Introduction
Neuroendocrine tumours (NETs) or neuroendocrine neoplasms (NENs) have been defined as inappropriate proliferation of amine precursor uptake and decarboxylation cells. The most common localisation of NENs has been described as lung, gastrointestinal tract, and pancreas [1]. Pancreatic neuroendocrine neoplasms (PNENs) are the second, after pancreatic ductal adenocarcinoma, most common type of pancreatic malignancies, comprising 1-2% of all pancreatic tumours and 7% of all NETs. Nonetheless, PNENs are a rare histopathological diagnosis, but the incidence of PNENs is still growing and is currently estimated to be about 0.32/100,000 people per year, especially due to improvements in diagnostic imaging. PNENs are characterised by different biological functions and can be divided into 2 groups: non-functioning (45-60%) and functioning (40-55%) types. The characteristic of PNEN has an impact on the presented symptoms. Non-functional PNENs are the most insidious changes due to the fact that the symptoms are non-specific. Most of them are detected by accident during the diagnostic process because of other indications when liver metastases are already present. Nevertheless, functional PNENs are easier to diagnose due to the symptoms associated with the secretion of appropriate hormones by tumour cells [2-4]. The functional PNENs group consists of insulinoma, gastrinoma, VIPoma, glucagonoma, and others. The symptoms of functioning PNENs are highly variable and depend on the secreted hormone [5]. They include Whipple triad, dizziness, gastroesophageal reflux disease, diarrhoea, or weight loss [6]. Most functioning PNENs are located in the tail of the pancreas. Despite not numerous symptoms in non-functional PNENs, there are serum markers of NENs including chromogranin A (CgA), pancreatic polypeptide (PP), neuron-specific enolase (NSE), and others [7]. Functioning PNENs are well-differentiated tumours with mild natural history, while non-functioning PNENs are poorly differentiated with a tendency to metastasise, and with worse outcomes [8]. Patients with PNENs have variable prognoses, and there are no studies regarding the median survival rate for a significant group of patients. A study conducted by Ekeblad et al. [9] on 324 patients with PNENs showed a median survival rate of 99 months, and the one-year survival rate was 64%.
The aim of our study was to analyse the histological differentiation and multi-slice computed tomography (MSCT) imaging features of PNENs.
Material and methods
We performed a retrospective cohort study based on the medical history of 157 patients with histologically confirmed pancreatic neuroendocrine tumours, hospitalised in the Department of Endocrinology and Endocrine Neoplasms between January 2016 and January 2022. All data were retrieved from the hospital electronic records (AMMS, Asseco Medical Solutions, Rzeszów, Poland).
There were 2 inclusion criteria: (1) having reached the age of 18 years and (2) complete medical history including results of histopathological examination and MSCT description.
The result of the histopathological examination was based on the material from a core needle biopsy. The Ki-67 index level and grading according to the World Health Organisation (WHO) criteria from 2017 and 2019 were evaluated.
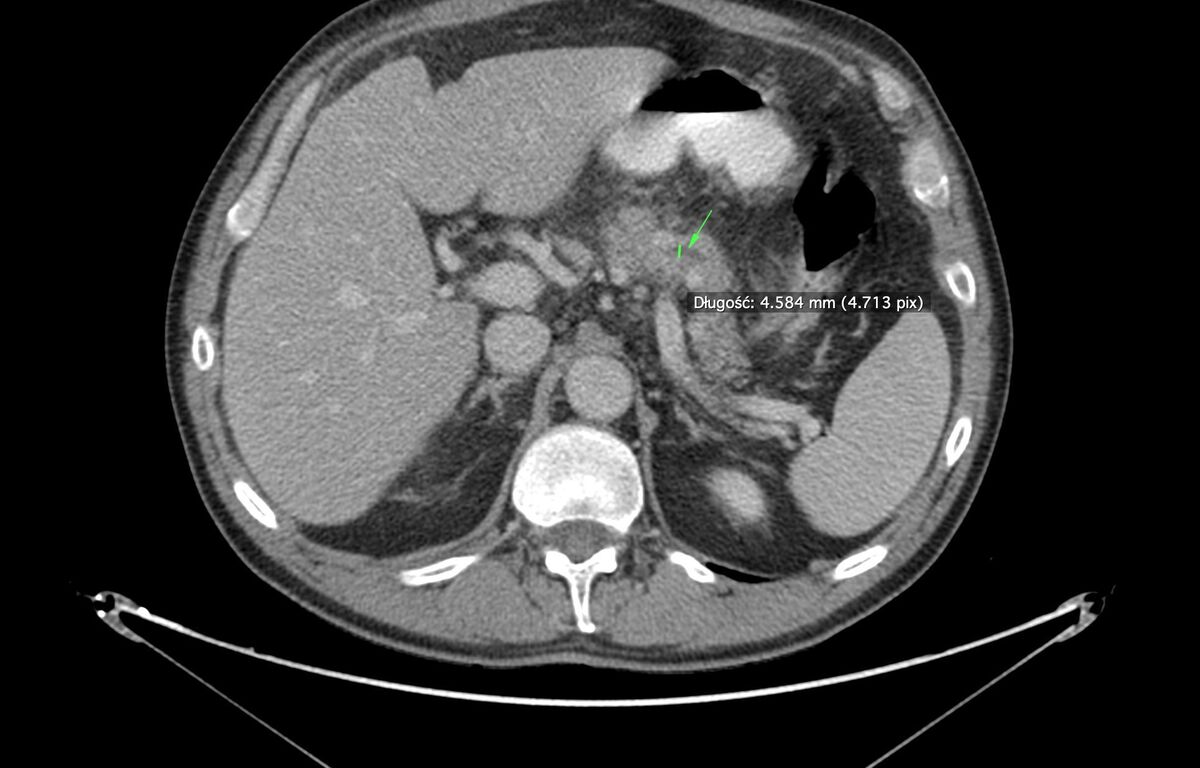
We evaluated selected radiological parameters such as: localisation of the tumour (head, body, or tail of pancreas); infiltration of the liver, the spleen, visceral arteries, the common bile duct, the stomach, and other organs; presence of intraductal papillary mucinous neoplasm, dilatation of the Wirsung’s duct; enlarged intraabdominal lymph nodes; metastases in the liver, the spleen, the lungs, and other organs; and the presence of calcifications, cysts, and hypervascularisation. We divided patients into 3 groups according to the WHO criteria based on the diameter of the tumour – < 2 cm, 2-4 cm and > 4 cm.
All of the MSCT descriptions and histopathological examinations were performed in the same institution. All radiological descriptions were made by a clinician with 30 years of experience in pancreatic pathology imaging.
Statistical analysis
To perform a statistical analysis, we used IBM SPSS Statistics 29 software. To present qualitative variables we used absolute values and percentages. To present quantitative variables we calculated ranges, means, and standard deviations or medians with interquartile ranges. The distribution of the quantitative variables was checked with the Shapiro-Wilk test. We performed between-group comparisons in terms of tumour size, location, and radiological features for 3 groups with different tumour grading (G1, G2, and G3). For univariate analysis we used the chi-square test, Fischer’s exact test, or Mann-Whitney U test. A significance level was set at p < 0.05. Selected variables which appeared to be significant in univariate analysis were included in the multivariable logistic regression model.
Histopathological evaluation
PNENs are mainly solid tumours, pink/red to brown in colour, located in the body and tail of the pancreas, and containing cysts in about 5% [10]. Most of them are less than 2 cm in size and are referred to as small tumours. On the other hand, those with dimensions greater than 2 cm are classified as large, and their metastatic capability increases; however, the size does not correlate with the progression of symptoms in tumours greater than 3 cm [10,11]. The 2019 WHO classification defines pancreatic NENs as neoplasms with significant neuroendocrine differentiation and secreting neuroendocrine markers, and divides them into well-differentiated (PNENs), poorly differentiated (neuroendocrine cancers), and mixed (neuroendocrine-non-neuroendocrine neoplasms) [10,12]. By determining the degree of similarity of neoplastic cells to the cells they derive from and knowing their proliferation potential as measured by the Ki-67 index and/or the rate of mitotic division, PNENs can be assigned with an appropriate grading value on a 3-level scale: G1 – low-grade tumours, G2 – intermediate-grade tumours, and G3 – high-grade tumours [5,12-14] (Table 1).
Table 1
Histological classification of pancreatic neuroendocrine neoplasms – WHO 2019 classification [13]
G1 and G2 lesions consist of small-to-medium-sized cells that show little atypia with retained cell structures. The nuclei are centrally located giving the image of “salt and pepper”. In addition, the presence of amyloid is characteristic of insulinoma while somatostatinomas are more glandular with the presence of sandy bodies. Tumours classified as G3 show a high degree of cell division and atypia. However, it should be noted that the differentiation of G3 PNENs from neuroendocrine carcinomas, which are by definition high-grade lesions, is difficult but necessary to implement appropriate treatment [10,12]. Similarly to many cancers, the TNM score also applies here [14].
Radiological evaluation
The detectability of PNENs largely depends on their size [14]. Due to the quickness, availability, and accuracy of the contrast MSCT scan, it is the diagnostic tool of choice [15,16]. MSCT is used to detect primary neoplasms and metastases, and it enables the diagnosis of non-functional PNENs [17]. PNENs are usually visible as a well-vascularised, round, compact mass that shows enhancement in the arterial phase after contrast administration, and cysts are found in approximately 10-17% [10,18]. G1-grade PNENs show significantly higher tissue blood flow than G2 and G3 graded ones, and therefore they exhibit stronger contrast enhancement in arterial and venous phases compared to those with G2 and G3 grades [19]. Weak contrast enhancement is observed in PNENs with G3 grade [20]. In G1 PNENs, significantly greater contrast enhancement is observed in the parenchymal and portal phases compared with G2 PNENs [21]. The arterial enhancement ratio (AER) and portal enhancement ratio (PER) have the highest values for G1 PNENs. These values are lower for lesions in G2 grade than in the case of G1. The lowest values of AER and PER are noted in PNENs with G3 grade [20]. The analysis of computed tomography (CT) texture parameters such as average grey intensity, kurtosis, and the degree of entropy differs significantly between G1, G2, and G3 PNEN lesions and can be used to differentiate them [22]. Calcification is rarely seen unless the lesion is malignant [23]. MRI has a similar application in the detection of primary lesions but is better suited for the diagnosis of liver metastases [17]. In the T1 sequence, the changes are low-signal while they are high-signal in T2. Gadolinium contrast helps highlight richly vascularised lesions. The diffusion-weighted imaging (DWI) sequence allows us to visualise even small metastatic changes as areas of high signal diffusion restriction [12,24]. On the other hand, endoscopic ultrasound (EUS) enables the detection of almost 100% of PNENs and is characterised by the ability to detect changes in size as low as 2-3 mm, and it gives a chance to collect biopsy material [17]. Insulinoma in the EUS image is a well-defined homogeneously hypoechoic lesion visible in the background of the pancreatic matrix. However, this method does not allow for the assessment of the malignancy of the neoplasm and is also not precise in the case of large tumours [21]. The methods of nuclear diagnostics include imaging of somatostatin receptors (SRI) in the tumour [17]. Currently, somatostatin receptor scintigraphy has been replaced by positron emission tomography using 68Ga-POSITIVE – PET-TK with 68Ga as the SRI method of choice. It is useful in the diagnosis of small metastases to the lymph nodes and bones [12]. There are also SRIs using F-18 fluorodeoxyglucose, but this test is less sensitive [4].
Results
We analysed 157 patients with diagnosed PNENs. Tumour size and location are presented in Table 2.
Table 2
Size and location of pancreatic neuroendocrine tumors in multi-slice computed tomography depending on the degree of histological differentiation
Tumour size was different in histological differentiation while its localisation was not.
MSCT features and its frequency are presented in Table 3.
Table 3
Radiological features in multi-slice computed tomography and their frequency in pancreatic neuroendocrine tumors depend on histological differentiation
Enhancement in arterial phase (p = 0.032), dilatation of the Wirsung’s duct (p = 0.001), infiltration of other organs (p < 0.001), distant metastases (p < 0.001), enlarged regional lymph nodes (p = 0.018), and hypervascularisation (understood as the pathological network of blood vessels of the tumour) (p = 0.032) were significant in histological differentiation, while the infiltration of common bile duct (p = 1.000), vessels (celiac trunk in particular) (p = 0.051), calcifications (p = 0.850), and cysts (p = 0.766) were not.
The results of logistic regression for features of selected tumours in the MSCT scan are presented in Table 4.
Table 4
Multi-slice computed tomography (MSCT) features and risk of higher grading – multivariable analysis and logistic regression
The risk of the tumour having histological malignancy grade G2 or G3 was increased in the case of infiltration of other organs (OR 3.1; 95% CI: 1.21-8.06; p = 0.019), distant metastases (OR 3.9; 95% CI: 1.44-10.61; p = 0.008), and for tumour size ≥ 2 cm (OR 2.7; 95% CI: 1.21-6.24; p = 0.016).
Discussion
The size of the tumour is important when deciding whether to surgically remove the lesion because if greater than 2 cm, it should be removed due to a higher risk of metastasis [11]. Tumour diameter in MSCT has been shown as a promising method of prediction of grading especially in PNENs with worse prognosis such as those graded G2/G3 [21]. The size of the tumour can also be assessed in B-mode ultrasonography with the same predictive value [22]. MRI is also a useful tool to evaluate the level of aggressiveness in PNENs [23]. Tumour margin or tumour enhancement may be of use to define PNEN grading as well as local invasion, metastases, and infiltration of vessels. Ill-defined margin, larger tumour size, and hypoenhancement pattern in the arterial phase are more common for high-grade tumours. Moreover, several parameters in T2 and DWI sequences can help evaluate the grading of the tumour. The following parameters are mentioned for the T2 sequence: inverse difference moment, energy, correlation, and difference entropy, while for the DWI sequence correlation, contrast, inverse difference moment, maximal intensity, and entropy are of use [24].
In our study, the tumour size in MSCT varied depending on its grading. 37.2% of the tumours with diameter > 40 mm were assessed as G1 while 62.8% were defined as G2+. 43.6% of G2+ tumours had the size of over 40 mm. Despite tumour size varying between individual staging categories, no parameter affected a localisation of the primary lesion (Table 2). It is worth noting that over three-quarters of the lesions were found in only one region of the pancreas (head, body, or tail), with the head being the most clinically important site and the body and tail being the least frequent sites. One-third of the lesions were located in the head of the pancreas, allowing for the potential performance of a pancreaticoduodenectomy when tumours are resectable. Meanwhile, the remaining lesions were located in the body and tail, which implicates a less burdensome management involving a peripheral resection of the pancreas.
Some of the factors that may affect the probability of achieving R0 resection need to be discussed. Infiltration to adjacent organs was present most frequently in patients with G2 and G3 tumours, compared to G1 (40.3% vs. 9.4%, p < 0.001), with the stomach as the most common site of infiltration. Similarly, the infiltration of vessels (mainly celiac trunk) was confirmed more frequently in G2 and G3 tumours in comparison to G1; however, this relationship was insignificant (19.4% vs. 8.3%, p = 0.051). Compared to G1, enlarged lymph nodes were more often confirmed in G2 and G3 tumours (27.4% vs. 12.5%, p < 0.018). Infiltration of adjacent organs and vessels as well as the presence of enlarged lymph nodes in G2 and G3 tumours can significantly contribute to decreased probability of radical surgery. A significantly dilatation of the Wirsung’s duct in G2 and G3 compared to G1 lesions (27.4% vs. 8.3%, p < 0.001) has also been found. As the data show, the dilatation of the Wirsung’s duct may be responsible for the increased formation of postoperative pancreatic fistula in patients with periampullary malignancies [25]. Similarly, the preoperatively assessed dilatation of Wirsung’s duct may be inherent to increased postoperative morbidity in patients with PNENs [26].
Calcification and the presence of cysts were not significant, as statistical analysis revealed. Distant metastases were also evaluated. Over 30% of the described PNENs showed secondary lesions in the liver, which is consistent with the literature [27,28]. Most of them were staged as G2 while G3 PNENs were detected the least frequently. We decided to divide the localisation of tumours into 2 main areas: the head, and the body and the tail together due to the possibility of performing peripheral resection in the latter case.
Due to the rich vascularisation, PNENs present enhancement in the arterial phase after contrast administration [2]. Arterial enhancement and dynamic washout correlate with the tumour [29]. In our study most of the tumours were hyperdense (79.6%). This pattern was also noticed across all staging categories. It is worth pointing out that the enhancement in arterial phase was significantly more frequent in G1 tumours compared to G2 and G3 (85.3% vs. 71%).
Disease progression can be foreseen using Ki-67 [30]. Enhanced CT may predict Ki-67 index. Yu et al. [31] found that nonmetastatic PNENs with larger diameter, ill-defined margin, distal main ductal dilation, and weak enhancement of the tumour in arterial phase in preoperative enhanced CT tend to have a Ki-67 index of > 5%. This may be useful to predict potential surgical resection.
There are some data suggesting that analysis of enhancement patterns may provide predictive information about whether endoscopic ultrasound-guided fine-needle aspiration biopsy is reliable for the assessment of the Ki-67 index. Additionally, PNENs in which less than half of the tumour showed a washout pattern were correlated with poor prognostic factors [32]. In our study, some radiological features like enhancement in arterial phase, dilatation of Wirsung’s duct, infiltration of other organs, distant metastases, enlarged regional lymph nodes, and hypervascularisation may predict the histopathological result, which is also correlated with poorer prognosis. The likelihood of the tumour displaying histological malignancy grades G2 or G3 tripled when there was infiltration of other organs, nearly quadrupled in the presence of distant metastases, and almost tripled for tumours with a size of 2 cm or more.
Certain MSCT characteristics are linked to histological differentiation, including enhancement during the arterial phase, Wirsung’s duct dilatation, organ infiltration, distant metastases, and the enlargement of regional lymph nodes. In cases of organ infiltration, the risk of the tumour having histological malignancy grades G2 or G3 is 3 times greater than when the infiltration is absent. Similarly, the presence of distant metastases raised the risk nearly fourfold, while tumour size equal to or greater than 2 cm was associated with an almost threefold increase in the risk of histological malignancy grades G2 or G3.
Limitations
Due to the retrospective nature of this study, there are some limitations. Firstly, it was impossible to assess the correlation with Ki-67 or histological differentiation with prognosis and results of treatment due to loss of data. Secondly, we compared the pre-operative Ki-67 index. We did not have access to the postoperative Ki-67 index level.