Introduction
Breast lesions, benign and malignant, are a common concern in women’s health, requiring accurate and efficient diagnostic techniques. Although mammography and ultrasound have played an essential role in detecting and describing these lesions, there are still cases where lesions avoid detection, so clinicians are forced to adopt innovative solutions [1-3]. In response, magnetic resonance imaging (MR) has become a powerful tool, providing high sensitivity in visualising breast tissue and abnormalities [4-6]. Its high sensitivity allows visualisation of lesions that were not detected by other imaging modalities. The complexity of breast anatomy, the diversity of lesion types, and the critical nature of diagnosis accuracy are the reasons for performing MR-guided breast biopsy. Especially in patients with suspicious lesions not identified in retrospective ultrasonography and occult in mammography, histological verification with MRI-guided breast biopsy is recommended [7-10].
The primary goal of this publication was to compare the results of MR-guided breast biopsies performed at 2 distinct medical centres. In Centre 1, both patient qualification and biopsy procedures were performed by the same experienced team. In Centre 2, patients were examined who sought biopsy procedures and were referred from various medical facilities. The purpose of this article is also to describe the biopsy findings and subsequently to perform a comparative analysis of the results obtained from biopsies performed at the 2 different centres.
Material and methods
A total of 228 patients were enrolled in the study, with 120 patients undergoing biopsies at Centre 1 and 108 at Centre 2. The age of patients varied from 23 to 79 years. For menstruating patients, biopsies were performed between the 7th and 14th day of the menstrual cycle [11]. Institutional review board ethical approval was obtained for the conduct of the study. Informed consent was obtained from all patients participating in the study.
MR-guided breast biopsies were performed using dedicated equipment at both centres. At Centre 1, biopsies were performed on a Siemens Avanto 1.5T MR machine, equipped with a dedicated breast coil (Noras) for imaging and biopsy purposes. The vacuum-assisted biopsy procedure was facilitated using a Mammotome device. At Centre 2, biopsies were carried out using a Siemens Sola 1.5T MR system, equipped with a Sentinelle breast coil, and a BD EnCore vacuum-assisted biopsy device. Prior to the procedure, patients were asked about the use of medications such as aspirin, anticoagulants, or other agents known to impact bleeding time. Before the biopsy, the diagnostic MRI was reviewed for the best patient positioning and approach planning. Patients were examined in the prone position with the breast compressed by the grid plates to avoid body movements and enable tissue sampling.
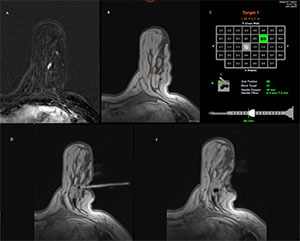
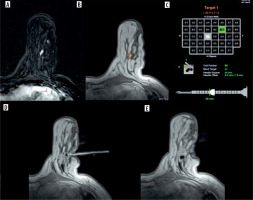
The imaging protocol was the same in both centres. The procedure was based on a T1-weighted 3D sequence without fat saturation and involved the use of subtraction images to enhance lesion visualisation. This standardised approach aimed to ensure consistent image quality and facilitate accurate targeting of the lesion during the biopsy procedure – the protocol is dedicated to visualise enhancing lesions after intravenous contrast injection (0.1 mmol/kg gadolinium-based agent) on subtraction images; position of the biopsy chamber inserted into the breast before tissue sampling and, after the procedure – to visualise the placed marker (Figure 1A-E).
Figure 1
Images of subsequent stages of MR-guided biopsy: A) T1 C+ subtraction image of enhancing, suspicious lesion, B) T1 C+ image without fat saturation, C) the localisation tools on the MR machine console, D) needle guide near the biopsy spot, E) marker placed at the biopsy spot
Breast composition types A, B, C, and D were assessed according to the American College of Radiology (ACR) BI-RADS lexicon [12].
All biopsy samples collected during MR-guided procedures were subjected to histopathological verification. Statistical analysis was performed to assess the relationship between various factors, including biopsy centre, lesion type, breast structure, and enhancement patterns. The distribution of lesion types and their dependence on the type of apparatus used for biopsies were evaluated using appropriate statistical tests. Furthermore, the potential impact of the radiologist’s experience on the characteristics of the lesion and the patient’s qualification for the procedure was explored.
Statistical analysis
The results of cancer lesions biopsied at 2 centres were compared. The following categorical variables of lesions were analysed, i.e. type of lesion, degree of BPE, type of breast structure, and continuous variables (age of patient and size of enhancement). Independence between relevant variables was analysed using the χ2 test of independence. However, differences between the median values of the enhancements and age in the individual groups analysed were examined based on the Mann-Whitney test for the median. A non-parametric test was used due to the lack of normal distribution of these variables. The significance level for all tests was set at p-value < 0.05.
Histopathological examination
Standard haematoxylin and eosin staining was performed, and the specimens obtained were evaluated by a pathologist with at least 5 years of experience in breast cancer diagnostics. Every single specimen was an object of evaluation. If breast cancer was determined, ER, PR, and HER status, as well as Ki67 index, were additionally identified to plan the patient management effectively.
Results
The results of the study on MR-guided breast biopsy, involving 228 patients with complete data, are as follows. Among the patients, 120 underwent biopsies at Centre 1, while 108 underwent biopsies at Centre 2. The average age of the patients in the analysed group was 49 years (median), with a minimum age of 27 and a maximum age of 81 years. A comparison of mean ages based on the presence of malignancy indicated that patients with diagnosed malignancies were older than those with benign changes (p = 0.00768). However, the distribution of lesions was independent of the degree of background parenchymal enhancement (BPE) and the type of lesion (p = 0.819). This independence was also maintained when analysing patient groups separately for Centre 1 (p = 0.489) and Centre 2 (p = 0.946).
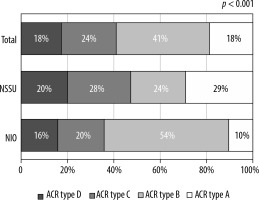
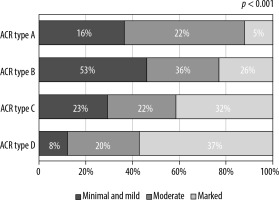
The distribution of lesions differed significantly according to the composition of the breast tissue in patients biopsied in the 2 centres (p < 0.001). Centre 2 predominantly had an ACR of type B breast composition (54%), while Centre 1 had a composition of type A composition (29%). The composition of the breast tissue was also dependent of BPE (p < 0.001), with a marked enhancement being predominant in types C and D breasts and minimal enhancement in the types A and B breasts. The results are shown in Figures 2 and 3.
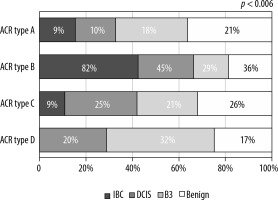
No significant relationship was observed between breast tissue composition and the type of lesion (malignant/benign) (p = 0.161). However, the composition of the breast tissue was correlated with histopathological results (p = 0.006), with the infiltrating carcinomas being dominant in ACR type C breasts (82%). This relationship is shown in Figure 4.
The sizes of the enhancements differed significantly according to the centre at which the biopsies were performed (median 17 for Centre 1 and 10 for Centre 2; p = 0.001, Mann-Whitney test).
The sizes of benign lesions (p = 0.002) and DCIS (p = 0.027) also showed significant differences between the 2 centres. The upper outer quadrant was the predominant location for malignant lesions in both centres.
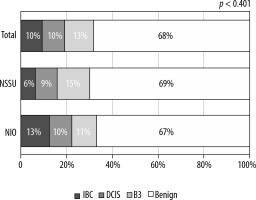
The distribution of the types of lesions (malignant/benign) was found to be independent of the biopsy device type used (p = 0.759). Furthermore, no correlation was observed between the type of histopathological change and the type of biopsy device (p = 0.401). In particular, in the case of Centre 1, a higher incidence of infiltrating carcinomas was diagnosed compared to lesions biopsied at Centre 2 (p = 0.12). Figure 5 shows this corelation.
Discussion
Comparative analysis of MR-guided breast biopsies performed in 2 distinct medical centres provides valuable information on the multifaceted dynamics that influences the diagnostic outcomes of this advanced procedure. In Centre 1, where biopsies were not only qualified but also performed by the same experienced radiologists, a higher rate of malignancy was observed in conjunction with larger lesion sizes. However, Centre 2 saw the same radiologists performing biopsies, but the patients were referred from external institutions. This divergence in patient demographics and referral sources underscores the intricate interplay between radiologist experience, patient selection, and lesion characteristics in the context of MR-guided breast biopsy.
Interestingly, the analysis revealed that the distribution of lesion types, whether malignant or benign, did not correlate with the specific vacuum biopsy devices used (p = 0.759). This implies that the choice of equipment does not inherently influence the detection and sampling of malignancies. This finding emphasises the consistent reliability of MR-guided biopsy devices in different clinical settings, thereby providing a standardised foundation for accurate lesion characterisation.
Furthermore, the discrepancy in the prevalence of carcinomas infiltrating between the 2 centres (p = 0.12) suggests a possible link between radiologist experience and the identification of the lesion. Centre 1, in which the radiologists both qualified and performed the biopsies, showed a higher incidence of infiltrating the body. This observation underscores the critical role of radiologist experience not only in procedural execution but also in patient qualification for MR-guided breast biopsy, where intricate judgment is critical for optimal outcomes.
Beyond the type of lesion, the distribution of lesion characteristics according to breast structure and biopsy centre was found to be statistically significant (p < 0.001). Variation in the dominance of fatty and heterogeneous breast structure (ACR type A and B) between the 2 centres (29% in Centre 1 vs. 54% in Centre 2) emphasises the importance of patient demographics and the composition of the breast to influence the distribution of lesions. This finding substantiates the need for customised patient selection and procedural approaches, acknowledging the distinct nature of breast anatomy among different populations.
Furthermore, observed variations in enhancement magnitudes depending on the biopsy site (p = 0.001) indicate the dynamic nature of the perfusion and uptake patterns. This underscores the complexity of interpreting imaging data and highlights the need for continued research into the intricate relationship between lesion characteristics and imaging findings.
The study has some limitations. The group of patients analysed is small, but MRI-guided biopsy is a high-end procedure used only in very specific cases, and it is expensive; therefore, the number of patients undergoing the procedure is limited. MRI-guided tissue sampling is limited by the position of the abnormality in the breast. Breast lesions located in the extreme posterior region of the breast or small abnormalities can be difficult or impossible to accurately target using MR. Another limitation is the non-uniform needle size that was used for the procedures. The needle gauge varies from 7G to 10G. That is why some malignancies could have been missed by not enough tissue material obtained, therefore using the 10G needle. However, due to the nature of the MR-guided biopsy, in some patients it was only possible to perform the biopsy with the 10G needle because the breast was too thin to use a larger needle and there was a risk of injuring the skin.
Conclusions
This comparative study elucidates the multifaceted factors influencing the outcomes of MR-guided breast biopsies in different centres. Radiologist experience, patient demographics, lesion characteristics, and breast structure collectively shape the diagnostic landscape. The results underscore the importance of expert radiologist involvement, informed patient selection, and a nuanced understanding of breast anatomy in optimising the potential of MR-guided breast biopsy as a diagnostic tool. This study encourages a more personalised approach to patient care, thereby ensuring accurate diagnoses and improved treatment strategies.