Introduction
The accurate detection and characterization of liver metastases in patients with known colorectal cancer are critical components in the management and treatment planning of these patients [1]. Liver metastasis is a common occurrence in colorectal cancer, and its early detection significantly influences treatment decisions and prognostic outcomes [2]. Dynamic contrast-enhanced magnetic resonance imaging (MRI) is an important imaging modality that provides high-resolution images facilitating the differentiation between benign and malignant liver lesions [3]. Certain sequences have been developed to reduce motion artifacts, enhancing image clarity in challenging abdominal areas [4]. However, MRI protocols can be time-consuming due to the use of contrast agents. This can pose challenges concerning the patient’s clinical condition and comorbidities. Additionally, it represents a major factor in terms of resource utilization and cost for the healthcare system. Therefore, there is ongoing research into abbreviated MRI (AMRI) protocols that aim to reduce imaging time without compromising diagnostic accuracy [5].
The literature contains numerous studies investigating gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA), known as a hepatocyte-specific contrast agent, in the detection of liver lesions. These studies have demonstrated high diagnostic accuracy in identifying liver lesions [6,7]. However, despite its advantages, Gd-EOB-DTPA is not the most commonly used contrast agent in routine clinical practice. Instead, extracellular contrast agents have broader application [8].
Therefore, we aimed to conduct our study using examinations with extracellular contrast agents. The objective of our study is to evaluate the diagnostic accuracy of 2 different abbreviated MRI protocols. The protocol we refer to as AMRI-1 includes T2-weighted imaging (T2W) combined with dynamic imaging. The other protocol, referred to as AMRI-2, includes T2W combined with diffusion-weighted imaging (DWI). These protocols have been compared with the standard comprehensive MRI protocol in terms of their effectiveness in detecting and characterizing liver metastases in patients with colorectal cancer.
Material and methods
Patient selection
This retrospective study analysed 100 patients (63 males, 37 females; mean age 62.6 years, SD 11.1 years) with known colorectal cancer who underwent MRI for liver metastasis detection. All detected lesions were confirmed to be metastases originating from colorectal cancer. Inclusion criteria were a confirmed diagnosis of colorectal cancer and the availability of histopathology, positron emission tomography–computed tomography (PET-CT), and follow-up imaging for lesion characterization. Exclusion criteria included incomplete imaging data and lack of histopathological confirmation. The study protocol was approved by the local Ethics Committee, and informed consent was obtained from all patients.
MRI protocols
All MRI examinations were performed on a 1.5-Tesla system (Optima MR450w, GE Healthcare, Milwaukee, WI, USA).
Three MRI protocols were evaluated:
AMRI-1: dynamic enhanced + T2W;
AMRI-2: DWI + T2W;
standard MRI: comprehensive protocol including T1W, T2W, dynamic contrast-enhanced, and DWI sequences.
Parameters of standard MRI sequences were performed with coronal T2W single-shot fast spin-echo (SSFSE) (TR/TE 685/82 ms; field of view [FOV] 420; slice thickness 5 mm), axial T2W SSFSE and fat-saturated T2W images (TR/TE 685/91 ms; FOV 440; flip angle 90°; slice thickness 4 mm; NEX 2), spoiled dual gradient-echo T1W in-phase and opposed-phase MRI (TR/TE 165/2.204 ms; slice thickness 4 mm), axial pre-contrast and dynamic post-contrast T1W 3-D LAVA FS (TR/TE 6.584/3.26 ms; FOV 440; flip angle 15°; slice thickness 4 mm) sequences, DW singleshot echo-planar imaging (TR/TE 6749/81 ms; NEX 2; FOV 380; image matrix size 148 × 190; slice thickness 5 mm) with b-values of 0, 500, and 800 s/mm2.
Image analysis
Two radiologists with 12 and 22 years of experience independently reviewed the MRI scans. The radiologists were aware that the patients had colorectal cancer but were blinded to the presence and nature of liver lesions. Lesions were categorised as benign, malignant, or indeterminate based on histopathology, positron emission tomography –computed tomography (PET-CT), and follow-up imaging. Sensitivity, specificity, and the area under the receiver operating characteristic curve (AUC) were calculated for each MRI protocol. Discrepancies between readers were resolved by consensus.
Statistical analysis
All statistical analyses were conducted using NCSS (Number Cruncher Statistical System) 2007 software (Kaysville, Utah, USA). Continuous variables were assessed for normality using the Shapiro-Wilk test. Data are presented as mean ± standard deviation (SD) for normally distributed variables and as median with interquartile range (IQR) for non-normally distributed variables. Categorical variables are presented as frequencies and percentages.
The inter-observer agreement between the 2 radiologists was assessed using Cohen’s κ statistic. The k-value was found to be 0.79, indicating substantial agreement between the observers.
Sensitivity, specificity, and the area under the receiver operating characteristic curve (AUC) values were compared across MRI protocols using χ2 tests, with statistical significance set at a p-value of <0.05.
Ethics committee approval
This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethics Committee approval was obtained from our institution’s Ethics Committee, with approval number B.10.1.TKH.4.34.H.GP.0.01/322, dated 03.10.2024. Because this study was retrospective, informed consent was waived.
Results
Lesion detection
The standard MRI protocol identified 197 liver lesions (175 metastatic, 18 benign, 4 indeterminate). Among these, 142 lesions (72.1%) were larger than 10 mm, with the majority being metastatic (140/142). Of the 55 lesions ≤ 10 mm, most were metastatic (35/55). In Figure 1, the Standard MRI protocol is exemplified for metastasis characterization.
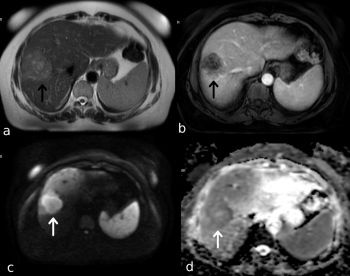
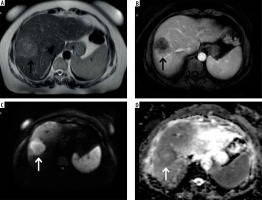
Figure 1
59-year-old male with metastatic colorectal cancer. A) Axial T2W sequence shows a hyperintense lesion in the liver right lobe anterior segment (black arrow). B) Axial T1W contrast-enhanced image shows hypointense lesion with peripheral contrast enhancement (black arrow). C) Axial DWI (b = 800). D) ADC map image shows diffusion restriction (white arrow), both readers characterised this lesion as malignant
Radiologist 1 identified 195 lesions using the AMRI-1 protocol (175 metastatic, 15 benign, 5 indeterminate), with 5 lesions representing partial volume artifacts (false positives). The sensitivity per lesion was 89.7% (95% CI: 0.85-0.93).
Radiologist 2 identified 183 lesions using the AMRI-2 protocol (169 metastatic, 6 benign, 8 indeterminate), with 8 lesions representing partial volume artifacts (false positives). The sensitivity per lesion was 92.3% (95% CI: 0.88-0.95).
Lesion detection rates are shown in Table 1.
Table 1
Lesion detection across different MRI protocols showing the total number of lesions detected, including the breakdown into metastatic, benign, indeterminate, and false positives
| MRI Protocol | Total lesions detected | Metastatic | Benign | Indeterminate | False positives |
|---|---|---|---|---|---|
| Standard MRI | 197 | 175 | 18 | 4 | 0 |
| AMRI-1 | 195 | 175 | 15 | 5 | 5 |
| AMRI-2 | 183 | 169 | 6 | 8 | 8 |
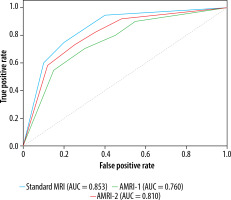
ROC curve analyses are shown in Figure 2.
Figure 2
ROC curve for different MRI protocols. This figure illustrates the ROC curves for the 3 MRI protocols evaluated in the study. The Standard MRI protocol demonstrated the highest diagnostic accuracy, followed by AMRI-2 and AMRI-1. The similarly high AUC values across the protocols suggest that both abbreviated MRI protocols (AMRI-1 and AMRI-2) could serve as effective alternatives to the standard protocol in clinical practice
In terms of lesion size distribution, all 3 MRI protocols demonstrated high effectiveness in detecting larger lesions (> 10 mm). Specifically, the Standard MRI protocol detected 142 lesions greater than 10 mm and 55 lesions that were 10 mm or smaller, while the AMRI-1 protocol identified 140 lesions greater than 10 mm and 55 lesions that were 10 mm or smaller. The AMRI-2 protocol detected 135 lesions larger than 10 mm and 48 lesions that were 10 mm or smaller. Although the detection rates for smaller lesions (≤ 10 mm) were similar between the Standard MRI and AMRI-1 protocols, the AMRI-2 protocol showed a slightly lower detection rate for these smaller lesions (as shown in Figure 3).
Figure 3
Lesion size distribution across MRI protocols. This figure compares the number of lesions greater than 10 mm and those 10 mm or smaller detected by each MRI protocol. While all protocols were effective in detecting larger lesions, the AMRI-2 protocol showed a slight decrease in the detection of smaller lesions (≤10 mm) compared to the Standard MRI and AMRI-1 protocols
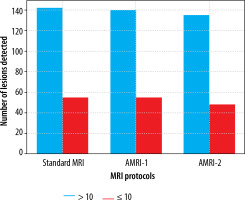
Lesion detection rates by lesion size are presented in Table 2.
Table 2
Lesion size distribution across MRI protocols, showing the number of lesions greater than 10 mm and less than or equal to 10 mm. No statistically significant differences were found between protocols
| MRI protocol | Lesions > 10 mm | Lesions ≤ 10 mm |
|---|---|---|
| Standard MRI | 142 | 55 |
| AMRI-1 | 140 | 55 |
| AMRI-2 | 135 | 48 |
| P value | > 0.05 | > 0.05 |
Diagnostic accuracy
After excluding indeterminate lesions, missed lesions, and false positives, the AUC for characterizing detected liver lesions was 91.0% (95% CI: 0.75-0.98) for Radiologist 1 (n = 190) and 93.5% (95% CI: 0.85-0.98) for Radiologist 2 (n = 183) using the AMRI protocols. The standard MRI protocol’s AUC was 96.8% (95% CI: 0.90-1.00) (as shown in Table 3 and Figure 4).
Table 3
Diagnostic accuracy of MRI protocols, comparing sensitivity, and the area under the ROC curve (AUC) for each protocol
| MRI Protocol | Sensitivity (%) | AUC (95% CI) |
|---|---|---|
| Standard MRI | 89.7 | 96.8 (0.90-1.00) |
| AMRI-1 | 89.7 | 91.0 (0.75-0.98) |
| AMRI-2 | 92.3 | 93.5 (0.85-0.98) |
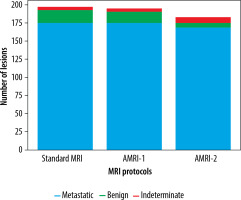
Figure 4
Proportion of lesion types detected by MRI protocols. This stacked bar chart provides an overview of the types of lesions detected by each MRI protocol. The Standard MRI protocol detected the highest number of metastatic lesions, while AMRI-1 and AMRI-2 also performed well in detecting metastatic lesions with slight variations in the detection of benign and indeterminate lesions. The chart underscores the effectiveness of all three protocols in identifying metastatic lesions, with minor differences in the detection of other lesion types
No statistically significant difference was found in sensitivity between the AMRI-1 and AMRI-2 protocols and the Standard MRI protocol (p > 0.05).
The acquisition times, advantages, and disadvantages of each MRI protocol are summarized in Table 4. This comparison highlights key differences in diagnostic accuracy, acquisition time, and suitability for patients with contrast agent restrictions.
Table 4
A comparative summary of acquisition times, advantages, and disadvantages of the MRI protocols
Discussion
Our study, along with other research in the literature, highlights the potential usefulness of AMRI protocols for the detection and characterization of liver metastases in colorectal cancer patients. Our results specifically demonstrate that the AMRI protocol, which includes DWI and can be performed without the use of contrast agents, has a comparable diagnostic accuracy to the standard MRI protocol.
DWI is a valuable imaging technique with unique advantages in various clinical settings. Beyond its use in liver metastasis detection, DWI has proven effective in identifying and characterizing lesions in multiple organs, particularly when contrast agents are contraindicated. This modality is especially beneficial in oncology for assessing tumour cellularity, monitoring treatment response, and differentiating between malignant and benign lesions in cases where rapid, non-invasive evaluation is required [9].
Canellas et al. [10] evaluated an abbreviated gadoxetic acid AMRI protocol for liver metastasis surveillance in colorectal cancer patients and, similarly to our findings, reported high sensitivity and specificity. Unlike our study, they used an AMRI protocol consisting of ultra-fast SE T2-weighted, DWI, and T1-weighted hepatobiliary phase (HBP) sequences. They reported sensitivity and AUC values above 90% for both readers, with no statistically significant difference compared to the standard MR protocol.
Granata et al. [11] compared gadoxetic acid-enhanced liver MRI with multidetector CT (MDCT) for the evaluation of colorectal liver metastases. In their study, they concluded that MRI has significantly higher diagnostic sensitivity and specificity than MDCT, particularly in patients undergoing chemotherapy and in detecting subcapsular and peribiliary metastases. Although our study did not directly compare MRI with MDCT, the high sensitivity and specificity of our AMRI protocols for detecting liver metastases are consistent with the findings of Granata et al. [11] and further reinforce the superiority of MRI, including abbreviated protocols, over CT in the evaluation of liver metastases.
Grabowska et al. [12] evaluated the diagnostic performance of various MRI sequences for detecting liver metastases in colorectal cancer patients and emphasized the importance of DWI and contrast-enhanced sequences in lesion detection and characterisation. Our study’s inclusion of DWI in AMRI protocols supports their findings by demonstrating the critical role of DWI in accurately identifying metastatic lesions, particularly those smaller than 10 mm.
Unlike other studies, we would like to emphasize that our study focused on the use of extracellular contrast agents, which are more commonly used in routine practice, instead of hepatocyte-specific contrast agents. Despite the advantages of gadoxetic acid in liver imaging, it is not routinely used, and we consider this distinction is important. This difference makes our study applicable to a wider range of clinical settings.
Granata et al. [13] reviewed AMRI protocols in various disease conditions, including hepatocellular carcinoma, prostate cancer, non-alcoholic fatty liver disease, and liver metastases. They concluded that these abbreviated protocols are effective in reducing examination time, cost, and patient discomfort without compromising diagnostic accuracy.
Hayoz et al. [14] compared the diagnostic accuracy of dynamic contrast-enhanced phases, the HBP, and DWI for the detection and characterization of liver metastases originating from neuroendocrine tumours (NETs). They found that the combination of DWI and HBP had the highest diagnostic accuracy for detecting and characterizing NET liver metastases. However, they also noted that AMRI protocols could be beneficial for specific patient groups.
The incorporation of AMRI protocols into routine clinical follow-up and screening programmes has several important advantages. Firstly, shorter examination times improve workflow efficiency, allowing more patients to be scanned in the same time frame. This can be of particular benefit in busy hospitals. Secondly, it is important in terms of reducing acquisition costs and supporting sustainability. Finally, shorter imaging sequences and, in some cases, the absence of contrast media may improve patient compliance and comfort [15].
In evaluating the 2 abbreviated MRI protocols in our study, the AMRI-1 protocol involved the administration of contrast agent, but to save time, only T2-weighted imaging was performed without additional sequences. This protocol demonstrated high diagnostic accuracy in detecting metastatic lesions when compared to the standard MRI protocol. The other protocol we investigated, AMRI-2, was performed without the use of contrast agent, making it a valuable alternative for patients who cannot receive contrast. Despite including only DWI and T2-weighted imaging sequences, the AMRI-2 protocol achieved a remarkably high diagnostic accuracy.
Another noteworthy point is that the AMRI-2 protocol demonstrated a slightly lower success rate in detecting lesions smaller than 10 mm compared to the other protocols. This finding suggests that small lesions require particular attention and more precise evaluation. In future studies, the use of thin-slice techniques and the optimization of imaging protocols in this direction could enhance the diagnostic accuracy for detecting small lesions. Such technical improvements could further increase the clinical effectiveness of the AMRI-2 protocol.
Our study has several limitations. Firstly, it is designed as a retrospective and single-centre study. Therefore, the results may only reflect a preliminary evaluation of the AMRI protocol. Larger, multicentre prospective studies are necessary. Secondly, histopathological confirmation was not available for most patients in the study. Although biopsy was included for lesion confirmation in certain cases, routine radiological diagnosis of liver metastases does not always require biopsy, as non-invasive methods like PET-CT or follow-up imaging are commonly used to confirm lesion characteristics in clinical practice. Additionally, our abbreviated MRI protocol was evaluated for a single region (the liver). However, we know that lymphadenopathy and peritoneal disease, which may accompany liver metastases, can also be reliably detected with DWI [16].
Conclusions
In our study, we specifically demonstrated that the AMRI-2 protocol (DWI + T2-weighted imaging) possesses comparable diagnostic accuracy to the standard MRI protocol in detecting and characterizing liver metastases. However, these AMRI protocols are not intended to entirely replace standard protocols. Considering the special conditions of some patients (such as allergies or comorbidities) or during specific follow-up intervals or after a certain period of monitoring, we believe that integrating AMRI protocols into the follow-up program could be appropriate.