Introduction
Haematological disorders such as thrombocytopaenia (TCP) are associated with a high risk of bleeding. The coexistence of TCP can also make the treatment of a number of other diseases much more difficult and complex, for example atrial fibrillation, cardiovascular complications, or continuation of tumour-related chemotherapy [1]. TCP that is resistant to treatment is a challenge for clinicians. Treatment options are limited, and they include a few medicament programs, but the results are often far from satisfactory. Even if, in patients with chronic TCP, the incidence of severe bleeding occurs relatively rarely, even with platelet (PLT) counts < 10,000/µl, it is not easy to decide when the routine prophylactic transfusion should be maintained. Moreover, PLT transfusion performed too often can induce refractoriness to this line of therapy due to immunological factors [2]. Invasive therapy, like splenectomy, is an option reserved only for a small group of patients. Partial splenic endovascular embolization (PSEE) could be a valuable, alternative option for most of the patients with TCP who do not respond well to other types of therapy. In our study we selected a group of patients diagnosed with refractory TCP, to undergo endovascular procedure, and we followed them for detailed analysis. The purpose of this study was to evaluate the effectiveness of TCP treatment with PSEE in a follow-up as an observation of PLT level changes and to assess the safety and potential complications after the embolization procedure.
Material and methods
In 2017-2019, PSEE was performed in a group of 22 patients aged 27-75 (mean 46.5 ± 3.5 years) due to TCP. This group included 13 men (mean age 59.15 ± 12.32 years) and 9 women (mean age 54.0 ± 13.28 years). The demographic characteristics and comorbidities in the study group are presented in Table 1. In this group, 5 participants underwent a second PSEE due to the lack of effectiveness after the first procedure. A total of 27 partial splenic embolization treatments were performed. The hospitalization time of patients with TCP was 5-35 days (mean 9.4 ± 2.12 days).
Table 1
Demographic characteristic and comorbidities of the study group
[i] TCP – thrombocytopaenia, PBC – primary biliary cholangitis, AH – arterial hypertension, AITP – autoimmune thrombocytopaenia, ITP – idiopathic thrombocytopaenic purpura, DMT2 – diabetes mellitus type 2, CVI – chronic venous insufficiency, IHD – ischaemic heart disease, AF – atrial fibrillation, CHF – chronic heart failure, AAA – abdominal aortic aneurysm, SAS – sleep apnoea syndrome, PVT – portal vein thrombosis, RA – rheumatoid arthritis
The study was performed in accordance with the guidelines of the local University Ethics Committee for conducting research involving humans – decision no. KB499/2016. All subjects provided their written informed consent to participate in this study according to the Helsinki Declaration.
In order to assess the severity of the post-embolization syndrome (PES), other authors graded it from 0 to 4 based on Southwest Oncology Group Toxicity Coding, where PES was recognized from grade 2 and more [3]. We decided to use the proprietary, 5-point, semi-quantitative scale. The occurrence of symptoms was assessed, and score values were assigned to the summary:
pain symptoms – 1 point;
sever pain requiring the use of opioid analgesics – 1 point;
nausea, vomiting – 1 point;
low-grade fever or fever – 1 point;
inflammatory parameters increase (C-reactive protein [CRP], white blood cells [WBC]) – 1 point.
0-1 point: mild postembolization syndrome; 2-3 points: moderate postembolization syndrome; 4-5 points: severe postembolization syndrome.
Embolization procedure
The PSEE was performed using the Seldinger method from the inguinal approach under local anaesthesia. 1% lignocaine was used for anaesthesia. 5F access sheaths and 5F guide sheaths or catheters with an end inserted into the celiac trunk were used. The rest of the procedure involved the use of the coaxial catheter technique using microcatheters. Prolonged arteriography of the celiac trunk and its branches was performed until indirect splenoportography was obtained. For injection, 15-20 ml low osmolar non-ionic iodine contrasts were administered at a rate of 4-5 ml/s. After the examination, the patency of the vessels, the direction of blood flow, the size of the spleen, and its vascularization were assessed. In the case of qualification for PSEE, selective arteriography of the selected branch of the splenic artery was performed in order to confirm the extent of its vascularization before the final administration of the embolization material (Figures 1 and 2). The access point was normally closed with an AngioSeal (Terumo) closure.
Figure 1
Selective catheter angiography of the spleen, splenomegaly and extended branches in the hilum of spleen are visible
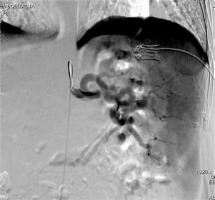
Figure 2
The same patient as Figure 3, N-butyl cyanoacrylate glue embolization of one splenic branch (black arrow) and the area of contrast deficit in part of the spleen (asterisk)
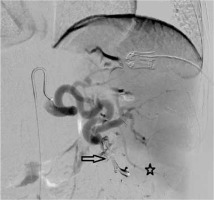
Patients with TCP resistant to treatment were qualified for angiography, and at the same time, 22 patients underwent PSEE; in 5 cases PSEE was repeated. Distal embolization was performed using the coaxial catheter technique with the use of a microcatheter (Progreate, Terumo Medical Corporation, USA; Lantern, Penumbra, USA). Embolizations were performed using selective arteriography of the branches in the splenic hilum, assessing the extent of their vascularization, and selecting the appropriate vessel for the procedure. The percentage of spleen parenchyma excluded from circulation was estimated within 30-70%.
For PSEE in patients with refractory TCP, in 5 patients it was performed in 2 stages. The mixture of Histoacryl (N-butyl cyanoacrylate glue [NBCA], Braun, Germany) and Lipiodol (Guerbert, France) - 10 cases, coils (Tornado, Cook Medical, USA; Ruby, Penumbra, USA) – 10 cases, and polyvinyl alcohol – (PVA, Cook Medical, USA) – 7 cases were used for the embolization procedure, often using various embolization materials together during one treatment (Figure 1).
Results
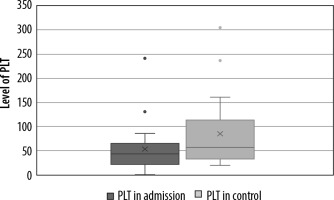
The results are presented in Table 2. Patients with treatment-resistant TCP often requiring blood transfusions were enrolled in the study. After the procedure in outpatient control, a gradual increase in PLT was observed in a mean period of 194 days. When no satisfactory increase in PLT count was observed after first procedure, patients were qualified for re-embolization. The procedure was performed twice in 5 patients. The mean value of PLT before procedure increased from 22.0 ± 15 to 87.7 ± 67.9 (p < 0.05) (Figure 3). All patients became independent of platelet transfusions.
Table 2
List of parameters assessed in the study group
Only in 2 cases was severe post-embolization syndrome observed (4-5 points). In both cases, approximately 70% of the circulation to the spleen was turned off. Closure less than 50% of the spleen circulation was associated with poorly expressed post-embolization symptoms (mild 0-1 point or moderate 2-3 points). The mean severity of the post-embolization syndrome in the whole group was 1.0 ± 1.2.
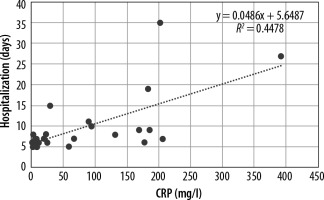
A strong positive correlation (r = 0.8, p < 0.05) was found between CRP and the severity of the post-embolization syndrome in patients after partial embolization of the spleen. Increased symptoms of post-embolization syndrome were also associated with a significant increase in hospitalization time: 27.0 vs. 7.2 days (r = 0.66, p < 0.05) (Figure 4).
The radiation absorbed by the patient during the procedure in 27 endovascular procedures with TCP and splenomegaly ranged from 0.103 to 1.658 Gy (mean 0.19 Gy). Preoperatively, patients with TCP and splenomegaly were routinely administered amoxicillin (or ciprofloxacin in the case of drug allergy). The antibiotic was administered intravenously in a dose of 2.0 × 1.2 g the day before endovascular procedure, and then treatment was continued for 7-10 days depending on the persistence of the elevated CRP. The percentage of spleen parenchyma excluded from circulation was estimated within 40-70% (mean 40-50%).
Complications
Serious complications occurred in 1 patient (3.5%) with TCP. He had a fluid reservoir in the spleen after 70% embolization of the spleen, requiring splenectomy.
The frequency of severe postembolization syndrome is low. In the group, after 27 embolization procedures, no features of postembolization syndrome were found in 11 patients, in 9 cases symptoms were mild, in 5 patients the symptoms were moderate, and only in 2 cases symptoms were severe (mean 1.04 on a 5-point scale).
Discussion
Partial endovascular embolization of the spleen (PSEE) is a procedure performed due to many different indications, including liver cirrhosis, gastric varices, and splenomegaly. There also exist surgical indications for the intervention, and they include the patients after liver transplant who suffer from splenic artery steal syndrome (SAS) as a complication of the prior therapy [4]. Coagulation disorders in the course of liver diseases are frequently observed abnormalities. They are not only related to impairment in the process of production of coagulation factors, but also affect the level of thrombopoietin, which exacerbates the decrease in platelet count. It is important because an additional benefit observed in the patients after the partial embolization of the spleen is the increase in platelet count, which minimizes the risk of bleeding, also in long-term follow-up [5]. However, the mechanisms that contribute to this rise are not fully understood.
Another indication to perform PSEE (or sometimes more invasive splenectomy) is hypersplenism-related TCP as an effect of sequestration of the platelets in splenic parenchyma.
The effectiveness of PSEE in our study group with refractory TCP has not been assessed so far. In the literature, research focuses mostly on the problem with hypersplenic TCP as a result of other diseases, e.g. neoplasia [6,7].
Based on available literature, the prevailing opinion is that proximal embolization (involving the trunk of the splenic artery) is an effective and safe procedure [8]. From our experience, the selective embolization comprising smaller branches of the splenic artery allows us to exclude only a part of the blood circulation in the organ, which decreases the risk of serious complications such as necrosis and its consequences. After the initial angiography, the branches chosen for embolization were those that supplied with blood to the middle and lower segments of the spleen, because the top of the organ can have extra vasculation from short gastro-omental branches.
This method of action allowed us to limit the area of splenic ischaemia, which resulted in less intense post-embolic syndrome during the post-operative period. A major complication was observed in only 1 case, and it concerned a patient who developed a splenic abscess after simultaneous exclusion of more than 70% of splenic circulation.
It was proven that PSEE performed in cancer patients treated with chemotherapy is a safe intervention, and in long-term follow-up it results in increased platelet counts, allowing continuation of chemotherapy [6]. The elevation of platelets was durable and correlated with the amount of splenic parenchyma that was cut off from the blood supply.
Post-embolization syndrome in the studied group of patients, if it occurred, was mild (average 1.0 on a 5-point scale). This observation can be explained by the fact that we have always tried to emphasize careful selection of the area and location of the embolization.
On the other hand, this strategy probably caused a lack of satisfactory response for the treatment in 5 of our patients and generated the need to repeat the PSEE procedure.
However, we should emphasize the fact that consecutive PSEE intervention did not involve increased risk of complications or exposure to excessive doses of radiation.
In our study the low dose of ionizing radiation in the range 0.103-1.658 Gy (0.19 Gy on average) is connected to the short time of embolization procedures and low level of periprocedural complications.
Therefore, in accordance with the regulations, after exceeding the dose of 1.0 Gy, additional diagnostic procedures should be implemented, and if the dose exceeds 3.0 Gy, specialist consultations should also be included. For this reason, strict compliance with the provisions on radiation protection of the patient is recommended, especially by less experienced operators.
The presented results were possible thanks to the use of new embolic devices and agents that limit the risk of potential migration and are less susceptible to recanalization.
Moreover, using microprofile devices and microca-theters allows deep peripheral intervention. However, the choice of materials used during the procedure depends on their availability and the operator’s experience.
The literature data indicate that complications after PSEE are rare, and they depend on the therapeutic method of exclusion of the circulation in the spleen (surgical or intravascular) with clear predominance of the intravascular method [9].
There are several limitations to our study, and they include mainly the number of patients, which was small, heterogenicity of the studied group, and different materials used for embolization procedures, which is why further research is needed.
Conclusions
Partial endovascular embolization of the spleen (PSEE) may be a valuable therapeutic option for patients with refractory TCP. The results show that it is a safe method with a low complication rate. Based on our experience, we suggest performing even 2 procedures of embolization of smaller amounts of splenic parenchyma over 1 procedure with occlusion of more than 70% of splenic circulation.
Despite the safety of PSEE, it is recommended that a prophylactic antibiotic therapy be introduced as a periprocedural procedure before operation. Moreover, procedures in the field of radiation protection should be strictly followed because the normative doses are exceeded during most embolization procedures.
The evaluation of PSEE effectiveness in patients with TCP requires further studies on a larger group of patients.