCT scans: a systematic review. Int J Environ Res Public Health 2022; 19: 560. DOI: 10.3390/ijerph19010560.
19.
Assiri HA, Hameed MS, Alqarni A, Dawasaz AA, Arem SA, Assiri KI. Artificial intelligence application in a case of mandibular third molar impaction: a systematic review of the literature. J Clin Med 2024; 13: 4431. DOI: 10.3390/jcm13154431.
20.
Issa J, Riad A, Olszewski R, Dyszkiewicz-Konwińska M. The influence of slice thickness, sharpness, and contrast adjustments on inferior alveolar canal segmentation on cone-beam computed tomography scans: a retrospective study. J Pers Med 2023; 13: 1518. DOI: 10.3390/jpm13101518.
21.
Issa J, Kulczyk T, Rychlik M, Czajka-Jakubowska A, Olszewski R, Dyszkiewicz-Konwińska M. Artificial intelligence versus semi-automatic segmentation of the inferior alveolar canal on cone-beam computed tomography scans: a pilot study. Dent Med Probl 2024; 61: 893-899. DOI: 10.17219/dmp/175968.
22.
Büttner M, Rokhshad R, Brinz J, et al. Core outcome measures in dental computer vision studies (DentalCOMS). J Dent 2024;150: 105318. DOI: 10.1016/j.jdent.2024.105318.
23.
Fenster A, Chiu B. Evaluation of segmentation algorithms for medical imaging. Conf Proc IEEE Eng Med Biol Soc 2005; 7186-7189. DOI: 10.1109/IEMBS.2005.1616166.
24.
Taha AA, Hanbury A. Metrics for evaluating 3D medical image segmentation: analysis, selection, and tool. BMC Med Imaging 2015; 15: 29. DOI: 10.1186/s12880-015-0068-x.
25.
Brock KK, Mutic S, McNutt TR, Li H, Kessler ML. Use of image registration and fusion algorithms and techniques in radiotherapy: report of the AAPM radiation therapy committee task group no. 132. Med Phys 2017; 44: e43-e76. DOI: 10.1002/mp.12256.
26.
Jaskari J, Sahlsten J, Järnstedt J, et al. Deep learning method for mandibular canal segmentation in dental cone beam computed tomography volumes. Sci Rep 2020; 10: 5842. DOI: 10.1038/s41598-020-62321-3.
27.
Järnstedt J, Sahlsten J, Jaskari J, et al. Comparison of deep learning segmentation and multigrader-annotated mandibular canals of multicenter CBCT scans. Sci Rep 2022; 12: 18598. DOI: 10.1038/s41598-022-20605-w.
28.
Lysenko AV, Yaremenko AI, Ivanov VM, et al. Comparison of dental implant placement accuracy using a static surgical guide, a virtual guide and a manual placement method – an in-vitro study. Ann Maxillofac Surg 2023; 13: 158-162. DOI: 10.4103/ams.ams_100_23.
29.
Tohka J. Partial volume effect modeling for segmentation and tissue classification of brain magnetic resonance images: a review. World J Radiol 2014; 6: 855-864. DOI: 10.4329/wjr.v6.i11.855.
30.
Juneja M, Aggarwal N, Saini S, et al. A comprehensive review on artificial intelligence-driven preprocessing, segmentation, and classification techniques for precision furcation analysis in radiographic images. Multimed Tools Appl 2024. DOI: 10.1007/s11042-024-19920-3.
31.
Orhan K, Bilgir E, Bayrakdar IS, Ezhov M, Gusarev M, Shumilov E. Evaluation of artificial intelligence for detecting impacted third molars on cone-beam computed tomography scans. J Stomatol Oral Maxillofac Surg 2021; 122: 333-337. DOI: 10.1016/j.jormas.2020. 12.006.
32.
Kempers S, van Lierop P, Hsu TH, Moin DA, Bergé S, Ghaeminia H, Xi T, Vinayahalingam S. Positional assessment of lower third molar and mandibular canal using explainable artificial intelligence. J Dent 2023; 133: 104519. DOI: 10.1016/j.jdent.2023.104519.
33.
Joo Y, Moon SY, Choi C. Classification of the relationship between mandibular third molar and inferior alveolar nerve based on generated mask images. IEEE Access 2023; 11: 81777-81786. DOI: 10.1109/ACCESS.2023.3302271.
34.
Fukuda M, Ariji Y, Kise Y, Nozawa M, Kuwada C, Funakoshi T, et al. Comparison of 3 deep learning neural networks for classifying the relationship between the mandibular third molar and the mandibular canal on panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol 2020; 130: 336-343. DOI: 10.1016/j.oooo.2020.04.005.
35.
Kazimierczak W, Kazimierczak N, Kędziora K, Szcześniak M, Serafin Z. Reliability of the AI-assisted assessment of the proximity of the root apices to mandibular canal. J Clin Med 2024; 13: 3605. DOI: 10.3390/jcm13123605.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.