Introduction
In December 2019, a series of unclear pneumonia cases arose in Wuhan/Hubei, China, which attracted worldwide attention [1]. On 31 January 2020, the World Health Organization declared the Coronavirus outbreak as a public health danger of international concern [2]. The clinical manifestation of patients who have been infected with SARS-CoV-2 includes both being asymptomatic or having mild signs and symptoms as well as patients with severe hypo-xaemia and characteristic pulmonary infiltrates that can develop into acute respiratory distress syndrome (ARDS). The disease that is caused by the SARS-CoV-2 virus is called COVID-19, based on the WHO recommendation. Patients with COVID-19 who suffer from severe diseases require hospitalization with supportive treatment of the most serious complications such as hypo-xia, respiratory failure, acute kidney damage, gastrointestinal bleeding, secondary infections, or thromboembolism [3].
About 90% of body fat in most people is found subcutaneously. The remaining fatty tissue is called visceral fat. The accumulation of visceral fat has been associated with a variety of diseases. Visceral fat produces a higher concentration of pro-inflammatory cytokines, which are released into the bloodstream and can lead to a cytokine storm. General obesity has recently been recognized as an independent risk factor for critical illness in patients with COVID-19. The role of fat distribution, especially visceral fat, which is often associated with metabolic syndrome, remains unclear.
Apart from general obesity, the distribution of adipose tissue is an important risk factor for metabolic syndrome [4]. Visceral adipose tissue is often associated with the metabolic syndrome, which results in an increased risk of cardiovascular disease and type II diabetes along with subsequent increased morbidity.
CT (computed tomography) of the chest plays a key role not only in the early detection and diagnosis of COVID-19 pneumonia, but also in monitoring its clinical course and assessing the severity of the disease. The characteristic features of a CT scan for COVID-19 disease are ground-glass opacities, vascular enlargement, bilateral abnormalities, lower lobe involvement, and a posterior predilection [4,5].
The aim of the study was to assess the relationship between the epigastric visceral fat area and the severity of pneumonia in the course of COVID-19 using chest CT examinations according to the ages of the included patients.
Material and methods
The study included 177 unvaccinated patients (54 women and 123 men, with an average age of 65 years) who were hospitalized in the Emergency Ward and in the departments of the Upper Silesian Medical Centre between 01.10.2020 and 30.11.2020. COVID-19 infection was confirmed using the RT-PCR test based on a nasopharyngeal swab specimen for all of the patients. A chest CT scan is part of the assessment of pulmonary inflammatory lesions. The patients were divided into 2 groups relative to the age of 65 years: 1) ≥ 65 years – 102 patients (75.63%), 2) < 65 years – 75 patients (42.37%).
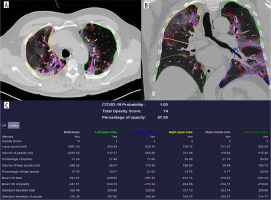
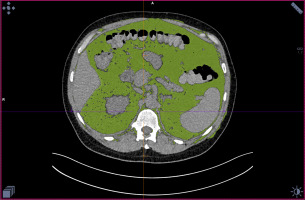
The cut-off point was adopted as a widely used cut-off in international references. The demographic data, information about the result of the COVID-19 test, and data about clinical outcomes in hospitalized patients were obtained from the hospital’s dedicated electronic system. The examinations were performed using a third-generation, dual-source CT system (Somatom Force; Siemens Healthineers, Forchheim, Germany) with the following scan and recon parameters: 120 kV, tube current automatically optimized to the patient’s size and shape using the CARE Dose system. Ref. mAs = 100 mAs, pitch = 1.2, rotation time = 0.5 s resulting in a scan time of 2.2 s. The lung series were reconstructed with a 0.75 mm slice thickness and an increment of 0.5 mm (overlapping) with an additional soft series reconstructed with a 1 mm slice thickness. The percentage changes in the amount of the affected lung tissue with a division into the individual lobes of both lungs were calculated using automatic postprocessing with the artificial intelligence powered software SyngoVia VB30A CT Pneumonia Analysis [6]. Based on the obtained results, the values of the Chest CT Score [7] and Total Opacity Score, which was created by Siemens Healthcare, were calculated. The opacity score was calculated for each lobe by estimating the given region percentage opacity using an artificial intelligence algorithm. An example of the Total Opacity Score is presented in Figure 1. Due to routine Chest CT imaging in patients with COVID-19, the area of epigastric visceral fat tissue was determined at the level of the upper endplate of the L1 vertebral body using SyngoVia VB30A Anatomy Visualizer software [8,9]. An example of the visceral fat visualisation is presented in Figure 2. This study was approved by our Bioethical Committee, Medical University of Silesia, and the requirement for informed consent was waived (IRB no. PCN/CBN/0022/KB1/113/21).
All the data were entered into a dedicated database. The Shapiro-Wilk test was used to check the normality of the data distribution. The 2 groups were compared using Student’s t-test for the normal distribution of a variable, while the groups without a normal distribution were analysed using the Mann-Whitney test. A correlation coefficient was used to measure the statistical relationship between 2 variables using Pearson’s r method. The results were considered to be significant at p-values < 0.05. All the presented analyses were performed using the advanced analytics software package Statistica 13 (TIBCO Software, Palo Alto, CA, USA).
Results
In a follow-up period of 2 months since hospital admission, 34 of the 177 (19.2%) included patients required hospitalization in the intensive therapy unit, 35 (19.8%) required mechanical ventilation, and 38 of the patients (21.5%) died.
The mean value of the visceral adipose tissue area was 196.23 ± 101.36 cm2. The area of adipose tissue significantly correlated with the percentage of affected lung tissue (r = 0.1476; p = 0.050), the Chest CT Score (r = 0.2086; p = 0.005), and the Total Opacity Score (r = 0.1744; p = 0.200).
The next part was an age-related analysis. The mean area of adipose tissue in the age group ≥ 65 years was 216.13 ± 105.19 cm2, while in the group < 65 years it was smaller, 169.18 ± 89.69 cm2. This difference was statistically significant (p = 0.002). The correlations of visceral tissue with the analysed parameters were also made according to age. In most cases, statistical correlations were only observed in the younger patients – the relationships between the area of visceral adipose tissue and affected lung volume percentage or semi-quantitative Chest-CT Score are presented graphically in Figures 3 and 4, respectively. There were no significant correlations found in the elderly patients. These data are presented in detail in Table 1.
Figure 3
The relationships between the area of visceral adipose tissue and affected lung volume percentage in younger patients aged < 65 years
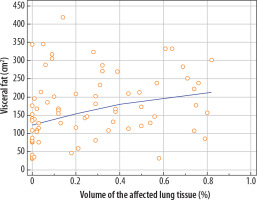
Figure 4
The relationships between the area of visceral adipose tissue and semi-quantitative Chest-CT Score younger patients aged < 65 years
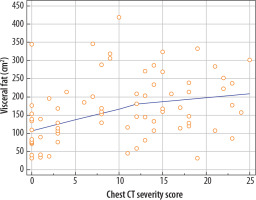
Table 1
Age-dependent correlations of epigastric region area of visceral fat with analysed parameters
Discussion
Obesity, especially abdominal obesity, is associated with metabolic syndrome and cardiovascular diseases, and it is also an independent risk factor for death [10]. Existing studies have shown that visceral adipose tissue is associated with higher production of inflammatory cytokines; however, the aging process changes the function, possibilities of proliferation, and size and number of adipocytes, which leads to changes in the secretion and synthesis of adipocytokines [11,12]. The development of imaging techniques such as computed tomography and magnetic resonance imaging has enabled remarkable progress to be made in the assessment of adipose tissue distribution [13].
The obtained results showed a correlation between the area of visceral adipose tissue and the extent of COVID-19 pneumonia in non-vaccinated patients, which is significant in patients under 65 years of age. Some additional semi-quantitative scales such as the Total Opacity Score and Chest CT Score were also used to assess the extent and distribution of the inflammatory changes in the lungs, which showed even stronger correlation between pneumonia severity and visceral adipose tissue area. In the group of patients above 65 years of age, however, no statistically significant correlation was found between the assessed parameters.
Our study proves a direct relationship between the volume of pulmonary parenchyma affected by inflammatory changes and the amount of visceral fat tissue. Visceral adipose tissue was previously associated with worse clinical outcomes in patients with COVID-19, especially in patients over 65 years of age [14]. This is contradictory to our results, which were statistically significant for patients under 65 year of age. This may suggest that factors other than the pure extent of lung inflammation can contribute to the clinical course of the disease.
Other research (Kuk et. al) have already shown that aging is associated with progressive changes in total and regional adipose tissue redistribution, which was also demonstrated as statistically significant in our study group [15]. This may lead to variable alterations in its secretory function, including pro- and anti-inflammatory cytokines produced by adipose tissue and therefore result in different inflammatory response in elderly individuals [16]. Further, more specific research is needed on the topic.
Our results confirm the relationship of visceral adipose tissue area with the severity of COVID-19 pneumonia in unvaccinated patients under 65 years of age. In clinical practice the relationship might be useful for predicting patients’ COVID-19 pneumonia course, utilizing routinely obtained or previous radiological imaging records. We must remember that other factors can also affected visceral fat. According to Liu J et al., body mass index (BMI) can correlate with visceral fat as well as others cardio metabolic risk factors including systolic blood pressure, triglyceride, and fasting plasma glucose, and inversely with HDL-C and physical activity score. Those factors may affect the results and we must remember about them reading the paper [17].