Introduction
Coronavirus disease 2019 (COVID-19) is a novel new type coronavirus of zoonotic origin with human-to-human transmission that was officially named by the World Health Organisation (WHO). The first reported cases were in Wuhan, Hubei province, China, which then disseminated all over China and later to other countries across the world that fear to have the potential to cause a pandemic. This infection originated in a wet “seafood market” in Wuhan, and it has a mean incubation period of 5.2 days. These patients suffer from severe pneumonia, in the form of fever, fatigue, dry cough, and respiratory distress [1-10]. Chest computed tomography (CT) and plain X-ray play a crucial role in the detection of early pulmonary changes and surveillance of patients with COVID-19. Several recent studies discuss the role of chest CT and X-ray in COVID-19 infection [11-33].
The aim of this study is to review the basic background and chest CT imaging findings in patients with COVID-19 infection.
Epidemiology
Coronaviruses are non-segmented, enveloped, single-strand viruses, with four mild species present with mild respiratory symptoms, and three severe forms called severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and the more recently identified coronavirus disease 2019 (COVID-19), which cause epidemics with high mortality rates. Different varieties of Coronaviruses are seen in bats, which are considered reservoirs for several viruses [1-5]. COVID-19 is assumed to be primarily hosted by bats, and then transmitted to humans through pangolin or other wild animals sold at the Wuhan seafood market with subsequent transmission from humans to humans. The incubation period infected with COVID-19 ranged from 3 to 7 days and up to 14 days. Patients can become the source of infection in the incubation period; therefore, early detection of infected patients is beneficial to control the spread of infection. The fatality rate is about 2.3%. The average number of new infections from an infected patient to a naïve population is 3.28, indicating that this disease will spread according to WHO rules [4-9].
Clinical presentation
The clinical presentation of patients with COVID-19 is non-specific including fever (98%), cough (75%), and myalgia or fatigue (45%), dyspnoea (55%), and acute respiratory distress syndrome (20%) and may progress to multiorgan dysfunction (e.g., shock, acute respiratory distress, acute cardiac dysfunction, acute kidney dysfunction) and even death (2.5%) [4-10].
Laboratory
The real-time reverse transcription-polymerase chain reaction (RT-PCR) assay is considered now as the gold-standard for diagnosis of COVID-19. However, this test may be associated with false-negative results from sampling errors and low-virus overload, not widely available, expensive, takes a long time for analysis and must be check by skilled personnel, while antibody-based techniques are used as supplemental tools [2-7].
Computed tomography findings
Imaging findings of COVID-19 at CT can be classified into pulmonary findings (Table 1) and extra-pulmonary findings (Table 2).
Table 1
Pulmonary findings in COVID-19
Table 2
Extra-pulmonary findings in COVID-19
Pulmonary findings
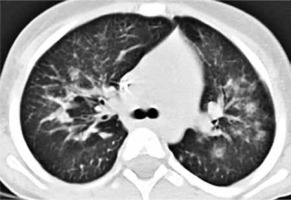
Ground glass opacity
Ground glass opacity (GGO) is described as hazy areas with slightly increased density in the lungs, but with unobscured bronchial and vascular margins. This is attributed to the partial filling of alveoli by exudate and alveolar septal inflammation. GGO is the most widely reported radiological sign linked to COVID-19. It is considered one of the earliest signs to appear in CT in the pre-clinical group (asymptomatic) and extends to predominate in the second and third weeks as well. GGO in COVID-19 has a characteristic distribution being peripheral (subpleural), often bilateral, multifocal, possibly nodular or mass-like, and predominantly affecting lower lung lobes. The last feature could be explained by the fact that diseased patients are likely to move less and prefer to lie down, so they develop radiological changes in the most dependent areas of the lungs. Extensive bilateral diffuse GGO (also named bilateral white lungs) is noted in severe cases that may require admission to the intensive care unit (ICU) and intubation [11-16] (Figure 1).
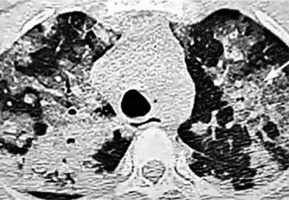
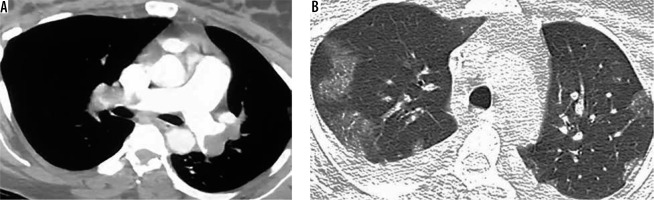
Figure 1
Ground glass opacity (GGO). A) High-resolution computer tomography (HRCT) shows GGO with air bronchogram at the posterior segment of the right upper lung lobe with thickening of the oblique fissure. There is inter- and intralobular septal thickening overlying the GGO at the anterior segment of the left upper lung lobe crazy paving (black arrow). B) HRCT shows bilateral diffuse extensive GGO (white lung sign) with air bronchogram and small consolidation at the posterior basal segment of the left lower lung lobe
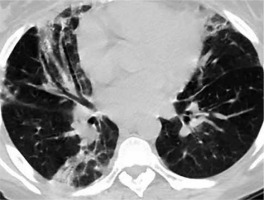
Consolidation
Consolidation is defined as a homogenous high density that obscures airway walls and blood vessels. In this condition, alveolar air is replaced by other materials (e.g. pathological fluids, cells, or tissues) with subsequent increase in pulmonary parenchymal density. It has bilateral, multifocal, and subsegmental distribution. The presence of consolidation is considered a sign of progressive COVID-19 disease, as it develops in the second week after the onset of symptoms. It is seen more in patients over 50 years old, so consolidation could serve as a clue of an illness that necessitates greater vigilance in management [13-19] (Figure 2).
Mixed ground glass opacity and consolidation
GGO is accompanied by focal, round, small areas of consolidation, which may suggest organising pneumonia. It is a sign of the progress of viral infection. It is found in about 2/3 of cases of COVID-19 [11-15] (Figure 3).
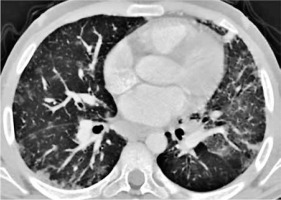
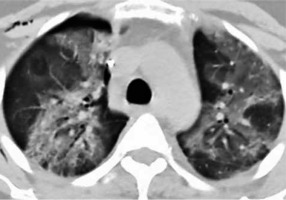
Figure 3
Mixed ground glass opacity (GGO) and consolidation. High- resolution computer tomography shows bilateral multiple multifocal peripheral and bronchocentric consolidations mixed with GGO, together with thick septations giving crazy paving appearance. Note small consolidation developing within GGO (white arrow)
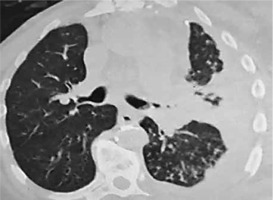
Crazy paving
Crazy paving is defined as ground-glass opacity superimposed by inter – and intra-lobular septal thickening, resembling stone paving. Like SARS, this pattern may be caused by two events occurring in the same time, alveolar oedema (causing GGO) and interstitial inflammatory reaction (causing septal thickening); both are caused by acute lung injury. The presence of crazy paving in combination with GGO and consolidation is considered another sign of progression of COVID-19 infection. There is large variability in the prevalence of this sign, ranging from 35 to 90% [18-25] (Figure 4).
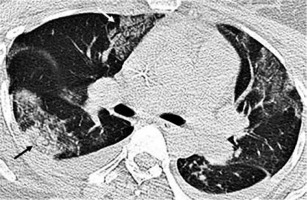
Figure 4
Crazy-paving sign. High-resolution computer tomography shows bilateral multifocal ground glass opacity (GGO) located at medial segment of the right middle lung lobe, apical segment of the right middle lung lobe and superior lingula superimposed by thickened inter and intralobular septations (crazy paving) (white arrow). It is associated with peripheral consolidation (black arrow) developed within GGO and bilateral pleural effusion
Halo sign
Halo sign is defined as ground-glass opacity around a pulmonary nodule. This pattern was noted for the first time in immune-compromised patients with invasive pulmonary aspergillosis. The peripheral halo of ground-glass opacity is linked to the presence of haemorrhagic nodules, and the mechanism of the haemorrhage may include haemorrhagic infarction, vasculitis, the fragility of the neovascular tissue, broncho-arterial fistula, or necrosis. Hence, the central dense zone corresponds to the nodule, while the surrounding halo of ground-glass opacity corresponds to haemorrhage/haemorrhagic infarction. This sign is seen in several infectious diseases such as varicella-zoster, cytomegalovirus, herpes simplex, and myxovirus. This sign is also described in COVID-19 infection; one recent study found it in 64% of their cases [18-26] (Figure 5).
Reversed halo sign
Reversed halo sign (atoll sign) is defined as a rounded area of ground-glass opacity surrounded by a complete or almost complete dense ring (more than 3/4 of a circle) of consolidation, at least 2 mm in thickness. The central low-density area (GGO) represents alveolar space opacification by alveolar septal inflammation and cellular debris, while the dense crescent is formed by granulomatous tissue within the distal air spaces. Reversed halo sign was originally described in cryptogenic organizing pneumonia but can also be secondary to other causes. It is infrequently reported in COVID-19 patients, and it is more commonly described in moderate disease than in severe disease. Most lesions are peripheral, located in lower lobes, while their rim is more often smooth than irregular. On follow-up these lesions are resolved in the majority of cases into GGO and linear fibrotic bands [23-29] (Figure 6).
Centrilobular nodules and tree in bud pattern
Pulmonary nodule is defined as a rounded opacity that might be well or poorly defined and can be up to 3 cm in diameter. Pulmonary nodules are classified according to distribution into centrilobular, peri-bronchovascular, and random. The presence of centrilobular nodules is a rare radiological sign in COVID-19. It is considered one of the unlikely signs in several score systems [27-30] (Figure 7).
Figure 7
Centrilobular nodules. High-resolution computer tomography shows multiple centrilobular nodules at the right middle lung lobe. There are also a few small peripheral consolidations at the apical segment of the right lower lung lobe as well as the superior lingula, ground glass opacity at the superior lingula with thick interlobular septations, and right pleural thickening
Air bronchogram
Air bronchogram is defined as a pattern of air-filled (low density) bronchi on a background of opaque (high density) airless lung. Based upon the autopsy report, it is now clear that low attenuation is a gelatinous mucous, not air. Air bronchogram could be seen within ground opacity or consolidation. Air bronchogram is noticed in the asymptomatic and rapid progressive groups. There is great variability in the incidence of air bronchogram in COVID-19 patients ranging from 7 to 68.6% [17-21] (Figure 2).
Air bubble sign
Air bubble sign, also called round cystic changes. It describes a small air-containing space (low density) in the lung parenchyma. It could be attributed to pathological dilation of a physiological space or a cross-section of the bronchiectasis, or simply associated with the process of consolidation resorption, because infection causes damage to the alveolar walls and leads to pneumatoceles [22-28] (Figure 8).
Subpleural curvilinear opacity
Subpleural curvilinear lines are 1-3 mm in thickness, lying parallel to the pleural surface about 1 cm or less from the pleura. Subpleural linear opacity is seen up to 20.8% of COVID-19 patients, and this finding is not specific for COVID-19 [22-27].
Reticulation pattern
Reticulation pattern defined as a thickening of the interstitial structures like inter – and intra-lobular septations (stripe-like opacities). The formation of reticulations is associated with interstitial lymphocyte infiltration. It increases with the progress of the disease. The incidence of reticulation pattern in COVID-19 ranged from 50 to 80% [14-19] (Figure 9).
Figure 9
Reticulations and fibrosis. High-resolution computer tomography shows multiple bilateral reticulations (stripe sign) at posterior basal segment of the right lower lung lobe, fibrotic band at the posterior basal segment of the left lower lung lobe associated with small consolidation at the inferior lingua with air bronchogram

Fibrosis
Fibrosis defined as linear dense peripheral opacities, parenchymal bands, and irregular interfaces. Some authors consider traction bronchiectasis as part of fibrotic changes. It is seen more in severe cases and appears in the second week after the beginning of symptoms indicating interstitial disease. A recent study found that older patients with severe illness are more likely to develop fibrosis. However, the relation between fibrosis and prognosis of the disease is debatable because it is considered as a good prognostic sign with stabilising disease status by some researchers, while others suggest that fibrosis is a bad prognostic sign as patients progress to peak stage with further development of pulmonary interstitial fibrosis [23-31] (Figure 9).
Extra-pulmonary findings
Bronchiectasis
Bronchiectasis is defined as bronchial dilatation in comparison to the nearby pulmonary artery (signet ring sign), lack of tapering of bronchi, and identification of bronchi within 1 cm of the pleural surface. It is assumed that bronchiectasis occurs due to interstitial infiltration and fibrotic changes that occur later as the disease progresses. Bronchial deformity denotes irreversible damage, which may affect the respiratory function of the patient. The appearance of bronchiectasis is seen in the second week of infection with COVID-19. Bronchial wall thickening may persist after healing and resolution of symptoms. Bronchial dilatation and traction bronchiectasis are reported in COVID-19 from 11 to 55%. This variation could be explained by the fact that different studies assess patients at different stages of the disease, mostly during the initial mild form, while bronchiectasis is associated more with severe form [15-26] (Figure 10).
Vascular enlargement in the lesion
Vascular enlargement in the lesion is defined as the dilatation of pulmonary vessels within and/or around the lesions. Several researchers reported high incidences of vascular enlargement in COVID-19 ranging from 70 to 80%, might have been caused by an acute inflammatory response with damage and swelling of the capillary wall. It should be differentiated from vascular changes seen with malignant infiltration by tumours such as bronchogenic adenocarcinoma, which is characterised by irregular vascular dilatation and vascular convergence [19-28] (Figure 11).
Figure 11
Vascular enlargement. High-resolution computer tomography shows enlarged pulmonary vein passing within ground glass opacity at the medial segment of the right middle lung lobe (vascular enlargement sign) black arrow. It is associated with consolidation at the apical segments of both lower ling lobes
Pulmonary embolism
There is an increasing incidence of pulmonary embolism reported in patients suffering from COVID-19 (26-30%). This was attributed either to prolonged stay in ICU with subsequent formation of deep vein thrombi or due to a hypercoagulability state because many cases had PE in their initial assessment [34,35] (Figure 12).
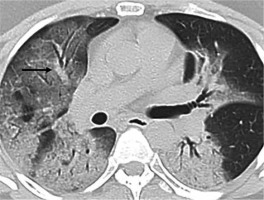
Figure 12
Pulmonary embolism. A) Computed tomography angiography pulmonary artery shows a hypodense filling defect in both pulmonary arteries (extensive pulmonary oedema). B) The same patients showed typical signs of COVID-19; high-resolution computer tomography shows bilateral multifocal subpleural ground glass opacity superimposed with thickened inter and intra-lobular septations (crazy paving) and bilateral pleural effusion, more on the right side
Mediastinal lymphadenopathy
Mediastinal lymphadenopathy is defined as enlarged mediastinal lymph nodes with short axis more than 10 mm. It is described as a rare finding in COVID-19, is seen in a severe group. The associated mediastinal lymphadenopathy, pleural effusion, and nodules indicate secondary bacterial infection [36,37] (Figure 13).
Pleural thickening
Pleural thickening either unilateral or bilateral is noted in about 32% of patients in the third week after the onset of infection. It is associated with a more aggressive form of the disease as it is associated with extensive adhesions in an autopsy.
Pleural effusion
Pleural effusion several studies have reported an absence of pleural effusion in COVID-19 cases. Other researchers have reported the presence of pleural effusion in a minority of cases. Effusion is associated with a severe form of the disease that needs ICU admission or even ends with death. The occurrence of pleural effusion in patients with similar viral diseases such as MERS-CoV or avian influenza H5N1 is a poor prognostic sign [11-17] (Figure 14).
Chest wall
Surgical emphysema and pneumothorax are critical signs that are rarely described in COVID-19 patients, unlike other similar viral diseases (SARS). It is postulated that repeated cough and alveolar damage could be the cause. However, mechanical ventilation might be another causative factor [12-19] (Figure 15).
Figure 15
Surgical emphysema. High-resolution computer tomography shows small right pneumothorax, subcutaneous surgical emphysema, with bilateral multifocal peripheral ground glass opacity
Finally, it is of great importance to highlight that normal CT of the chest does not exclude infection with COVID-19 as reported by many studies, especially in the first few days of infection [11-22].
Paediatric chest computed tomography findings
Chest CTs in children with COVID-19 infection show characteristic consolidation with surrounding halo sign due to underlying co-infection associated with increased calcitonin. These imaging findings are different from adults with COVID-19. Another difference is that children show generally milder form of lung affection with less multi-lobar involvement, less bilaterality, and rapid resolution [38,39].
Discussion
Classification and rational
Different designs are proposed for structured reporting of COVID-19; all agree on the definition of typical radiological findings of typical COVID-19-related pneumonia and non-COVID-19-related pneumonia, but they have some differences regarding the definition of probable, atypical, or indeterminate features. The aim of structured reporting is to help radiologists to identify specific radiological features related to COVID-19, unify languages and terms, increase confidence in repots, and reach a better understanding of radiological reports by referring physicians.
An Italian group classified radiological signs of COVID-19 into three categories based on their experience with 702 patients. Category 1, which is negative for COVID-19, includes cases with no radiological signs suggestive of pneumonia or those who have signs specific for other types of pneumonia as viral and tuberculosis. About 5% of patients who are negative for signs of pneumonia show typical signs of COVID-19 after one week. Category 2is indeterminate for COVID-19, which includes cases showing radiological signs that could overlap or put as differential diagnosis with other types of pneumonia. Category 3 is typical COVID-19, which shows bilateral GGO/consolidation in characteristic distribution. Categories 2 and 3 are further subdivided into mild and moderate/severe according to the severity [40] (Table 3).
Table 3
Italian radiological signs determining the severity of COVID-19
British Society of Thoracic Imaging (BSTI) suggested another reporting system composed of four categories. Classic COVID-19 shows GGO ± consolidation in characteristic distribution. Probable COVID-19 shows a lower lobe mix of bronchocentric and peripheral consolidations or scarce GGO. Indeterminate COVID-19 shows signs that do not fit into classic, probable, or non-COVID. Non-COVID (atypical) signs include lobar pneumonia, cavitation, centrilobular nodules, pleural effusion, lymphadenopathy, and established pulmonary fibrosis [41] (Table 4).
Table 4
British Society Thoracic Imaging reporting of COVID-19
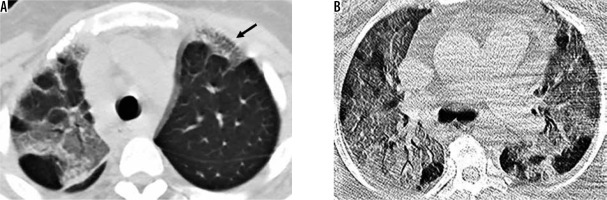
The Radiological Society of North America (RSNA) reporting system is the most commonly used and applied approach, they suggested four categories: typical (specific signs; GGO ± consolidation in a characteristic distribution) (Figure 16); indeterminate (signs reported in COVID pneumonia but not specific enough, GGO lacking specific distribution, not rounded, and not peripheral) (Figure 17); atypical (signs uncommon with COVID-19 pneumonia but specific to other types of pneumonia, lobar consolidation, centrilobular nodules, cavitation, pleural effusion with reticulations); and negative for COVID pneumonia. It shares some similarities with the BSTI classification, but each has a different nomination for the same characters (atypical features in RSNA = non-COVID in BSTI). In addition, the RSNA classification provides a suggested reporting language in order to make it easier for clinicians to understand radiological terms. They mentioned that the decision to use the term COVID-19 in reports depends on several factors including suspicion for the infection, the prevalence of COVID-19, and institutional preferences, because describing a case as COVID or non-COVID would definitely narrow management options for the referring physicians [42] (Table 5).
Figure 16
Classic COVID. A, B) Bilateral peripheral multifocal ground glass opacity + crazy paving + reversed halo sign (arrow) + peripheral consolidation (moderate form)
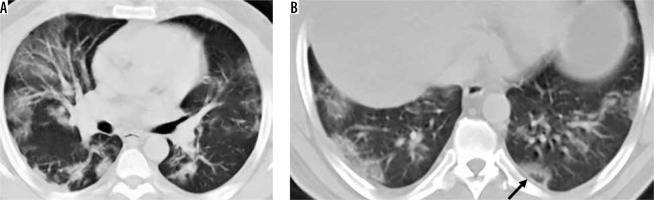
Figure 17
Indeterminate COVID. A) High-resolution computer tomography (HRCT) shows bilateral broncho-centric consolidation and reticular pattern (stripes), presence of reticulations suggests moderate form. B) Another patient HRCT shows bilateral peri-lobular and broncho-centric consolidations
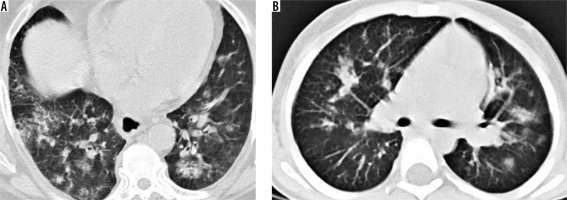
Table 5
Structured reporting of COVID-19 according to RSNA and thoracic society
The Dutch Radiological Society proposed a grading scale of the degree of suspicion of COVID-19 pneumonia ranging from low suspicion (Co-RAD 1) to high suspicion (Co-RAD 5) according to CT radiological findings. Co-RAD 0 is given if the image quality is insufficient for diagnosis. Co-RAD 1 means very low suspicion and is equivalent to non-COVID pneumonia in RSNA classification. Co-RAD 2 represents a low level of suspicion of COVID pneumonia; it is equivalent to atypical COVID in the RSNA classification. Co-RADS 3 is equivalent to indeterminate in the RSNA classification; it includes perihilar ground-glass, homogenous extensive GGO ± sparing of some secondary pulmonary lobules, GGO with smooth inter-lobular septal thickening ± pleural effusion, and small GGO that are not centrilobular and not lying near the visceral pleura. It also includes patterns of consolidation coping with organising pneumonia. Co-RAD 4 represents a high degree of suspicion with GGO that is either unilateral, in a peri-broncho-vascular distribution, or superimposed with pre-existing lung disease. It is equivalent to indeterminate in RSNA classification. Co-RAD 5 represents a very high degree of suspicion with GGO in peripheral bilateral multifocal distribution; it is equivalent to typical COVID pneumonia in RSNA classification. If the patient had positive RT-PCR at the time of examination, it is graded as Co-RAD 6. This scale is designed for regions with a high prevalence of COVID-19 infection. Co-RAD 1 has high negative predictive value (for patients complaining of 4d or more), Co-RAD 5 has very high positive predictive value, while Co-RAD 2-4 shows variable predictive values and low interobserver agreement [43] (Table 6).
Table 6
CO-RAD scale
The role of chest computed tomography in COVID-19 management
Early detection in relation to a serological test
The CT findings may be seen in patients with clinically suspicious but without positive RT-PCR; however, a normal CT scan of the chest is not considered exclusion of infection with COVID-19 [24-27]. The RT-PCR test for COVID-19 has high specificity and low sensitivity (60-70%). The detection rate of the initial chest CT (98%) is significantly higher (p = 0.001) than RT-PCR (71%) in patients with COVID infection [46].
Classification and staging
Researchers have described the progress of the disease in patients with COVID-19 into four stages [8-13]. Earlystage (0-4 d) – CT findings show focal GGC and/or consolidation (40%), multifocal lung opacity (40%) with peripheral predominance (50%). Middle stage (5-13 d) – CT shows progressive disease with a crazy-paving pattern (20%) and new or increasing consolidation with bilateral and multi-lobar involvement (85%). Late-stage (14 d or more) – CT shows varying degrees of clearing without complete resolution. A long-term sequel is fibrotic changes that include reticulations, inter-lobular septal thickening, and/or traction bronchiectasis [47,48].
Disease severity and guide to therapy
CT scan of the chest can be used to assess the severity of involvement of the lungs by COVID-19 in order to guide patient management. Patients with severe form manifested by the presence of bilateral multiple lobular and subsegmental consolidation need to be admitted to the ICU, while patients with a mild form of the disease with bilateral GGO and subsegmental consolidation do not require ICU administration. Patients with severe form with diffuse heterogeneous consolidation with GGOs involving most of both lungs associated with bronchiectasis, presenting as “bilateral white lung”, usually need a ventilator [49,50].
Surveillance with the response to therapy
Patients are treated with antiviral, anti-inflammatory drugs, and antibiotic therapy. CT of the chest could be a valuable tool to assess disease regression in the form of a decrease in number and size of pulmonary consolidation or conversely to demonstrate disease progression with the appearance of crazy-paving and increase in size and number consolidation [14-19]. However, more studies are needed to determine the best time interval for follow-up and consensus from societies of chest and radiology for the protocol of management and surveillance of these patients [30-32].
Prediction of secondary bacterial infection
The presence of pleural effusion, multiple tiny lung nodules, and mediastinal lymphadenopathy are suggestive of overlying bacterial infection, which occurs in 15% of hospitalised patients. The presence of the overlying infection has a serious effect and necessitates the start of an aggressive course of antibiotics [13-19].
Differentiation from simulating lesions
Unfortunately, most of the CT findings of COVID-19 are non-specific and might overlap with other viral pneumonia like influenza, as well as other coronaviruses diseases such as SARS and MERS. The involvement of both lungs at the initial study is highly suggestive of COVID-19 compared to MERS and SARS, which are unilateral. In MERS (similar to COVID-19) the mean number of lung segments involved is higher in the mortality group than in the recovered group, and pleural effusion correlates with a poor prognosis. Some types of viral pneumonia (especially influenza pneumonia) show radiological features that may be identical to COVID-19. However, COVID-19 shows GGOs that are more peripheral than central and more reticular in pattern as well as vascular enlargement, less pleural effusion, and less lymphadenopathy. Heart failure could share similar features as COVID-19 but it shows GGOs of central and stepped distribution with more vascular enlargement sign and rapid improvement after effective treatment [51,52].
Screening with prevention and control
Although most radiology societies do not recommend the use of chest CT as a routine screening for the detection of COVID-19 pneumonia, it can be used in certain occasions to screen patients with clinical signs suggestive of COVID-19 in order to take rapid measures such as early isolation and early treatment, and to control the outbreak using public health strategies. Hence, chest CT plays a role in the prevention and control of the disease. Radiologists better to prepare for a pandemic of COVID-19 all over the world [12-16].
Other imaging modalities
Plain radiology
Plain radiography shows GGGs that are mostly bilateral, peripheral, multifocal, and with lower lobe predominance, but it is less sensitive than CT (69%). Consolidation, on the other hand, unlike CT, is the most common radiological finding in X-ray of patients with COVID-19. Pleural effusion is found in a minority of cases (3%) [53-55].
Chest ultrasound
Chest ultrasound shows various B-line patterns including bilateral focal, multifocal, or confluent thickening attributed to either interlobular septal thickening or hazy opacities that do not obscure the bronchial structures or lung parenchyma. Consolidations in a variety of patterns, including multifocal small, non-translobar, translobar with occasional mobile air bronchograms, thickening, and irregularity of subpleural lines, are reported in patients with COVID-19. The A-lines develop during the recovery phase [56,57].
Advanced computed tomography techniques
Dual-energy CT improves the image quality with less radiation dose and motion artifacts [58]. Ultra-high-resolution computer tomography shows a crazy-paving pattern and decreased lung volume [59]. Quantitative CT delineates the pulmonary distribution (GGO and consolidations) to assess the disease extension [60-62]. At positron emission tomography (PET) CT, lung lesions show high 18F-FDG uptake with lymph node involvement. Conversely, the disseminated disease is absent, a finding suggesting that COVID-19 has pulmonary tropism. Although 18F-FDG PET CT cannot be routinely used in an emergency setting, it can be applied in the differentiation of complex patients [63]. Artificial intelligence enables early detection of changes in the lung at CT and helps to reduce the turnaround time; this is essential for the mass population screening at the outbreak in China and all over the world because it decreases the workload of radiologists and clinicians and promotes rapid triaging [64,65]. Futures studies are needed with the application of routine and advanced MR imaging [66-74] for diagnosis and differentiation from other infective or granulomatous pulmonary lesions in the future.
Conclusions
We conclude that chest CT can detect pulmonary and extra-pulmonary findings of COVID-19. The typical CT features of COVID-19 infection are bilateral peripheral multifocal GGOs and/or lung consolidations, while the presence of extra-pulmonary findings denotes advanced disease. Different structured reporting systems have been developed to facilitate communication between the clinicians and radiologists. Lastly, CT plays a role in the initial diagnosis of disease progression and guidance of therapy, surveillance of patients with response to therapy, prediction of overlying bacterial infection, and differentiation from simulating lesions.