Introduction
The main purpose of endodontic treatment (ET) is to prevent and treat acute and chronic apical periodontitis (AP). From a biomechanical point of view, this means cleaning, shaping, and disinfecting the root canal system to allow three-dimensional filling at a later stage. Achieving these goals is a prerequisite for therapeutic success [1-3].
ET is a multi-stage process in which a number of factors must be taken into account. One of the factors is radiological control after ET. Radiologic features of appropriate ET are as follows:
prepared root canal filled completely unless space is needed for a post;
the prepared and filled canal contain the original canal;
no space between canal filling and canal wall can be seen;
there should be no canal space visible beyond the end-point of the root canal filling;
the tooth should be adequately restored after root canal filling to prevent bacterial recontamination of the root canal system or fracture of the tooth [4].
During diagnosis and treatment planning, it is extremely important to know the morphology of the root canal system and its deviations from the norm, as well as the shape and size of the pulp chamber. This knowledge allows for thorough treatment planning and increases the likelihood of a positive treatment outcome [5]. A successful ET can be well defined by the absence of apical periodontitis and the absence of clinical symptoms after a period of observation.
Intraoral radiographs are an essential diagnostic tool used during the planning of ET. They provide information on tooth anatomy, the presence of periapical lesions, their progression, and treatment results. Periapical lesions are visible on radiographs if there has been a loss of bone mineralisation in the range of 30 to 50%. For this reason, periapical lesions are not always visible on X-rays [6-8]. X-rays are two-dimensional images of a three-dimensional structure, which means that some features of the examined area may not be sufficiently visible. In addition, differences in the density of the bone surrounding the examined tooth and the difficulty in obtaining reproducible images can affect the interpretation of this type of tissue imaging [6,9]. The introduction of cone-beam computed tomography (CBCT) into daily practice has enabled three-dimensional imaging of the dentition, the maxillofacial skeleton, and the interrelationships of anatomical structures. CBCT imaging, however, has some disadvantages. These include the increased radiation dose absorbed by the patient, the generation of artifacts, and the occurrence of scattered radiation that makes a substantial contribution to the image noise [10-12].
CBCT offers the possibility of using different sizes of the imaging area (FOV – field of view), which ranges from 3 to 20 cm. Using CBCT for endodontic diagnosis, it is important to follow the principle of using the smallest possible FOV, the smallest possible voxel size and the shortest possible patient exposure time when operating with pulsed emission mode [13,14].
The purpose of this study was a retrospective cross-sectional study of the Polish subpopulation performed to evaluate the quality of ET and the condition of periapical tissues of permanent teeth based on CBCT images and the influence of the quality of ET on the occurrence of periapical lesions.
Material and methods
A retrospective cross-sectional study included a group of patients who underwent a CBCT in the period from 01/01/2015 to 04/06/2021 at the University Dental Clinic of the Pomeranian Medical University in Szczecin, Poland. The entire material was collected retrospectively based on the available medical records. The CBCT images used in this study were acquired for a variety of indications, i.e. orthodontic, implant, orthognathic, surgical, and ET planning. The consent of the Bioethics Committee of the Pomeranian Medical University in Szczecin was obtained to conduct the study, with consent number KB-0012/191/04/18.
Inclusion criteria for the study group were as follows: patients over 18 years of age, permanent teeth, the teeth and their periapical region visible on all the multiplanar views (axial, coronal and sagittal), CBCT field of view 6 × 8, 8 × 8, 8 × 15, voxel size ≤ 200 μm (4-16 mA, 57-90 kV, 6.1-2.3 s). Cases not fulfilling these criteria were excluded from the study. Maxillary and mandibular third molars, impacted teeth, and records with poor quality were also excluded from the analysis.
The CBCT scans were recorded using the Cranex® 3Dx (Soredex Oy, Tuusula, Finland). The scans were evaluated using the OnDemand 3D program (Cybermed Co, Seoul, Korea) in a darkened room by one endodontist with 6 years of clinical experience (KLB), who was calibrated before the start of the study. Intra-observer reliability for PESS index was assessed by calculating Cohen’s k by a double scoring of 50 randomly selected CBCTs at one-month intervals. All kappa values exceeded 0.80. In cases of difficult assessment, the images were consulted by a senior endodontist (AN).
No CBCT study has been performed specifically for this study. The age, sex, total number of teeth, number of endodontically treated teeth, and number of teeth with AP of each patient included for the study were recorded.
The periapical and endodontic status scale (PESS) was used to assess the quality of ET and the extent of apical periodontitis on CBCT. The first part of the PESS is the Complex Periapical Index (COPI), which was designed for evaluation of periapical lesions. The second part of the PESS is the Endodontically Treated Tooth Index (ETTI), which was designed for ET quality evaluation [15]. The COPI was used to assess the AP in each tooth included in the analyses. The relationship between root and radiolucent lesion (R) was assessed only for multi-rooted teeth. The ETTI was used to make canal-by-canal assessments of each endodontically treated tooth (Figure 1). For the purposes of this study, the ETTI has been modified by adding the H3 score to assess the homogeneity of the root canal filling. The H3 score refers to the absence of a root canal filling in the case of previous pulp amputation or canals missed in previous ET (filling material visible only in the aspect of the pulp chamber). The periapical and endodontic status scale is presented in Table 1.
Table 1
The periapical and endodontic status scale (PESS)
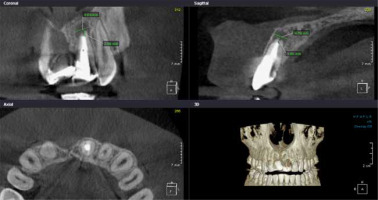
Figure 1
Assessment of endodontic treatment (L2H1CS1CF5) and apical periodontitis (S2RxD1) using the PESS index. L2 – root canal filling > 2 mm from radiographic apex, H1 – complete obturation (homogenous appearance of the root canal filling), CS1 – adequate coronal seal, CF5 – endodontically treated root with radiolucency, S2 – diameter of medium well-defined radiolucency 3-5 mm, Rx – no assessment, D1 – radiolucency around the root
Statistical analysis
The study group was evaluated using descriptive analysis. Pearson’s χ2 test was used to evaluate the differences in the quality of ET and AP in different age groups of patients and in different groups of teeth, as well as to evaluate the difference in size, root-to-AP ratio, and location of bone destruction according to the quality of ET. For all groups compared, a p-value < 0.05 was considered significant. The odds ratio (OR) was used to determine the characteristics of the quality of ET and AP.
All analyses were performed using Statistica 13.0 software (StatSoft Poland).
Results
Of the 1351 CBCT records, after applying the exclusion criteria, 180 scans were available for statistical analysis (85 male and 95 female, mean age 41.85 ± 15.51 years), containing 4158 permanent teeth. The distribution of patients by age and gender is shown in Table 2. Apical periodontitis was found in 248 teeth (6%), ET was found in 413 teeth (9.9%), and both ET and AP were observed in 159 teeth (3.8%).
Table 2
Distribution of the study population
Apical periodontitis, COPI
Apical periodontitis was present in 248 teeth evaluated and included ET teeth (159) and non-ET teeth (89). All age groups were dominated by small, well-defined lesions up to 3 mm in diameter (46.4%), except for the group of patients aged 18-29 years, in whom large lesions over 5 mm were predominant. Medium well-defined radiolucency 3-5 mm was diagnosed in 16.2% of teeth and large well-defined radiolucency > 5 mm in 37.5% of teeth. Apical periodontitis involved one or more than one root in 41.7% and 44.7% of teeth, respectively. 13.6% of teeth with a radiolucent lesion involved a furcation. The most common bone destruction (63.7%) was observed around the tooth root, while the least common bone destruction (12.9%) was in contact with important anatomical structures such as the maxillary sinus, inferior alveolar nerve canal or incisive canal. The destruction of cortical bone occurred in 23.4% of the teeth. Table 3 summarises the COPI index in the age and tooth groups.
Table 3
Complex periapical index according to age and tooth group (%)
| Age group | Teeth group | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ET | Non-ET | ET | Non-ET | |||||||||||||||||
| 18-29 | 30-39 | 40-49 | 50-59 | ≥ 60 | Total | 18-29 | 30-39 | 40-49 | 50-59 | ≥ 60 | Total | Anterior | Premolar | Molar | Total | Anterior | Premolar | Molar | Total | |
| S1 | 8 (3.2) | 27 (10.9) | 21 (8.5) | 17 (6.9) | 16 (6.5) | 89 (35.9) | 2 (0.8) | 4 (1.6) | 4 (1.6) | 8 (3.2) | 8 (3.2) | 26 (10.5) | 19 (7.7) | 20 (8.1) | 50 (20.2) | 89 (35.9) | 13 (5.2) | 8 (3.2) | 5 (2.0) | 26 (10.5) |
| S2 | 2 (0.8) | 8 (3.2) | 5 (2.0) | 4 (1.6) | 3 (1.2) | 22 (8.9) | 1 (0.4) | 5 (2.0) | 3 (1.2) | 7 (2.8) | 2 (0.8) | 18 (7.3) | 5 (2.0) | 6 (2.4) | 11 (4.4) | 22 (8.9) | 10 (4.0) | 7 (2.8) | 1 (0.4) | 18 (7.3) |
| S3 | 9 (3.6) | 10 (4.0) | 12 (4.8) | 7 (2.8) | 10 (4.0) | 48 (19.4) | 7 (2.8) | 6 (2.4) | 9 (3.6) | 9 (3.6) | 14 (5.6) | 45 (18.1) | 14 (5.6) | 13 (5.2) | 21 (8.5) | 48 (19.4) | 28 (11.3) | 11 (4.4) | 6 (2.4) | 45 (18.1) |
| Total | 19 (11.7) | 45 (18.1) | 38 (15.3) | 28 (11.3) | 29 (11.7) | 159 (64.1) | 10 (4.0) | 15 (6.0) | 16 (6.5) | 24 (9.7) | 24 (9.7) | 89 (35.9) | 38 (15.3) | 39 (15.7) | 82 (33.1) | 159 (64.1) | 51 (20.6) | 26 (10.5) | 12 (4.8) | 89 (35.9) |
| χ2 = 5.09, p = 0.75 | χ2 = 7.41, p = 0.49 | χ2 = 2.11, p = 0.72 | χ2 = 2.87, p = 0.58 | |||||||||||||||||
| R1 | 3 (2.9) | 11 (10.7) | 6 (5.8) | 6 (5.8) | 7 (6.8) | 33 (32.0) | 2 (1.9) | 1 (1.0) | 3 (2.9) | 1 (1.0) | 3 (2.9) | 10 (9.7) | – | 9 (8.7) | 24 (23.3) | 33 (32.0) | – | 6 (5.8) | 4 (3.9) | 10 (9.7) |
| R2 | 5 (4.9) | 11 (10.7) | 8 (7.8) | 12 (11.7) | 4 (3.9) | 40 (38.8) | 3 (2.9) | – | – | 2 (1.9) | 1 (1.0) | 6 (5.8) | – | 5 (4.9) | 35 (34.0) | 40 (38.8) | – | 1 (1.0) | 5 (4.9) | 6 (5.8) |
| R3 | – | 2 (1.9) | 3 (2.9) | 3 (2.9) | – | 8 (7.8) | – | 1 (1.0) | 2 (1.9) | – | 2 (1.9) | 6 (5.8) | – | 1 (1.0) | 7 (6.8) | 8 (7.8) | – | 3 (2.9) | 3 (2.9) | 6 (5.8) |
| Total | 8 (7.8) | 24 (23.3) | 17 (16.5) | 21 (20.4) | 11 (10.7) | 81 (78.6) | 5 (4.9) | 2 (1.9) | 5 (4.9) | 3 (2.9) | 6 (5.8) | 22 (21.4) | – | 15 (14.6) | 66 (64.1) | 81 (78.6) | – | 10 (9.7) | 12 (11.7) | 22 (21.4) |
| χ2 = –, p = –A | χ2 = –, p = –A | χ2 = 2.83, p = 0.24 | χ2 = 2.91, p = 0.23 | |||||||||||||||||
| D1 | 16 (6.5) | 32 (12.9) | 22 (8.9) | 23 (9.3) | 17 (6.9) | 110 (44.4) | 7 (2.8) | 5 (2.0) | 6 (2.4) | 16 (6.5) | 14 (5.6) | 48 (19.4) | 26 (10.5) | 23 (9.3) | 61 (24.6) | 110 (44.4) | 30 (12.1) | 14 (5.6) | 4 (1.6) | 48 (19.4) |
| D2 | 2 (0.8) | 7 (2.8) | 9 (3.6) | 1 (0.4) | 1 (0.4) | 20 (8.1) | 1 (0.4) | 4 (1.6) | 3 (1.2) | 2 (0.8) | 2 (0.8) | 12 (4.8) | 1 (0.4) | 7 (2.8) | 12 (4.8) | 20 (8.1) | 3 (1.2) | 5 (2.0) | 4 (1.6) | 12 (4.8) |
| D3 | 1 (0.4) | 6 (2.4) | 7 (2.8) | 4 (1.6) | 11 (4.4) | 29 (11.7) | 2 (0.8) | 6 (2.4) | 7 (2.8) | 6 (2.4) | 8 (3.2) | 29 (11.7) | 11 (4.4) | 9 (3.6) | 9 (3.6) | 29 (11.7) | 18 (7.3) | 7 (2.8) | 4 (1.6) | 29 (11.7) |
| Total | 19 (11.7) | 45 (18.1) | 38 (15.3) | 28 (11.3) | 29 (11.7) | 159 (64.1) | 10 (4.0) | 15 (6.0) | 16 (6.5) | 24 (9.7) | 24 (9.7) | 89 (35.9) | 38 (15.3) | 39 (15.7) | 82 (33.1) | 159 (64.1) | 51 (20.6) | 26 (10.5) | 12 (4.8) | 89 (35.9) |
| χ2 = 8.34, p = 0.40 | χ2 = 19.08, p = 0.01* | χ2 = 10.33, p = 0.04* | χ2 = 7.87, p = 0.96 | |||||||||||||||||
ET – endodontic treatment, S1 – diameter of small well-defined radiolucency up to 3 mm, S2 – diameter of medium well-defined radiolucency 3-5 mm, S3 – diameter of large well-defined radiolucency > 5 mm, R1 – radiolucent lesion appears on one root, R2 – radiolucent lesion appears on more than one root, R3 – radiolucent lesion with involvement of furcation, D1 – radiolucency around the root, D2 – radiolucency is in contact with important anatomical structures, D3 – destruction of cortical bone
Endodontic treatment, ETTI
Endodontically treated roots without AP (22.1%) and roots with AP (9.4%) were most common between the ages of 30 and 39 years. Based on the statistical analysis, significant correlations were found between the results presented in Table 4. The data obtained show that the highest number of endodontically treated teeth affected by AP was found in teeth with root canal filling 0-2 mm from the radiographic apex, incomplete canal obturation, and adequate coronal seal in the third decade of life. The lowest number of ET teeth affected by AP was observed in teeth with root canal overfilling and complete obturation between the ages of 18 and 29 and over 60 years, and in teeth with lack of the root canal filling between the ages of 18 and 29 years and the fifth decade of life. Among the ET teeth without AP, the most numerous group consisted of teeth with root canal filling 0-2 mm from the radiographic apex and complete obturation, as well as adequate coronal seal in the third decade of life. The most common condition following ET was AP and untreated or missed root canals.
Table 4
Endodontically treated teeth index according to the age and teeth group (%)
| Age group | Teeth group | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ET with AP | ET without AP | ET with AP | ET without AP | |||||||||||||||||
| 18-29 | 30-39 | 40-49 | 50-59 | ≥ 60 | Total | 18-29 | 30-39 | 40-49 | 50-59 | ≥ 60 | Total | Anterior | Premolar | Molar | Total | Anterior | Premolar | Molar | Total | |
| L1 | 16 (1.9) | 30 (3.6) | 24 (2.9) | 22 (2.6) | 7 (0.8) | 99 (11.8) | 41 (4.9) | 110 (13.1) | 78 (9.3) | 68 (8.1) | 44 (5.2) | 341 (40.6) | 21 (2.5) | 11 (1.3) | 67 (8.0) | 99 (11.8) | 55 (6.6) | 100 (11.9) | 186 (22.2) | 341 (406) |
| L2 | 5 (0.6) | 28 (3.3) | 25 (3.0) | 17 (2.0) | 20 (2.4) | 95 (11.3) | 12 (1.4) | 51 (6.1) | 26 (3.1) | 25 (3.0) | 27 (3.2) | 141 (16.8) | 11 (1.3) | 29 (3.5) | 55 (6.6) | 95 (11.3) | 21 (2.5) | 45 (5.4) | 75 (8.9) | 141 (16.8) |
| L3 | 1 (0.1) | 7 (0.8) | 4 (0.5) | 8 (1.0) | 1 (0.1) | 21 (2.5) | 2 (0.2) | 12 (1.4) | 11 (1.3) | 7 (0.8) | 4, (0.5) | 36 (4.3) | 3 (0.4) | 5 (0.6) | 13 (1.5) | 21 (2.5) | 9 (1.1) | 6 (0.7) | 21 (2.5) | 36 (4.3) |
| L4 | 8 (1.0) | 12 (1.4) | 14 (1.7) | 8 (1.0) | 15 (1.8) | 57 (6.8) | 5 (0.6) | 12 (1.4) | 12 (1.4) | 10, (1.2) | 8 (1.0) | 47 (5.6) | 1 (0.1) | 10 (1.2) | 46 (5.5) | 57 (6.8) | 2 (0.2) | 3 (0.4) | 42 (5.0) | 47 (5.6) |
| L5 | – | 2 (0.2) | – | – | – | 2 (0.2) | – | – | – | – | – | – | 2 (0.2) | – | – | 2 (0.2) | – | – | – | – |
| Total | 30 (3.6) | 79 (9.4) | 67 (8.0) | 55 (6.6) | 43 (5.1) | 274 (32.7) | 60 (7.2) | 185 (22.1) | 127 (15.1) | 110 (13.1) | 83 (9.9) | 565 (67.3) | 38 (4.5) | 55 (6.6) | 181(22.2) | 274 (32.7) | 87 (10.4) | 154 (18.4) | 324 (38.6) | 565 (67.3) |
| χ2 = 25.14, p = 0.01* | χ2 = 9.13, p = 0.69 | χ2 = 35.03, p = 0.00* | χ2 = 26.04, p = 0.00* | |||||||||||||||||
| H1 | 8 (1.0) | 33 (3.9) | 28 (3.3) | 27 (3.2) | 8 (1.0) | 104 (12.4) | 51 (6.1) | 146 (17.4) | 100 (11.9) | 82 (9.8) | 65 (7.7) | 444 (52.9) | 17 (2.0) | 16 (1.9) | 71 (8.5) | 104 (12.4) | 76 (9.1) | 130 (15.5) | 238 (28.4) | 444 (52.9) |
| H2 | 14 (1.7) | 34 (4.1) | 25 (3.0) | 20 (2.4) | 20 (2.4) | 113 (13.5) | 4 (0.5) | 27 (3.2) | 15(1.8) | 18 (2.1) | 10 (7.7) | 74 (8.8) | 20 (2.4) | 29 (3.5) | 64 (7.6) | 113 (13.5) | 9 (1.1) | 21 (2.5) | 44 (5.2) | 74 (8.8) |
| H3 | 8 (1.0) | 12 (1.4) | 14 (1.7) | 8 (1.0) | 15 (1.8) | 57 (6.8) | 5(0.2) | 12 (1.4) | 12 (1.4) | 10 (1.2) | 8 (1.0) | 47 (5.6) | 1 (0.1) | 10 (1.2) | 46 (5.5) | 57 (6.8) | 2 (0.2) | 3 (0.4) | 42 (5.0) | 47 (5.6) |
| Total | 30 (3.6) | 79 (9.4) | 67 (8.0) | 55 (6.6) | 43 (5.1) | 274 (32.7) | 60 (7.2) | 185 (22.1) | 127 (15.1) | 110 (13.1) | 83 (9.9) | 565 (67.3) | 38 (4.5) | 55 (6.6) | 181 (21.6) | 274 (32.7) | 87 (10.4) | 154 (18.4) | 324 (38.6) | 565 (67.3) |
| χ2 = 15.57, p = 0.05* | χ2 = 5.08, p = 0.75 | χ2 = 14.21, p = 0.01* | χ2 = 22.90, p = 0.00* | |||||||||||||||||
| CS1 | 28 (3.3) | 63 (7.5) | 48 (5.7) | 45 (5.4) | 35 (4.2) | 219 (26.1) | 53 (6.3) | 173 (20.6) | 113 (13.5) | 105 (12.5) | 68 (8.1) | 512 (61.0) | 36 (4.3) | 35 (4.2) | 148 (17.6) | 219 (26.1) | 83 (9.9) | 143 (17.0) | 286 (34.1) | 512 (61.0) |
| CS2 | 2 (0.2) | 16 (1.9) | 19 (2.3) | 10 (1.2) | 8 (1.0) | 55 (6.6) | 7 (0.8) | 12 (1.4) | 14 (1.7) | 5 (0.6) | 15 (1.8) | 53 (6.3) | 2 (0.2) | 20 (2.4) | 33 (3.9) | 55 (6.6) | 4 (0.5) | 11 (1.3) | 38 (4.5) | 53 (6.3) |
| Total | 30 (3.6) | 79 (9.4) | 67 (8.0) | 55 (6.6) | 43 (5.1) | 274 (32.7) | 60 (7.2) | 185 (22.1) | 127 (15.1) | 110 (13.1) | 83 (9.9) | 565 (67.3) | 38 (4.5) | 55 (6.6) | 181 (21.6) | 274 (32.7) | 87 (10.4) | 154 (18.4) | 324 (38.6) | 565 (67.3) |
| χ2 = 6.41, p = 0.17 | χ2 = 13.00, p = 0.01* | χ2 = 14.68, p = 0.00* | χ2 = 5.35, p = 0.07* | |||||||||||||||||
| CF1 | – | – | 1 (0.3) | – | 1 (0.3) | 2 (0.5) | – | – | – | – | – | – | – | – | 2 (0.5) | 2 (0.5) | – | – | – | – |
| CF2 | 8 (2.1) | 12 (3.1) | 14 (3.6) | 8 (2.1) | 15 (3.9) | 57 (14.8) | 5 (1.3) | 12 (3.1) | 12 (3.1) | 10 (2.6) | 8 (2.1) | 47 (12.2) | 1 (0.3) | 10 (2.6) | 46 (11.9) | 57 (14.8) | 2 (0.5) | 3 (0.8) | 42 (10.9) | 47 (12.2) |
| CF3 | – | 1 (0.3) | – | – | 1 (0.3) | 2 (0.5) | – | 2 (0.5) | – | – | – | 2 (0.5) | – | – | 2 (0.5) | 2 (0.5) | – | – | 2 (0.5) | 2 (0.5) |
| CF4 | – | – | 1 (0.3) | – | – | 1 (0.3) | 1 (0.3) | – | – | – | – | 1 (0.3) | – | – | 1 (0.3) | 1 (0.3) | 1 (0.3) | – | – | 1 (0.3) |
| CF5 | 30 (7.8) | 79 (20.5) | 67 (17.4) | 55 (14.2) | 43 (11.1) | 274 (71.0) | – | – | – | – | – | – | 38 (9.8) | 49 (12.7) | 187 (48.4) | 274 (71.0) | – | – | – | – |
| Total | 38 (9.8) | 92 (23.8) | 83 (21.5) | 63 (16.3) | 60 (15.5) | 336 (87.0) | 6 (1.6) | 14 (3.6) | 12 (3.1) | 10 (2.6) | 8 (2.1) | 50 (13.0) | 39 (10.1) | 59 (15.3) | 238 (61.6) | 336 (87.0) | 3 (0.8) | 3 (0.8) | 44 (11.4) | 50 (13.0) |
| χ2 = –, p = –A | χ2 = –, p = –A | χ2 = –, p = –A | χ2 = –, p = –A | |||||||||||||||||
ET – endodontically treated root, AP – apical periodontitis, L1 – 0-2 mm from radiographic apex, L2 – > 2 mm from radiographic apex, L3 – overfilling (extrusion of material through the apex), L4 – filling material visible only in pulp chamber, L5 – filled canal of a surgically treated root, H1 – complete obturation (homogenous appearance of the root canal filling), H2 – incomplete obturation (voids and porous appearance of the root canal filling), H3 – lack of the root canal filling, CS1 – adequate (coronal restoration appears intact radiographically), CS2 – inadequate (detectable radiographic signs of overhangs, open margins, recurrent caries, or lost coronal restoration), CF1 – root perforation, CF2 – root canal not treated/missed, CF3 – root resorption, CF4 – root/tooth fracture, CF5 – endodontically treated root with radiolucency
Molars with root canal filling 0-2 mm from the radiographic apex and complete obturation, as well as adequate coronal seal constituted the most numerous group of ET teeth without AP and those with AP. Complications after ET, i.e. AP and untreated or missed root canals, were also most common in molars.
Relationship between ETTI and COPI
Statistical analysis showed that significant factors for the occurrence of small periapical lesions were underfilled root canals (p = 0.00), teeth treated with the amputation method (p = 0.00), and inhomogeneous filling in root canal (p = 0.00). The appearance of a medium-sized periapical lesion was influenced by filling material visible only in the pulp chamber (p = 0.00) and incomplete obturation of the root canal (p = 0.00). The risk of a large periapical lesion greater than 5 mm in diameter was statistically significantly increased in underfilled root canals (p = 0.00), material pushed beyond the radiographic apex (p = 0.01), root canals treated with the amputation method (p = 0.03), filled root canals of teeth that underwent microsurgical treatment (p = 0.01), and voids and porous filling in the root canal lumen (p = 0.03).
Statistical analysis showed that inadequate coronal sealing in the final restoration (visible filling overhang, marginal gap, secondary caries or lost filling) had a statistically significant effect on the occurrence of small, medium, and large periapical lesions.
A periapical lesion affecting only one root of a multi-rooted tooth was influenced by an inhomogeneous filling in the root canal (p = 0.00) and treatment by amputation method (p = 0.01). Periapical lesions affecting more than one root (R2) were more frequent in the absence of root canal filling (p = 0.00), voids and porous filling in the root canal lumen (p = 0. 03), whereas the root furcation of teeth was more frequently affected by inflammatory lesions in teeth treated by amputation method (p = 0.00), in the case of inhomogeneous root canal filling (p = 0.02), and when the root canal filling material was pushed beyond the radiographic apex (p = 0.03).
Inadequate coronal sealing in the final restoration (visible filling overhang, marginal gap, secondary caries, or lost filling) had a significant influence on the occurrence of a periapical lesion affecting only one root of a multi-rooted tooth (p = 0.01) and the involvement of the root furcation by a periapical lesion (p = 0.00).
The location of bone destruction only around the roots and bone destruction in contact with important anatomical structures were statistically significantly influenced by all deficiencies in ET assessed by the ETTI index. The occurrence of cortical bone destruction was significantly affected by underfilled root canals (p = 0.00), canals with material pushed beyond the radiographic apex (p = 0.00), and filling material visible only in the pulp chamber (p = 0.00).
Statistical analysis showed that inadequate coronal sealing in the final restoration (visible filling overhang, marginal gap, secondary caries, or lost filling) had a significant influence on the location of bone destruction only around the roots, bone destruction in contact with important anatomical structures, and cortical bone destruction (for D1, D2, and D3; p = 0.00). Detailed results are presented in Table 5.
Table 5
The risk of apical periodontitis depending on the quality of endodontic treatment
| Indicators | Size of radiolucent lesion | OR | Cl | p | Relationship between root and radiolucent lesion | OR | Cl | p | Location of bone destruction | OR | Cl | p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Length of root filling | ||||||||||||
| L1 | S1 | 1.00 | R1 | 1.00 | D1 | 1.00 | ||||||
| L2 | 2.38 | 1.57-3.63 | 0.00* | 1.18 | 0.67-2.06 | 0.57 | 1.92 | 1.30-2.84 | 0.00* | |||
| L3 | 1.49 | 0.68-3.25 | 0.32 | 0.38 | 0.09-1.70 | 0.20 | 8.67 | 3.14-3.87 | 0.00* | |||
| L4 | 3.44 | 2.00-5.93 | 0.00* | 2.50 | 1.32-4.74 | 0.01* | 2.99 | 1.80-4.97 | 0.00* | |||
| L1 | S2 | 1.00 | R2 | 1.00 | D2 | 1.00 | ||||||
| L2 | 1.36 | 0.66-2.81 | 0.41 | 1.25 | 0.74-2.13 | 0.41 | 2.08 | 1.05-4.14 | 0.04* | |||
| L3 | 0.42 | 0.06-3.23 | 0.41 | 1.56 | 0.68-3.57 | 0.29 | – | – | – | |||
| L4 | 4.73 | 2.31-9.71 | 0.00* | 2.96 | 1.64-5.38 | 0.00* | 4.35 | 2.00-9.48 | 0.00* | |||
| L1 | S3 | 1.00 | R3 | 1.00 | D3 | 1.00 | ||||||
| L2 | 2.51 | 1.41-4.45 | 0.00* | 1.72 | 0.56-5.27 | 0.34 | 4.92 | 2.14-11.31 | 0.00* | |||
| L3 | 3.25 | 1.42-7.45 | 0.01* | 4.46 | 1.22-16.31 | 0.03* | 2.31 | 0.87-6.12 | 0.09 | |||
| L4 | 2.42 | 1.07-5.47 | 0.03* | 7.18 | 2.17-23.83 | 0.00* | 5.64 | 2.01-15.87 | 0.00* | |||
| L5 | 62.09 | 2.91-1325.80 | 0.01* | - | - | - | 179.74 | 8.06-4006.20 | 0.00* | |||
| Homogeneity of the root canal fillings | ||||||||||||
| H1 | S1 | 1.00 | R1 | 1.00 | D1 | 1.00 | ||||||
| H2 | 7.01 | 4.51-10.89 | 0.00* | 2.67 | 1.46-4.89 | 0.00* | 20.27 | 12.70-32.34 | 0.00* | |||
| H3 | 4.96 | 2.92-8.43 | 0.00* | 3.54 | 1.92-6.54 | 0.00* | 18.98 | 10.95-32.93 | 0.00* | |||
| H1 | S2 | 1.00 | R2 | 1.00 | D2 | 1.00 | ||||||
| H2 | 12.88 | 6.16-26.96 | 0.00* | 1.90 | 1.06-3.40 | 0.03* | 5.79 | 2.85-11.76 | 0.00* | |||
| H3 | 11.41 | 5.05-25.78 | 0.00* | 2.85 | 1.61-5.07 | 0.00* | 7.82 | 3.53-17.29 | 0.00* | |||
| H1 | S3 | 1.00 | R3 | 1.00 | D3 | 1.00 | ||||||
| H2 | 5.34 | 3.07-9.29 | 0.00* | 3.36 | 1.17-9.68 | 0.02* | 1.36 | 0.55-3.37 | 0.51 | |||
| H3 | 2.35 | 1.06-5.17 | 0.03* | 4.25 | 1.46-12.35 | 0.01* | 2.04 | 0.75-5.55 | 0.16 | |||
| Coronal seal | ||||||||||||
| CS1 | S1 | 1.00 | R1 | 1.00 | D1 | 1.00 | ||||||
| CS2 | 2.11 | 1.25-3.55 | 0.01* | 2.40 | 1.30-4.43 | 0.01* | 2.65 | 1.61-4.36 | 0.00* | |||
| CS1 | S2 | 1.00 | R2 | 1.00 | D2 | 1.00 | ||||||
| CS2 | 5.27 | 2.74-10.13 | 0.00* | 1.72 | 0.93-3.16 | 0.08 | 4.65 | 2.28-9.47 | 0.00* | |||
| CS1 | S3 | 1.00 | R3 | 1.00 | D3 | 1.00 | ||||||
| CS2 | 2.28 | 1.17-4.46 | 0.02* | 4.91 | 1.93-12.49 | 0.00* | 8.18 | 4.11-16.30 | 0.00* | |||
S1 – diameter of small well-defined radiolucency up to 3 mm, S2 – diameter of medium well-defined radiolucency 3-5 mm, S3 – diameter of large well-defined radiolucency > 5 mm, R1 – radiolucent lesion appears on one root, R2 – radiolucent lesion appears on more than one root, R3 – radiolucent lesion with involvement of furcation, D1 – radiolucency around the root, D2 – radiolucency is in contact with important anatomical structures, D3 – destruction of cortical bone, L1 – 0-2 mm from radiographic apex, L2 – > 2 mm from radiographic apex, L3 – overfilling (extrusion of material through the apex), L4 – filling material visible only in pulp chamber, L5 – filled canal of a surgically treated root, H1 – complete obturation (homogenous appearance of the root canal filling), H2 – incomplete obturation (voids and porous appearance of the root canal filling), H3 – lack of the root canal filling, CS1 – adequate (coronal restoration appears intact radiographically), CS2 – inadequate (detectable radiographic signs of overhangs, open margins, recurrent caries, or lost coronal restoration), OR – odds ratio, Cl - confidence interval
Discussion
Knowing the condition of endodontically treated teeth and the status of periapical tissues can help predict future oral health needs in patients of the examined population. In addition, the assessment of the quality of dental treatment in a given population can influence the educational program of future dentists and the direction of their professional development [7,16]. The present cross-sectional study was conducted on the basis of available CBCT examinations, so it does not represent a random sample of the Polish subpopulation. Therefore, extrapolation of results to the general population should be done with caution. According to Pak et al. [17] a cross-sectional survey is the best way to study health status, disease. and treatment provided in a population. Ideally, the study would have been conducted in a randomised setting, but performing CBCT in healthy patients does not follow American Association of Endodontists (ASE) and European Society of Endodontology (ETE) guidelines [13,14]. In CBCT imaging, the level of risk associated with increased radiation exposure compared to conventional imaging should be outweighed by the potential benefits.
In this study, 4158 teeth in 180 patients were evaluated. To date, the largest group of patients was evaluated by Meirinhos et al. [18], who examined 20,836 teeth in 1160 patients, and Aysal et al. [19], who examined 20,606 teeth. In these studies, a full-arch scan with voxel size of 200 μm or less was used. Van der Veken et al. [20] studied 11,117 teeth in 631 patients. Unfortunately, the authors did not provide CBCT imaging parameters (FOV and voxel size). Due to the aforementioned need for radiation protection of patients, CBCT examinations were also conducted on groups of smaller size. Paes da Silva et al. [21], Mashyakhy et al. [22], and Dutta et al. [23] in their CBCT-based cross-sectional studies evaluated, respectively, 3595 teeth in 245 patients with a voxel size of up to 0.3 mm, 5504 teeth in 208 patients with a voxel size of 0.25 mm (unfortunately, the authors did not provide information about the FOV), and 5585 teeth in 214 patients using voxel sizes of 0.25 mm and 0.3 mm and FOVs of 6, 8, and 13 cm. Cross-sectional studies based on orthopantomogram images in relation to CBCT were characterised by study groups with larger populations. In a study conducted by Huumonen et al. [24] on 6101 patients, the authors managed to evaluate as many as 120,635 teeth. Archana et al. [25] conducted their observations on a smaller group of 1340 patients (30,098 teeth evaluated). Kielbassa et al. [26] managed to include 1000 patients (22,584 evaluated teeth) in their study group.
In the present study, of all assessed teeth, AP was found in 6%, while AP co-occurred with ET in 3.8%. The findings of studies evaluating the prevalence of periapical lesions in other populations using CBCT imaging were as follows: Paes da Silva et al. [21] observed 3.4% of teeth affected by periapical lesions, and Dutta et al. [22], Van der Veken et al. [20], and Meirinhos et al. [18] found 5.8%, 5.9%, and 10.4% of such teeth, respectively. Endodontically treated teeth with co-existing AP accounted for 2.3%, 2.6%, 4.0%, and 6.1% in the studies by Dutta et al. [22], Paes da Silva et al. [21], Van der Veken et al. [20], and Meirinhos et al. [18], respectively. The presence of AP in teeth with correct ET may suggest the presence of a true periapical cyst, which have a completely enclosed lumina, unlike a pocket cyst which is open to the root canal. Pocket cysts heal after proper ET [27].
Our study showed that periapical lesions were most commonly observed in patients in the third decade of life, with an incidence rate of 1.4%. Similar observations were made by Van der Veken et al. [20] in a study of the Belgian population. Among subjects in the fourth decade of life, the percentage of teeth with a periapical lesion was 1.3%. Studies based on panoramic images and dental status yielded more varied results, as shown in Table 6. These differences may be due to several factors, such as the quality of imaging, the social status of the study population, the background of the study population, the level of education of the dentists in the study area, or the time at which the study was performed.
Table 6
Apical periodontitis in selected populations according to age group
| Year | Author | Country | AP in age groups (%)† | |||||
|---|---|---|---|---|---|---|---|---|
| 18-29 | 30-39 | 40-49 | 50-59 | ≥ 60 | Total | |||
| CBCT | ||||||||
| 2021 | The present study | Poland | 0.7 | 1.4 | 1.3 | 1.3 | 1.3 | 6.0 |
| 2017 | Van der Veken [20] | Belgium | 0.9 | 0.8 | 1.3 | 1.5 | 1.4 | 5.9 |
| Orthopantomogram | ||||||||
| 2017 | Kielbassa et al. [26] | Austria | 0.4 | 0.5 | 1.2 | 1.8 | 2.5 | 6.4 |
| 2016 | Miri et al. [39] | Iran | 0.8 | 0.9 | 1.0 | 0.8 | 0.9 | 4.4 |
| 2011 | Kamberi et al. [28] | Kosovo | 3.1 | 4.4 | 2.3 | 1.6 | 0.9 | 12.3 |
| A full-mouth radiographic survey (14 periapical radiographs) | ||||||||
| 2004 | Jiménez-Pinzón et al. [40] | Spain | 1.8 | 1.0 | 0.5 | 0.2 | 0.7 | 4.2 |
Periapical lesions in roots with inadequate root canal filling were frequently detected on radiographs in the epidemiological studies mentioned above [9,18,19,25,26]. The results of the present study show that after ET, 38.5% of teeth were affected by AP. This is similar to the results of the Belgian study based on CBCT by Van der Veken’s team [20] and the Japanese study based on orthopantomogram images developed by Tsuneishi’s team [30]. The findings of this study showed that teeth with underfilled root canals were almost 2.5 times more likely to develop small periapical lesions, and teeth where the filling material was only visible in the pulp chamber were almost 3.5 times more likely to develop these lesions, compared with teeth where the ET had been carried out correctly. Aysal et al. [19] showed in their CBCT study that the risk of periapical lesions was just over 3 times higher in roots with underfilled canals, 5.5 times higher in roots with overfilled canals, and almost 3 times higher in teeth with inhomogeneously filled canals, compared to correctly treated teeth. A meta-analysis by Alves Dos Santos et al. [31] in 2022, based on CBCT studies, showed that homogeneous root canal filling and correct filling length (0-2 mm from the apex opening) have an impact on the success of ET. It should be mentioned that various filling materials (gutta-percha, glass fibre, metal posts) produce artifacts in the CBCT image that affect the assessment of canal filling (false positive cases of homogeneous filling) and complications such as vertical root fracture [32,33].
Similar correlations have been observed in studies based on orthopantomograms. Jersa et al. [29] showed a 3-fold increased risk of periapical lesions in teeth with poor quality ET compared to teeth with correctly performed ET. Similarly, Kamberi et al. [28] found a 5-fold increase in the risk of periapical lesions, while Huumonen et al. [24] found a 2-fold and 2.5-fold increase in the risk of these lesions for incorrect root canal filling in men and women, respectively, compared to correct root canal filling. Unfortunately, the aforementioned authors used a simplistic analysis to evaluate ET. They only considered correctly or incorrectly performed ET. Dugas et al. [34] and Kielbassa et al. [26] addressed this issue in more detail by including the homogeneity of the root canal filling material and the quality of the crown restoration after ET in their analyses. The former team found an almost 3-fold increase in the risk of periapical lesions for teeth with inhomogeneous root canal fillings compared with teeth with a homogeneous filling, and a 2.5-fold and almost 3-fold increase in the risk of periapical lesions for teeth with underfilled and overfilled root canals, respectively, compared with teeth with a proper root canal filling. Dugas et al. [34] also considered the quality of the crown restoration and found an almost 2-fold increased risk of periapical lesions in teeth with abnormal crown fillings compared to teeth with normal restorations. The second team’s findings showed an almost 2-fold increased risk of periapical lesions in teeth with incorrect root canal fillings and lack of root canal filling homogeneity compared to teeth with correct root canal fillings, and an almost 2-fold increased risk of periapical lesions in teeth with incorrect crown fillings compared to teeth with correct restorations [26].
The presented study is cross-sectional based on available CBCT studies; therefore, it does not represent a random sample of the population. Hence, extrapolation of results to the general population should be done with caution. According to Pak et al. [17], a cross-sectional study is the best way to examine health status, disease, and treatment in a given population. Ideally, the project would include a randomised study, but performing CBCT in healthy patients is not consistent with ASE and ETE guidelines [13,14]. The potential benefits of CBCT imaging must be balanced by the relatively higher level of risk associated with radiation exposure compared to conventional imaging. In a 2015 meta-analysis by Ludlow et al. [35], the mean effective doses for large, medium, and small FOV CBCT are 212 μSv, 177 μSv, and 84 μSv, respectively, while for small FOV, many devices achieve reasonable exposures of around 30 μS.
The development of artificial intelligence is very promising and interesting. Attempts have been made to use it to diagnose caries and AP based on 2D and 3D images [36,37]. The results show that it is more useful in assessing AP on CBCT than orthopantomogram [37]. It seems that future research should focus on the development of artificial intelligence in the diagnosis of dental pathology.
Based on the cited findings, our own results, and the new concept of ALADA – “as low as diagnostically acceptable”, which is a modification of ALARA – “as low as reasonably achievable”, routine use of CBCT with small FOV for ET of molars can be considered [35,38].
Conclusions
The quality of the ET provided to the Polish subpopulation is not satisfactory. The lack of homogeneity of the root canal filling is a significant risk factor for ET failure, most commonly affecting molars. Improper ET and poor quality of crown restoration after ET have an impact on the increased risk of occurrence, size, degree of root coverage, and extent of inflammatory periapical lesions in relation to adjacent anatomical structures.
Disclosures
1. Institutional review board statement: The study was approved by the Bioethics Committee of the Pomeranian Medical University in Szczecin, with approval number KB-0012/191/04/18.
2. Assistance with the article: None.
3. Financial support and sponsorship: None.
4. Conflicts of interest: None.



