Introduction
Abscesses contain localized infected fluid and elicit fever and pain. Some abscesses can be treated with antibio-tics alone, but others result in life-threatening sepsis [1]. When patients report strong pain, when monotherapy with antibiotics fails, and when there is a high risk of sepsis, abscesses should be drained. Image-guided percuta-neous drainage rather than surgical drainage has been used to address intra-abdominal or pelvic abscesses because it is safe and minimally invasive [2,3].
When intra-abdominal or pelvic abscesses are not visualized on ultrasound (US) images, computed tomography (CT)-guided drainage is useful. Abscesses deep in the body can be punctured under CT guidance; the puncture route should be on the same axial slice. However, as the ability to adjust the puncture route by changing the patient’s position and tilting the CT gantry is limited, a technique for puncturing in the cranio-caudal direction under CT fluoroscopy is needed.
We report a patient with rectal cancer, who underwent successful transperineal CT-guided drainage of an ischiorectal abscess. Chasing the needle tip by moving the CT gantry facilitated puncturing in the cranio-caudal direction.
Case report
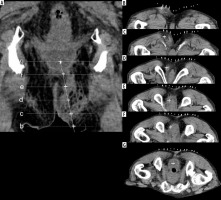
An 82-year-old man with no family history of cancer presented with a 1-week history of defecation pain. His medical history included the endoscopic submucosal dissection of rectal cancer 2 years earlier. His regular medication was apixaban for atrial fibrillation. We observed red and swollen skin induration near the anus. His white blood cell count was 11.6 × 103/μl, and C-reactive protein was 7.7 mg/dl. Contrast-enhanced CT scans showed rectal cancer recurrence with subepithelial invasion; there was an abscess on the ischiorectal fossa close to the tumour (Figure 1A). Endoscopic biopsy yielded a pathological diagnosis of rectal cancer recurrence.
Figure 1
A) A puncture line was drawn on the coronal image of the planning computed tomography. B-G) The marker (+) on the puncture line was shown on each axial image. During puncture the axial images served as the reference images
We planned to perform curative abdominoperineal resection (APR). To improve his preoperative condition, his abscess was treated for 1 week with antibiotics. Because his improvement was poor, we decided to perform CT-guided drainage to control the abscess. We initially considered a transgluteal approach, which is one of the most common approaches to drain pelvic abscesses. However, we suspected that this abscess had been containing cancer cells because it arose from his rectal cancer, and we thought that the drainage tract via a transgluteal approach remaining after APR would increase the risk of their dissemination. Therefore, we chose drainage via the transperineal approach by mutual agreement between interventional radiologists and gastrointestinal surgeons. A drainage tract in the APR range was thought to have a lower risk of dissemination. We intended to remove the drainage tube with the tract during the APR procedure.
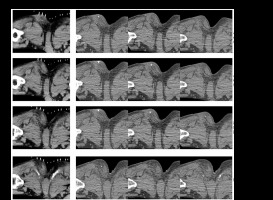
For CT-guided drainage via transperineal approach, the patient was in the jackknife position. The drainage using trocar technique was performed under local anaesthesia. As shown in Figure 1A-G, we drew a line from the puncture to the target point on coronal images of planning CT scans. Then, we placed a mark on the line on each axial image at 4-mm intervals. The marked axial images were on display during the procedure. The needle was advanced 4 mm at a time under CT fluoroscopy. The CT gantry position was moved toward the patient’s head to chase the needle tip throughout the puncture procedure. Figure 2 shows the details. We placed the needle tip on the skin puncture point and made it visible on the caudal slice of 3 simultaneous CT fluoroscopy slice images. We advanced the needle 4 mm at a time to the cranial side while referring to the marks on the axial images of planning CT scans. When the needle tip was shown on the cranial slice, we moved the CT gantry 8 mm to the cranial side to identify the needle tip on the caudal slice. This manoeuvre was repeated until we reached the target point. We then placed a pigtail 7Fr Dawson-Mueller drainage catheter (Cook Japan Inc., Tokyo, Japan) in the abscess on the ischiorectal fossa (Figure 3) and drained it. This improved the patient’s general condition; the catheter and the tract were removed during APR. There were no complications, and his postoperative course was good.
Figure 2
Three simultaneous computed tomography (CT) fluoroscopy images acquired during puncture are shown. Step 1: The needle tip was placed at the most caudal side of the 3 images. Step 2: With reference to the marker on the same axial level of the planning CT, the needle was advanced 4 mm at a time until the needle tip was seen on the middle image. Step 3: Then the needle was advanced another 4 mm until its tip was seen on the cranial image. Step 4: Thereafter the CT gantry was moved 8 mm to the cranial side to see the needle tip on the caudal image, and the steps were repeated until the target was reached
Discussion
We describe our unique CT-guided drainage technique, which can be applied when the puncture and the target sites are observed on different CT image slices. Our method overcomes the limitation of CT-guided drainage, which is difficult to puncture in the cranio-caudal direction.
Percutaneous drainage is a standard treatment for pelvic abscesses that do not require immediate surgery. CT-guided drainage has been widely used to address deep pelvic abscesses that are not visualized on US images.
Under CT guidance, deep pelvic abscesses can be drained via the transgluteal or the trans iliopsoas approach [4-8]. Both approaches are suitable for CT-guided drainage because the puncture and target points can be set in the same slice of axial CT images. The transperineal approach, including the transrectal and the transvaginal approach, is usually performed under US or endoscopic US guidance [9-13]. The transperineal approach is usually not employed under CT fluoroscopy guidance because the needle has to be advanced in the cranio-caudal direction. Our method permits safe and precise puncture in the cranio-caudal direction under CT fluoroscopy.
The puncture route must be carefully planned. The planning CT must be reconstructed because the puncture and the target sites are on the same slice. Therefore, we chose the puncture route on the reconstructed coronal image and put a mark on each axial image to refer to it during the procedure. Moving the CT gantry facilitates continuous monitoring of the needle tip on the CT fluoroscopy image. The operator must always see the position of the needle tip; the needle direction can be adjusted like a 3D joystick. The needle is advanced with reference to the marking on axial images of the planning CT until it appears on the next slice image simultaneously obtained by CT fluoroscopy. The CT gantry must be moved to chase the needle tip so that it never disappears on the 3 CT fluoroscopy slices. We think that our technique may also be useful for the CT-guided drainage of other lesions.
The transgluteal approach is favoured for addressing deep pelvic abscesses. In our rectal cancer patient, we feared cancer cell dissemination because his abscess was due to cancer perforation and may have contained cancer cells [14]. Consequently, because the residual drainage tract was expected to raise the risk of dissemination, we applied the trans-perineal approach and placed the tract in the area of the APR. Although CT fluoroscopy with real-time multiplanar reconstruction is useful for oblique punctures, it is not available at many institutions.



