Introduction
Diastasis of abdominal wall recti muscles, i.e. the increase in width of the linea alba with a separation between the paired recti muscles above the normal distance, represents a very common occurrence, at least in the minor degrees of widening [1,2]. Though diastasis can be found in both sexes and at various ages of life, it typically represents a post-partum event [3]. Widening of the weakened linea alba can be as large as 20 cm, with an inter-rectal distance greater than 5 cm being classified as severe [4]. Recti muscle diastasis is basically regarded as an aesthetic issue, with the subject presenting a bulging and flabby abdomen and looking as if they were “still pregnant”. However, a number of intra-pregnancy post-partum impairments have been somehow linked to this abnormality, including back pain, abdominal pain, and incontinence [5-7]. Risk factors for developing post-partum diastasis are believed to include patient age above 35 years, foetal macrosomia, twin pregnancy, and history of previous pregnancies [2,6,7]. Caesarean section seems not to be a risk factor, compared to spontaneous delivery, although according to some studies the risk of developing diastasis is higher after a Caesarean section [2]. Conversely, the antepartum activity level may have a protective effect on recti muscle diastasis, and exercise may improve post-partum symptoms of diastasis [1].
Recti muscle diastasis is usually identified clinically, or even by patient auto-evaluation. However, clinical assessment can be difficult when the subcutaneous layer is particularly thick [8,9]. Additionally, an accurate and objective measurement of the separation is mandatory to plan the appropriate management. Ultrasound (US) is commonly employed in the assessment of the anterior abdominal wall abnormalities [10-13]. Being a non-invasive and repeatable imaging modality [14,15]. US is regarded as the imaging modality of choice in the initial assessment of recti muscle diastasis, although plastic surgeons usually require also a computed tomography (CT) or a magnetic resonance imaging (MRI) study in patients scheduled for surgical repair with abdominoplasty.
The purpose of this single-centre, prospective study was to categorise the different anatomical variations of the rectus abdominis muscles diastasis by using US. To our knowledge, no published series has evaluated this issue of rectus muscle diastasis.
Material and methods
Study population
The study was approved by our Institutional Review Board. All enrolled patients gave their informed consent. Between May 2018 and April 2019 there were 92 consecutive women referred to our US laboratories because of a suspicion of diastasis recti. Patients had been referred for US by their plastic surgeon, family doctor, or gynaecologist. Many patients were self-referred. None of the women was pregnant at the moment of the examination, and none had abnormalities of the abdominal wall (deforming surgical scars, extensive fibrosis, etc.) that could interfere significantly with the US measurement. Sometimes a belly that is too flabby may be an obstacle to correct measurement, but no cases in our study had be excluded for this reason. The following data were recorded: patient age, parity, number of previous pregnancies, modality of delivery (spontaneous versus Caesarean section), and time since last delivery. There were also some males evaluated in the same period, but these were excluded to improve uniformity of the study populations.
Examination protocol
Studies were performed by two operators, with 33 and 13 years of experience with US, respectively. Operators had a specific training in evaluating diastasis recti. Voluson E8 (GE Healthcare) and RS85 (Samsung Healthcare) scanners were employed. US scans were performed with high-frequency, broad-band linear transducers. Transducer frequency could be adapted according to the thickness of the subcutaneous layer, but it was typically 10 MHz. Harmonic imaging was employed whenever necessary, particularly when the border of the rectus muscle did not appear to be sufficiently sharp. Patients were placed in the supine decubitus, with the head slightly extended above a pillow, the upper limbs aligned to the trunk, and the knees slightly flexed.
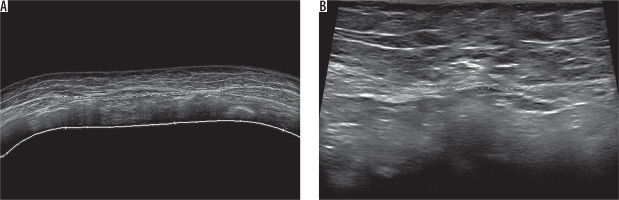
Measurements were obtained at rest, in a neutral moment immediately after an expiration. We accurately avoided pressing excessively on the abdominal surface with this transducer, to avoid pressure-related contraction reflexes. The typical level of the transverse scan of the abdominal wall was 3 cm above the navel and 2 cm below the navel, but the entire of the midline was checked to identify the exact pattern of diastasis. The inter-rectal width, i.e. the margin-to-margin distance between the medial border of the two rectus muscles, was recorded. At each of the two levels, the measurement was repeated three times by a single operator and then the mean value was collected. In the case of a diastasis exceeding 4 cm we employed trapezoid field-of-view scans to measure, while in the case of diastasis above 5 cm we employed real-time, extended field-of-view reconstructions. Measures obtained through an extended field-of-view image have proven to be fully comparable to those obtained on a conventional US image (Figure 1) [16]. In our practice we also routinely check the abdominal wall midline, both at rest and during the Valsalva manoeuvre, to rule out any concomitant hernia. However, this aspect is beyond the focus of this study.
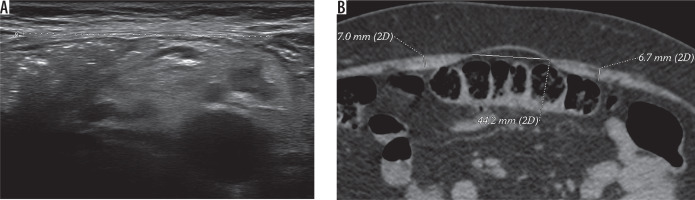
Figure 1
Thirty-two-year-old woman with two previous pregnancies. Diastasis (callipers) is present both above the navel (69 mm, extended field-of-view image in A) and below the navel (30 mm, conventional field-of-view image in B)
We also reviewed the data regarding diastasis severity from the non-contrast enhanced CT studies (64-detector row scanner) studies and non-contrast enhanced MRI (1.5T scanner) studies in patients who also underwent cross-sectional imaging.
Data analysis
All measures were taken three times, and the mean value was recorded. Diastasis was defined as a margin-to-margin distance of more than 20 mm. Diastasis was classified according to the following five anatomical patterns: open only above the navel, open only below the navel, open at the navel level, open completely but wider above the navel, open completely but wider below the navel.
Results
Diastasis was found in 82 patients, representing the 89.1% of the study population. The 82 patients with diastasis had an age range between 30 and 51 years, with a mean age of 35 years. There were five nulliparous women and 77 women with history of previous pregnancies. These ranged from one to four pregnancies, mean 1.9. Among 149 deliveries, there were 91 spontaneous deliveries and 58 Caesarean sections. Time from last delivery was 8-62 months, mean 14 months. Last delivery was spontaneous in 48 out of 77 women history of pregnancies and through Caesarean section in 29 (Table 1).
Table 1
Demographic data in our study population
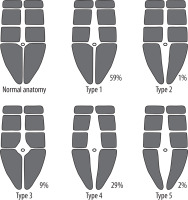
The separation width ranged between 21 and 97 mm, with a mean value of 39 mm. The following prevalence and severity of the various anatomical patterns was found. Open only above the navel in 48 cases (58.5%; 21-88 mm, mean 40 mm). Open only below the navel in one case (1.2%; 33 mm). Open at the navel level in seven cases (8.5%; 23-39 mm, mean 34 mm). Open completely but wider above the navel in 24 cases (29.3%; 21-97 mm, mean 41 mm). Open completely but wider below the navel in two cases (2.4%; 21-29 mm, mean 25 mm) (Table 2, Figure 2). In many of the cases with diastasis present only or more largely above the navel level, the distance between the two recti muscles measured below the navel was not only below the 20 mm threshold but was also close to zero, without any visible gap between the muscles.
Table 2
Prevalence and severity of the five diastasis patterns. Correlation with the modality of delivery
Figure 2
Schematic drawing of the prevalence of recti muscle diastasis according to the five anatomical patterns categorised in this study
There was no significant correlation between last delivery type and the pattern of diastasis. Comparing the only two groups with sufficient numerosity, we found similar percentages between patients with a history of spontaneous delivery and patients with previous Caesarean section. In 48 patients with a diastasis only above the navel, 8% had no history of delivery, 56% had a previous spontaneous delivery, and 35% had a previous Caesarean section. In 24 patients with a diastasis complete but wider above the navel, 4% were nulliparous, 58% had history of spontaneous delivery, and 37.5% had history of Caesarean section.
Eleven out of the 82 patients (13.4%) were undergoing CT imaging. In no case did CT categorise a different diastasis pattern in comparison with US. The difference in diastasis measurements between US and CT was 0-9 mm (mean, 4 mm). Also, seven out of the 82 patients (8.5%) underwent MRI. MRI did not categorise a different pattern compared to US in any case. The difference in diastasis measurements between US and MRI was 0-8 mm (mean, 3 mm) (Figure 3).
Discussion
Diastasis recti is an aponeurotic laxity of the linea alba, with the muscles themselves that can be normal in thickness or, more frequently, atrophic (myoaponeurotic laxity) [16,17]. Below the navel the collagen fibres of the linea alba are arranged in a more transverse way, compared to their arrangement above the navel [18]. This basically accounts for the findings in our series. The novelty of the current study is that we provided an in vivo confirmation of this knowledge, providing statistical data on the prevalence of the different anatomical patterns. During pregnancy, the geometry of abdominal muscles changes, still maintaining their function [2]. After the delivery there is a physiological reduction of the recti muscles’ thickness and an increase in the normal distance between the two muscles. This change usually persists for some months but, normally, within one year from the delivery the distance between the two muscles returns to the normal, pre-pregnancy value. In primiparous women, the inter-rectal distance may be considered “normal” up to values wider than in nulliparous [19].
There is no consensus of opinion regarding the normal distance between the rectus muscles. Only a few studies have evaluated the abdominal muscles in normal women and defined rectus diastasis. Beer et al. studied 159 healthy nulliparous women aged between 20 and 45 years with body mass index below 30 [20]. According to the Beer classification, the surgical definition of an abnormal inter-rectal distance is a width larger than 22 mm when measured 3 cm above the navel and larger than 16 mm when measured 2 cm below the navel [20]. In one study, the normal inter-rectal distance in primiparous women investigated 12 weeks after partum was found to be 26 mm when measured 2 cm above the navel and 11 mm when measured 2 cm below the navel [21]. In another article the normal inter-rectal distance 2 cm above the navel was established to be 15 mm in post-partum women and 10 mm in nulliparous women [22]. However, a recent study showed that the normal width of the linea alba changes during pregnancy and in the post-partum period, depending also on the level of the US scan [19]. During pregnancy, the normal range of values, i.e. the 20th and the 80th percentile, correspond to 49-79 mm below the umbilicus, 54-86 mm at 2 cm above the umbilicus, and 4-79 mm at 5 cm above the umbilicus. At six months postpartum, the 20th and the 80th percentiles corresponded to 9-21 mm at 2 cm below the umbilicus, from 17 to 28 mm at 2 cm above the umbilicus, and from 12 to 24 mm at 5 cm above the umbilicus [19]. It is also our experience that the distance is almost never uniform all along the linea alba. Our study supplies statistical information on the various anatomical patterns encountered in clinical practice, showing that some of them are more common than others.
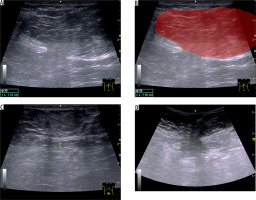
Patients with diastasis recti must also be investigated for the concomitant presence of median line hernias. This is done both at rest and during the Valsalva manoeuvre (Figure 4). At the same time, a diastasis may clinically mimic a ventral hernia, particularly during the Valsalva test [10,23]. A diastasis should be excluded before an abdominal wall liposuction procedure, to avoid complications involving the abdominal content and particularly the bowel loops [24].
Figure 4
Forty-one-year-old woman with three previous pregnancies. A) Longitudinal ultrasound (US) image obtained using a linear probe demonstrates a large, fat-containing, non-reducible epigastric hernia arising from a tear that is located near on the linea alba. Note also that the neck (11.5-mm, defect in the linea alba), is narrow in comparison to the hernial fundus. B) Schematic interpretation of the same image, in which the hernial sac is shown in red (in transparency). C) Transverse US image below the navel shows the linea alba in that location, thinned; no tears are demonstrable on US. D) Corresponding image of the epigastric hernia obtained using a using a convex, which allows a greater panoramic view
According to a recent meta-analysis, the available information supports US as an adequate method to assess diastasis of the recti abdominis muscles [25]. US measurement of inter-rectal distance has proven to have good to excellent intraobserver (both test-retest and between sessions) and interobserver reproducibility, particularly in the above-navel level of the abdominal wall [26-28]. In comparison with intra-operative findings also, US measurement has proven reliable, particularly in the above-navel area, while at the below-navel level there is a slight tendency to underestimate the separation between the two muscles [24,29]. The same applies to MRI [30] measurements and to CT [31] measurements, both of which underestimate somehow the extent of muscles separation [32,33]. The minor discrepancies found between pre-operatory measures, including imaging modalities other than US, and intra-operatory measures are possibly due to the muscle tone relaxation during general anaesthesia [32].
A pathological diastasis does not necessarily require repair, and conservative management may be an alternative [2,4]. As proven through US observations, the inter- rectus distance can be reduced by isometric contraction of the abdominal muscles, with the subject actively performing an abdominal crunch (crook lying position) [22]. Conversely, the drawing-in exercise, which mainly activates the transverse abdominal and internal oblique muscles, seems to be ineffective in improving diastasis [21]. Surgical repair is mostly done due to aesthetic reasons, and it is basically reserved for severe cases, larger than 5 cm, or when there is an associated hernia [1].
Our study has some limitations. First, the number of patients could have been larger. Second, we did not have a reference standard, and the presence and extent of diastasis in our US series had no independent verification. A minority of our patients also underwent CT or MRI, some others had abdominoplasty, but the vast majority of cases only had a US diagnosis. In this small group of patients there was no significant difference in terms of pattern categorisation and of diastasis severity measurement between US and CT/MRI. US has proven effective in various published series in measuring the width of diastasis recti, also with a good correlation with surgery [24,26,28].
Conclusions
The above-navel patterns of rectus abdominis muscle diastasis are by far the most common ones. Even when open completely, diastasis is usually wider above the navel. Knowledge of the anatomical type of rectus muscle diastasis could be interesting both to the patient (exercises to do and exercises to avoid) and to the surgeon (abdominoplasty approach planning, decision to insert or not insert a mesh, choice of the mesh type and size, etc.). In particular, establishing in each patient the anatomical pattern of diastasis may allow the development of tailored postnatal exercise programs.