Introduction
Prostate cancer (PCa) is the most common cancer in the world and the second most common cause of cancer- related deaths [1]. If PCa is detected locally, the 5-year survival rate approaches 100%, but in the presence of metastatic disease, this rate decreases to 30% [2]. Therefore, the early detection of PCa in suspected patients is crucial. Conventional methods for this detection include a digital rectal examination (DRM) and prostate-specific antigen (PSA) measurement, and in patients found to be clinically suspicious, a blind biopsy is performed under transrectal ultrasonography (TRUS) guidance [3]. However, these methods have certain limitations. For example, in TRUS biopsies, false-negative results can be obtained, and cancer can be evaluated as low grade [4]. In addition, 25% of tumours cannot be diagnosed in the first TRUS-guided biopsy. Therefore, repeat biopsies are undertaken, but the rate of diagnosis of PCa in repeat biopsies is even lower than that of the first procedure [5]. In addition, it is reported that taking the analysis of prostatectomy material as a reference, the accuracy of the Gleason scores reported from a TRUS-guided biopsy is between 30 and 58% [6]. Therefore, the use of multiparametric magnetic resonance imaging (mpMRI) in PCa has become widespread. Use of mpMRI is recommended to prevent unnecessary biopsies, to perform targeted biopsy in detected lesions, and to detect cancer foci in areas that cannot be adequately examined by DRM [7,8].
With the widespread use of mpMRI, the rate of incidental findings (IFs) detected by this examination has also increased [9-12]. While some of the detected IFs are benign and not clinically significant, others may need to be followed up by imaging. Furthermore, for some IFs, a histopathological diagnosis is required, and some patients may need surgery. Therefore, it is particularly important to differentiate between clinically significant and non-significant IFs. In the current study, we aimed to determine the frequency of IFs detected in the mpMRI examination according to their organ distribution and clinical significance.
Material and methods
Before the study, ethics committee approval was obtained from the non-interventional Ethics Committee of Eskişehir Osmangazi University. The mpMRI examinations performed between January 2015 and January 2020 were retrospectively screened from the hospital image archive. All patients with suspicion of PCa based on clinical findings, who were followed up for this cancer with mpMRI, were included in the study. Pelvic MRI examinations performed due to other malignancies and without multiparametric features were not included in the study.
mpMRI was performed at least 6 weeks after the biopsy procedure in accordance with the PI-RADS recommendations [13]. All examinations were undertaken using a 48-channel body coil in a 3-Tesla (General Electric, Milwaukee, WI) MRI device. No enema or antispasmolytic was used before the MRI scan. The imaging protocol was as follows: axial turbo-spin echo (TSE) axial T1 imaging, TSE T2-weighted imaging in 3 planes (axial, coronal, and sagittal), diffusion-weighted imaging (EPI, b = 0, 500, and 2000), and dynamic contrast-enhanced pelvic MRI following a contrast agent injection (1 mmol/kg gadoteric acid, 3 ml/sec). The images were evaluated by a radiologist with 10 years’ experience in genitourinary MRI.
The images were retrospectively re-evaluated in terms of IFs, defined as incidentally detected asymptomatic findings that were not associated with PCa. Findings used in PCa staging, such as seminal vesicle invasion, rectal invasion, bladder invasion, bone metastasis, and pathological lymph nodes were not considered as IFs. The findings associated with PCa were also recorded. In patients who had undergone more than 1 mpMRI, the first examination was evaluated.
The IFs were divided into 2 categories as those related to the genitourinary system and those of the extragenitourinary system. In addition, the IFs that required urgent diagnosis and treatment were evaluated as clinically significant, while those for which follow-up alone was sufficient without the need for additional imaging or surgical procedures were included in the clinically non-significant group. The patient population was divided into age ranges 39-54 years, 55-64 years, 65-74 years, and over 75 years to compare the frequency and clinical significance.
Continuous variables were expressed as mean and standard deviation, and categorical variables as numbers or percentages. The mean values of IFs were compared between the age groups using the Mann-Whitney U test. SPSS was used for all statistical analyses, and p < 0.05 was considered statistically significant.
Results
There were 515 mpMRI scans that met the initial criteria. Eighty-nine of these scans belonged to repeat examinations, and thus they were excluded from the study. The mpMRI examinations of the remaining 426 patients were included in the study. A total of 321 IFs were detected in 212 (49.8%) of these patients, of whom 123 (28.8%) had 1 IF, 69 (16.2%) had 2 IFs, and 20 (4.7%) had 3 IFs. The mean age of the patients was 63.53 ± 7.89 (39-86) years. There were 58 patients (13.6%) aged 39 to 54 years, 171 patients (40.1%) aged 55-64, 165 patients (38.7%) aged 65-74, and 32 patients (7.5%) aged over 75. Table 1 summarizes the rates of IFs according to the age range of the patients. The rate of IFs per patient increased with age, but the rate of IFs per patient was 0.94 and 0.88 in the 64-75 and over 75 age groups, respectively (p = 0.001).
Table 1
Number of genitourinary and extragenitourinary IFs according to patient age ranges and their rates per patient
There were 132 genitourinary IFs (41.1% of all) (Figures 1 and 2A-B). The findings are summarized in Table 2. Among the genitourinary IFs, the most common were increased bladder wall thickness (n = 47, 35.6%), epididymis cysts (n = 16, 12.1%), and hydroceles (n = 16, 12.1%). The number of extragenitourinary IFs was 189 (58.9% of all IFs), with the most common being observed as inguinal hernia containing fat (n = 79, 41.7%). Other common findings were colon diverticula (n = 23, 12.1%), Tarlov cysts (n = 19, 10%), and enchondromas (n = 10, 5.2%). The results of extragenitourinary IFs are summarized in Table 3. The rates of IFs per patient for the 39-54, 55-64, 65-74, and over 75 age groups were determined as 0.10, 0.23, 0.45, and 0.38, respectively, for the genitourinary group and 0.31, 0.44, 0.49, and 0.50, respectively, for the extragenitourinary group. When the findings were evaluated according to the age ranges, a statistically significant increase was found in the IF rate in the 39-54, 55-64, and 65-74 age ranges (p < 0.05). However, there was no statistically significant increase for the 75-year-old group compared to the 65-74 age group (p = 0.853).
Figure 1
Axial T2-weighted image magnetic resonance imaging (T2WI MRI) shows a bladder stone in the bladder lumen
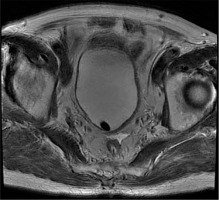
Figure 2
A) Axial T2-weighted image magnetic resonance imaging (T2WI MRI) and B) sagittal T2WI MRI shows herniated bladder with intraabdominal fat in the right inguinal canal
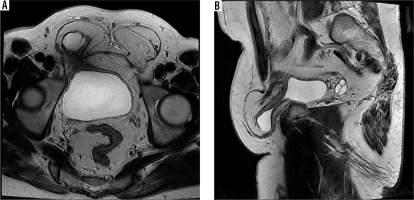
Table 2
Clinically significant and non-significant genitourinary incidental findings
Table 3
Clinically significant and non-significant extragenitourinary incidental findings
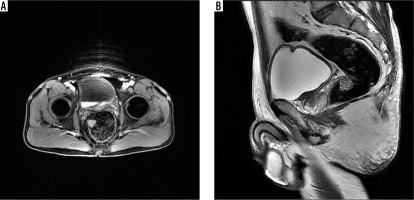
When the IFs were divided into 2 groups, as clinically significant and non-significant, 22 (6.9%) clinically significant IFs were detected. Of these findings, 4 were related to the genitourinary system and 18 were related to the extragenitourinary system. Clinically significant IFs were identified as bladder masses in 4 cases (ureteral carcinomas) (Figure 3A-B), inguinal hernia with bowel loops in 4, rectal polyps in 3 (tubulovillous adenoma in 1 and no pathology in 2) (Figure 4A-B), iliac artery aneurysms in 4, a colon polyp (no pathology), an anal canal mass (squamous carcinoma), a peritoneal mass (adenocancer), an intramuscular mass (Schwannoma’s), a mass in the left lumbar paravertebral muscle (no pathology), a left parailiac mass, and an appendiceal mass (in one patient each). The mean age of the patients with clinically significant IFs was 66.78 (56-80) years. There were 3 clinically significant IFs in the 75-year-old group, 12 in the 65-74 group, and 7 in the 54-65 group. Fifteen (68.2%) of the clinically significant IFs were detected among the patients over the age of 65 years. Statistically, the frequency of clinically significant IFs was higher in patients over 65 years of age (p = 0.001).
Figure 3
A) Axial T2-weighted image magnetic resonance imaging (T2WI MRI) and B) sagittal T2WI MRI shows a mass on the right posterolateral wall of the bladder
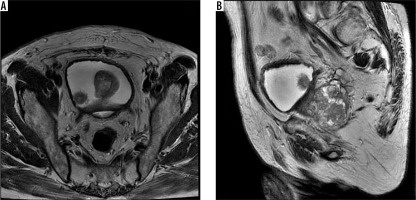
Figure 4
A) Axial contrast-enhanced T1-weighted image magnetic resonance imaging (T1WI MRI) shows a mass protruding into the rectum lumen on the right lateral wall of the rectum. B) In the same patient’s MRI, a mass lesion can be seen in the anterior wall of the rectum in the sagittal T2-weighted image (T2WI) image
Although not included in the study as IFs, extraprostatic findings (seminal vesicle, rectal bladder invasion, bone metastasis, and pathological lymph node) were detected in 132 patients. Forty-six patients had suspicious seminal vesicle invasion, 17 had bladder invasion, a further 17 had rectal invasion, 31 had bone metastasis, 20 had pathological lymph nodes, and 1 patient had penile metastasis.
Discussion
Currently, mpMRI is frequently used in the detection, follow-up, and post-treatment evaluation of PCa patients. With this increasing use, the rate of IF detection in mpMRI has increased, but due to the relatively new widespread adoption of this examination, there are not yet many studies in the literature on this subject. In our study, we found IFs in approximately half (49.8%) of the patients who underwent mpMRI. The frequency of IFs increased with age, with 183 (39.7%) of all IFs being detected in patients over 65 years. In the same patient group, 68.2% of the clinically significant IFs were observed.
In a study performed with CT colonoscopy for the detection of IFs, the rate of extracolonic IFs was reported as 85% [14], while other studies conducted with patients admitted to the emergency department with trauma detected IFs at a rate of 58-62% [15,16]. In another study, in which all abdominal CT scans of patients presenting to the emergency department were evaluated, the rate of IFs was reported to be 86% [17]. In mpMRI studies in the literature, Cutaia et al. [9] found 461 IFs in 341 (52.7%) of 647 patients, and Sherrer et al. [18] detected 349 IFs in 233 (40%) of 580 patients. In our study, we detected IFs in 212 patients (49.8%), which is largely consistent with the literature. We consider that the small differences between our study and previous research may be due to the mean patient age, which was 67.1 years (IF rate: 52.7%) in the study of Sherer et al. [18] and 63.3 years in the study of Cutaia et al. [9] (IF rate: 40%). The mean age of our sample was 65.5 years, and both the mean age and IF rate in our study were between the values reported by the previous 2 studies, which can also explain the slight differences.
In our study, there were 132 genitourinary IFs (41.1%). In other studies in the literature, the genitourinary IF rate was found to be 30.2% and 49% [9,18], indicating differences compared to our study. The reason for the higher rate of genitourinary IFs in the study of Sherrer et al. [18] may be that they used the T1-weighted imaging sequence including the whole abdomen, while our protocol was limited to the pelvis, in line with the PI-RADS recommendations. Therefore, the previous researchers also included frequently encountered renal cysts (23% of genitourinary IFs) in their evaluation [18]. On the other hand, the scan covering the whole abdomen did not result in a much increase in extragenitourinary IFs. In another study [9], the reason for the detection of a lower rate of extragenitourinary IFs (30.2%) compared to our study may be the inclusion of findings such as dolichocolon, muscle changes, and phleboliths, whereas we excluded them from our sample.
Clinically non-significant IFs obtained by imaging methods may cause unnecessary worry and health burden. However, although the rate is low, it is important to identify clinically significant IFs. In our study, we evaluated 22 (6.9%) of all IFs as clinically significant. In another study conducted with mpMRI, the findings were divided into 3 groups, and 94 (20.4%) IFs were identified to be potentially clinically significant and 12 Ifs (2.6%) as clinically significant [9]. When compared with this study, our rate of clinically significant IFs was markedly higher, but this may be due to the different classification systems used. Because the classification of IFs is not standardized, comparisons between studies may cause some errors. A standardized classification method for IFs would be useful to make a more accurate and efficient comparison between the results of studies in the literature. Similarly to our data, the clinically significant IF rate was found to be 6.6% in a previous study [18].
The rate of clinically significant IFs was determined as 6-12.7% in studies using non-contrast abdominal CT for stone diagnosis [19,20], 13.3% in a study conducted with trauma patients admitted to the emergency department [21], and 23% in a CT colonoscopy study [14]. The reason why this rate was low in studies conducted with mpMRI and in our study may be due to the limited imaging area of this modality. In our study, the rate of IFs and clinically significant IFs increased with age, and 3 of the clinically significant findings were found in the over 75 age group and 12 in the 65-74 age group. In total, we detected 15 of the 22 IFs (68.2%) in patients over 65 years old. As reported in the literature, an increase in patient age increases the incidentally detected findings. It has been reported that the rate of clinically significant IF is 4 times higher in patients over 80 years compared to those in the 18-30 age range [20]. In our study, when we evaluated the patient groups aged under and over 65 years, the rate of clinically significant IFs was approximately 2 times higher in the latter.
Our study has certain limitations. The first concerns the retrospective design. Second, the pathology results of some of the IFs in the clinically significant category were not available. A further limitation is that we did not evaluate the contribution of each MRI sequence to the detection of IFs. Finally, there is no standard in the classification in the literature to distinguish between clinically significant and non-significant IFs. For this reason, our classification may have caused some errors when comparing our data to the studies in the literature.
Conclusions
IFs are frequently encountered during imaging. However, because the prostate mpMRI examination is a relatively new protocol, there are only a few studies in the literature that have determined the rate of IFs using this imaging modality. This should be kept in mind while evaluating all imaging methods of IFs. The existence of IF findings and the detection of clinically significant IFs are important in many aspects. Although the clinically significant IF rate is relatively low (6.9% in our study), the rate of clinically significant IFs is high in patients undergoing prostate mpMRI, especially in those over 65 years old. It should not be forgotten that with the early detection of these findings in the asymptomatic period, the survival and treatment chances of the patients increase.


