Introduction
Pancreaticoduodenectomy, also known as the Whipple procedure, is the preferred surgical method for the pancreatic head, uncinate process, and pancreatic neck masses. It is also predominantly preferred for the surgical treatment of the ampulla of Vater involving the periampullary region, extrahepatic biliary tracts, and duodenal masses. This technique had very high mortality and morbidity rates when first applied [1]. In the early series 60% morbidity and 25% mortality rates were reported [2]. However, with advances in the surgical techniques and postoperative intensive care facilities, mortality rates have been reported to have decreased to 2-10% and complications to 36-41% [2]. Today, mortality can even be lower than 5% in specialised centres [3]. Despite not always being life-threatening, complications related to the Whipple procedure increase hospital stay and costs and lead to delays in the adjuvant therapy of cancer patients. Major postoperative complications include postoperative abdominal abscesses, pelvic abscesses, hepatic infarction, biliary tract injuries or stricture, pancreatic fistulae, pancreatic anastomosis leakage, delayed gastric emptying, postoperative bleeding, and biliary leakage [2,4].
The majority of complications that develop after the Whipple procedure are diagnosed by cross-sectional imaging. Computed tomography (CT) is the most common imaging modality for a rapid and adequate diagnostic examination in patients with suspected postoperative complications. Shorter examination time and wider availability are among the advantages of CT over magnetic resonance imaging [1,5]. This study aimed to evaluate early CT findings in patients suspected of complications following the Whipple procedure.
MATERIAL AND METHODS
The local institutional review board approved this retrospective study and waived informed consent. Patients who underwent the Whipple procedure between January 2015 and January 2019 were retrospectively screened. Of the 65 patients who underwent this procedure, 48 also had a CT examination due to the suspicion of early postoperative complications. A CT scan had been performed using intravenous contrast material in 45 of these patients. Oral contrast agent was used in patients other than suspected vascular complications. The remaining patients without contrast-enhanced images were excluded from the study. As a result, the CT images of a total of 45 patients were evaluated.
All the CT scans were performed using a multi-slice CT device (Toshiba, Aquillon 64, Japan; GE, Revolution EVO, USA) in the routine portal phase (60 s) after intravenous contrast agent injection. The following CT parameters were used: 200-250 mAs, 120 kVp, and 0.5-0.625 isotropic spatial resolution. The intravenous contrast agent (1.5 ml/kg; iopromide 370, Bayer Schering Pharma AG, Germany or iohexol 350, GE Healthcare, USA) was administered through the antecubital veins with an automatic syringe at a rate of 3 ml/s. Dilute contrast agent was used in patients using oral contrast agent (1/30 ratio). The images were consecutively evaluated by two radiologists based on consensus using a dedicated workstation (GE, Advantage Workstation 4.3, USA).
In the early postoperative period, thin-walled, homogeneous with pure fluid attenuation and without air in the surgical bed and near the anastomoses collection were evaluated as fluid collection. The presence of air within a fluid collection with a thickened and enhancing wall was diagnosed as abscesses formation. A collection showing abscess CT findings in the liver parenchyma after the operation was evaluated as hepatic abscess. Fluid collections in the pancreatic bed or around the pancreaticojejunostomy site, air bubbles in a peripancreatic collection, disruption of the pancreatic anastomosis, or showing extravasation oral contrast materials was evaluated as the presence of pancreatic fistula. Similarly, gastrojejunostomy leakage was diagnosed by demonstrating the defect or contrast agent passage in the anastomosis site and the presence of fluid collection around the anastomosis. Superior mesenteric vein (SMV) and portal vein thromboses were evaluated with a full or partial filling defect in the lumen, especially in the portal phase. In patients with clinical suspicion of delayed gastric emptying, severely distended stomach filled with oral contrast material on CT suggested delayed gastric emptying. Active extravasation of arterial contrast agent was evaluated as active bleeding and intraluminal haemorrhage [6,7].
RESULTS
The Whipple operation was performed to 65 patients. Forty-five of these patients had early CT scans after the Whipple procedure; 30 were men and 15 were women. The mean age of the patients was 61.1 years (range: 20-81 years), being calculated as 62.1 years (range: 20-81 years) for women and 62.6 years (range: 40-77 years) for men. The mean time between the procedure and the CT scan was 14 days (5-45 days).
Complications were found in 24 patients (53.33%), while 21 cases (47.67%) developed no complications. In clinical follow-up, 10 of 21 patients underwent control CT examination, and there was no complication in follow-up CT examinations. The symptoms of all 21 patients regressed, and they were discharged without complications. Of the 24 patients with complications, 13 had multiple complications. Eight of these patients had fluid collection in the operation site, 10 had an abscess, five had a pancreatic fistula, and two had haematoma. In addition, delayed gastric emptying was detected in six patients, anastomotic leakage in the gastrojejunostomy line in two patients, SMV thrombosis that was not observed in the preoperative CT scan in two patients (one complete and one partial), a hepatic abscess in one patient, and intraluminal haemorrhage and active extravasation in one patient. In two patients, the haematoma was located intraabdominally, extraluminally in the peritoneal cavity between the small bowel loops. In the patient with intraluminal haemorrhage, there was an active arterial extravasation (jejunal branches of superior mesenteric artery) in the anastomosis site between intestinal loops; in addition there was an intra-luminal haematoma.
Most of the complications were treated by spontaneous, surgical and percutaneous interventional procedures, and mortality in the early postoperative period occurred only in the patient that had developed intraluminal haemorrhage and active extravasation. A CT-guided drainage catheter was placed in four patients with abscess formation and in patients with liver abscess. Patients with anastomotic leakage from the gastrojejunostomy line and one of the patients with abscess were surgically treated. No interventional procedures were performed in patients who had fluid collection because there was no clinical suspicion of an infection. In the follow-up of all these patients, the fluid collection was observed to have spontaneously regressed. The remaining five patients with abscess and two patients with haematoma were observed to undergo spontaneous resolution on follow-up CT examination.
Discussion
The Whipple procedure is the only potential curative treatment for periampullary tumours. Two different types of the procedure have been described: classic-conventional and pylorus-preserving. The conventional standard Whipple procedure involves the resection of the pancreatic head, duodenum, and gastric antrum. Furthermore, the gallbladder is always removed and lymph node dissection is performed. Gastrojejunal, choledochojejunal, or hepaticojejunal and pancreaticojejunal anastomoses are also undertaken with the jejunal loops brought up to the right upper quadrant [5]. In the pylorus-preserving type, in addition to these procedures, the gastric antrum is preserved and used for the anastomosis of the duodenojejunostomy of the proximal part. In the literature, no difference was reported between the two types in terms of complication rates [8]. The conventional Whipple procedure had been performed in all cases included in the current study.
The Whipple procedure is complex and arduous because at least three anastomoses are performed and many organs are involved. Therefore, it has high mortality and morbidity rates. Although in the last decade the mortality rates associated with this procedure have been reported to decrease, especially in specialised centres, the morbidity rates remain high [1,4,9].
Computed tomography plays an important role in the diagnosis of postoperative complications. CT can be performed either in two phases, namely arterial (30 s) and portal (60 s), or only in the portal phase. The use of an oral contrast agent is generally not preferred in these patients because it can cause artefacts [1]. In our study, CT had been performed in the portal phase after the administration of an intravenous contrast agent. Oral contrast media was also used in 21 patients with no suspected vascular complications.
In the early CT examination, mild fluid, oedema, and contamination in fat-saturated sequences are common findings and should not be considered as residual or abnormal inflammation. In the superior mesenteric artery (SMA) and SMV, slowing in blood flow or appearances of mass-like images may be detected due to local stasis. These findings should not be evaluated in favour of recurrence or residues, especially in cases with negative surgical margins. In addition, many prominent lymph nodes may be observed in the early period due to inflammation around the operation loop. These lymph nodes should not be considered malignant in the first postoperative CT examination, but they should be carefully monitored in subsequent scans [10]. Knowledge of these conditions that can mimic pathology in the early postoperative process is important in the accurate detection of true pathologies.
Complications detected in CT in the early period include abscesses, fluid collection in the operation site, delayed gastric emptying, pancreatic fistulas, haematoma, anastomosis leakage, portal vein and SMV thrombosis, hepatic abscesses, intraluminal haemorrhage, pancreatitis, and hepatic infarction [11]. None of our cases developed pancreatitis or hepatic infarction, but the remaining complications were seen.
Small collections of fluid in the operation site are often seen postoperatively. They usually do not require interventional procedures and spontaneously regress [5]. However, they predispose patients to infections; therefore, in cases of suspected infections, the fluid can be clinically drained with a needle. Non-drained collections require reimaging if there is greater suspicion of infection. The presence of air in the collection suggests an abscess or fistula [12]. In the current study, eight patients (18%) had a homogeneous fluid collection in the operation site.
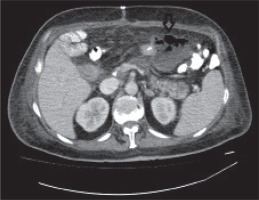
Intraabdominal abscesses may develop secondary to pancreatic fistulas, superinfection of an acute postoperative collection, hepaticojejunostomy, and leakage from gastrojejunostomy or duodenojejunostomy anastomoses. An abscess should be considered in the presence of a cystic lesion with a contrast-enhanced wall and air densities on CT (Figure 1). Ten of our patients (22%) had a secondary abscess formation. In the literature, the rate of abscess formation has been reported to be 6%, independent of the underlying cause [13]. The abscess rate was significantly higher in our patients compared to the literature, which may be because the rates reported in the literature belonged to patients with clinically diagnosed abscesses in contrast to our sample, in which the CT examination revealed small abscesses with no clinical symptoms.
Figure 1
An axial contrast-enhanced abdominal computed tomography image revealing fluid collection located in the anterior of the pancreatic tail on the left midline of the abdomen, containing air densities, consistent with a thick-walled abscess (arrow)
Delayed gastric emptying is one of the most common complications after the Whipple procedure. The diagnosis of this complication is mainly undertaken based on clinical findings. It is defined as the prolonged need for a nasogastric tube for more than 10 days after surgery. The incidence of this complication has been reported to be 11-29% in the literature [14,15]. Although the diagnosis is not primarily based on imaging, the presence of a marked dilated stomach filled with oral contrast material on CT suggests a high probability of delayed gastric emptying. This diagnosis can be supported by fluoroscopic barium examinations and nuclear medicine examinations [1]. The CT findings suggested the presence of delayed gastric emptying in six of our patients (13%), and when we checked their medical records, we found that all had been clinically diagnosed with this condition. In our study, the rate of this complication was similar to the literature [14]. In addition, previous studies reported that complications, such as abscess formation, pancreatic fistulas, and severe intraoperative blood loss are usually associated with delayed gastric emptying [14]. In our study, two of our patients had delayed gastric emptying alone. In another patient, fluid collection was seen in the operation site, and a further two patients developed pancreatic fistulas, of whom one also had an abscess in the operation site.
A pancreatic fistula is another common complication seen together with delayed gastric emptying. These fistulas are also the cause of the highest mortality and morbidity rates among the complications of the Whipple procedure. The incidence of a pancreatic fistula is reported to be 6-14%, and the mortality rate ranges from 1.4 to 3.7% [16]. Pancreatic fistulas are often accompanied by other complications, such as pancreatitis, abscess formation, haemorrhage, and delayed gastric emptying [16]. A generally accepted definition for the diagnosis of a pancreatic fistula is a drain output of any measurable volume of fluid on or after postoperative day 3 with an amylase content greater than three times the serum amylase activity. A grading system was also established, which stratified patients from a relatively benign clinical course (grade A fistula), moderately unwell patients requiring medical or minimally invasive intervention (grade B), and critically ill patients, often with sepsis, requiring invasive intervention (grade C) [17]. The diagnosis of a fistula is made clinically, but a CT examination is performed to detect the possible presence of an accompanying abscess in all diagnosed or suspected fistula cases [18]. In CT, the fistula can present with contamination around the pancreaticoduodenectomy line, fluid in the pancreatic bed, interrupted anastomosis, and air densities in this region [1,18]. In the current study, five patients (11%) had a pancreatic fistula. The complication rate was similar to that reported in the literature [1,16,18]. Four of these patients had an abscess formation, one of whom had additional haematoma and the other had delayed gastric emptying. Thrombosis was present in the single case without an abscess.
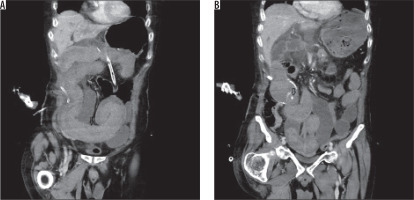
Postoperative haematoma is a rare but well-defined complication with an incidence of 4%. The mortality rates due to haematoma have been reported as up to 38% with statistical significance [19]. It can be classified as early and late haemorrhage. Early haemorrhage is seen within 24 h postoperatively, usually secondary to gastroduodenal artery bleeding and inadequate ligation. Late haemorrhage may develop secondarily to erosion or pseudoaneurysm in mesenteric vascular structures [19]. In this study there were haematomas in two patients and active extravasation and intraluminal haemorrhage in one patient (Figure 2). The follow-up CT images showed spontaneous resorption of haematoma in both haematoma cases, and no intervention was required. However, the patient with active bleeding died.
Figure 2
A) A contrast-enhanced abdominal computed tomography coronal cross-section image of a patient showing increased long-segment wall thickness in the jejunal segment and a significant high-density area (arrow) in favour of intraluminal haemorrhagic material. B) A contrast-enhanced coronal section image of the same patient obtained from a different level, showing a high-density focus in the proximal area that is suggestive of active extravasation (arrow)
Leakage from the gastrojejunostomy line is a rare complication. Although the exact rates have not been determined, the incidence of this complication has been reported to be 0.04% in some studies [20]. The aetiology is considered to be multifactorial, but it has not yet been fully elucidated; however, inadequacies in the surgical technique or impairment of the anastomotic blood supply have been implicated as possible causes of this complication. The presence of fluid collection adjacent to the level of anastomosis on radiological CT and direct extravasation if an oral contrast agent is used may help in the diagnosis [1,5]. In our study, two patients had anastomotic leakage, both of whom were treated surgically and survived.
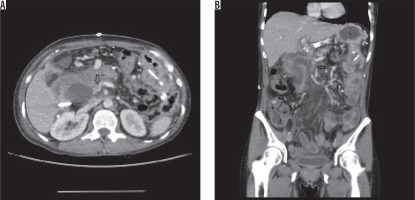
In recent years, with the advances in pancreatic cancer surgery, the definitive distinction between resectable and non-resectable tumours has begun to disappear, and the concept of borderline resectable tumour has emerged. Initially, only the patients without the involvement of SMA, celiac artery, hepatic artery, or portal vein SMV confluence were considered to be resectable. However, with the introduction of the borderline resectable term, the tumour surrounding SMA at less than 180 degrees, those invading the short-segment of the hepatic artery, or those occluding the short-segment of the portal vein and SMV are also considered to be resectable by surgical reconstruction according to NCCN guidelines [21]. All these developments have led to the increased resection of venous vessels and use of grafts. The risk of venous thrombosis has increased in parallel to the higher venous reconstruction rates [22]. It has been reported in the literature that venous thrombosis is seen in 17% of cases, and the more complex the operation, the higher the risk [23]. If not diagnosed and treated properly, venous thrombosis can lead to intestinal ischaemia, hepatic ischaemia, ascites, and eventually death. When diagnosed, the treatment is systemic anticoagulant or surgical thrombectomy [23,24]. SMV thrombosis was present in two of our cases (4.4%), but portal vein thrombosis was not detected in any patient. The thrombosis rates were found to be lower compared with the literature. Both patients were treated with systemic anticoagulants, and no surgical intervention was required. No other complications secondary to SMV thrombosis developed. The detection of thrombosis in CT can be challenging; therefore, not only axial images but also coronal views should be evaluated in detail to detect short-segment filling defects on CT particularly for the evaluation of SMV thrombosis [1,11]. The coronal examination undertaken in this study made a diagnostic contribution in one of our patients (Figure 3).
Figure 3
A) An axial contrast-enhanced computed tomography image of a patient, revealing a significant hypodense area (arrow) in the superior mesenteric vein (SMV) lumen distal to the confluent level in favour of thrombus, accompanied by an immediately adjacent collection on the right side. B) A coronal section image of the same patient, which better demonstrates the presence of long-segment hypodense thrombus (arrow) in SMV
Bile ducts are susceptible to ischemia, and hepatic abscesses or bilomas may develop as a result of any disruption in the integrity of the bile duct due to surgery. A hepatic abscess is best diagnosed by CT using intravenous contrast media. Hepatic abscess treatment is performed according to the patient’s clinical findings, and only antibiotic treatment may be sufficient in small abscesses if the patient’s general wellbeing is good. However, in large abscesses, a sample should be taken from the abscess and drained by an interventional procedure [5]. In the literature, the incidence of hepatic abscesses has not been reported to be frequent, and similarly, in our study, only one patient developed a hepatic abscess, which was treated by catheter placement under CT. After drainage and antibiotherapy, the CT of the patient revealed the resorption of the abscess.
In this study, we evaluated the complications detected on CT in the early period in patients who underwent the conventional Whipple procedure, and we discussed these complications in relation to the literature. Twenty-four of our patients developed complications, and the rate of complications was generally similar to those previously reported. Our rates of pancreatic fistula, delayed gastric emptying, fluid collection, and haematoma were also consistent with the literature. The rate of abscesses was higher in our study group compared to previous research; however, we observed no mortality due to this complication. Our SMV thrombosis rate was lower than reported in the literature. Among all of our cases, the mortality rate was very low, with only one patient dying due to early complications.
There were some limitations of our study. First, the study had a retrospective design. Second, in addition to the Whipple procedure being a complex and very specific surgical method, our sample was relatively small. Studies with a larger patient population can contribute more data to the literature.
CONCLUSIONS
Despite the developing techniques and possibilities, some of the complications specific to the Whipple operation can be detected on CT. In our study, complications seen in CT were fluid collection in the operation site, abscess formation, pancreatic fistula, haematoma, delayed gastric emptying, anastomotic leakage in the gastrojejunostomy line, SMV thrombosis, hepatic abscess, intraluminal haemorrhage, and active extravasation.


