Introduction
Infectious spondylodiscitis (also referred to as vertebral osteomyelitis, discitis-osteomyelitis complex, infectious spondylitis/discitis) is an infectious process of vertebrae, disc space, and/or adjacent paraspinal soft tissue. Its incidence is approximately 2.4 cases per 100,000 population, which increases with changes in epidemiology favouring older age groups [1,2]. The most common factors implicated for increasing incidence include increasing age, intravenous drug abuse, immunocompromised status, and worldwide increase in spinal interventions and spine surgery [3]. The most common causative microorganism is Staphylococcus aureus bacteria [1]. Infection reaches the spine most commonly through a haematogenous route; however, other sources include direct inoculation during surgery or trauma and from contiguous spread of an adjacent soft tissue infection. The microorganisms become lodged in the end arteries of subchondral plates of vertebral bodies, from where the infection spreads to the adjacent intervertebral disc and subsequent vertebral body endplate, resulting in an osteomyelitis-discitis complex. The infection and inflammatory response cause regional oedema and tissue breakdown, ultimately resulting in bone destruction [4]. Because of nonspecific clinical presentation of fever, malaise, and back pain and variable elevation of inflammatory biomarkers, a delayed diagnosis is not unusual. The delay is crucial because the complications include abscess formation, orthopaedic and neurological complications from vertebral collapse, and even death.
Infectious Disease Society of America guidelines re-commend spine magnetic resonance imaging (MRI) and obtaining blood culture and/or image-guided tissue biopsy in suspected cases [1,5]. While MRI is the modalityof choice for early detection [3], image-guided spinal biopsy plays a crucial role in the definitive diagnosis via tissue sampling, as well as to tailor antibiotic therapy to the specific organism.
During the treatment of infectious spondylodiscitis,follow-up MRI is frequently performed to monitor response to treatment, evaluate persistent or worsening symptoms, and suspected complications. In returning patients with persistent or worsening symptoms, repeat MRI often demonstrates worsening bony destruction. This may be perceived by medical and infectious disease clinicians in appropriate clinical settings as ongoing or recurrent infection, leading to the request for repeat image-guided biopsy (Figure 2). The aim of this study was to determine MRI features that could help differentiate the bone destruction due to persistent/recurrent infection from worsening bone destruction due to mechanical factors in which repeat biopsy would yield negative results. In particular, we hypothesized that worsening bone destruction does not necessarily indicate ongoing or recurrent infection but can be due to physiological and mechanical factors from the temporal evolution of the disease process; bone resorption from the initial infection can lead to continuing bone turnover during the reparative process.
Figure 1
Typical magnetic resonance imaging features of infectious spondylodiscitis. Sagittal (A) T1- and (B) sagittal T2-weighted images of lumbar spine demonstrate abnormal marrow signal intensity in vertebral bodies, destruction of endplates, and abnormal T2 hyperintensity in intervertebral disc space.Axial (C) and sagittal (D) post-contrast T1-weighted images demonstrate abnormal marrow enhancement, as well as abnormal enhancing soft tissue thickening in paraspinal and epidural space (white arrows in C and D)

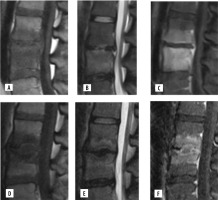
Figure 2
Magnetic resonance imaging features in a case of negative repeat spinal biopsy. 23-year-old female with infectious spondylodiscitis, presenting with persistent backpain after 6 weeks of medical treatment. Initial MRI lumbar spine with and without contrast (A-C). Sagittal T1 (A), sagittal T2 (B) and sagittal postcontrast T1 fat-saturated (C) images demonstrate abnormal marrow oedema and enhancement of L3-L4 vertebral bodies, endplates, and abnormalT2 hyperintensity in intervening disc. There is also abnormal epidural soft tissue thickening and enhancement. Repeat MRI without and with contrast (D-F).D) Sagittal T1-, (E) sagittal T2-, and (F) sagittal post-contrast T1-weighted images demonstrate worsening destruction of endplates, central wedging of vertebral bodies, and persistent abnormal marrow oedema and enhancement. However, there is improvement in the epidural soft tissue enhancement.Repeat biopsy of L3 was negative for any pathogen
Material and methods
After receiving exemption of review from our institutional review board, we performed a single-centre retrospective study. All potential cases of infectious spondylodiscitis were reviewed from January 2011 to August 2018. We selected subjects over 18 years of age, who were diagnosed with infectious spondylodiscitis, who underwent at least 2 spinal interventions for the diagnosis at the same level, and had MRI prior to each intervention. The exclusion criteria were subjects less than 18 years of age, the presence of spine hardware, and recurrence of infection at different vertebral levels. The first MRI and spinal intervention was done at the time of initial diagnosis. Repeat MRI followed by spinal intervention was done for suspected recurrence or worsening primary infection.
MRI was performed on a 1.5T Siemens machine. Our MRI protocol included pre-contrast sagittal T1, T2, and STIR, coronal T2, axial T1- and T2-weighted sequences, and post-contrast axial and sagittal T1 FS sequences. The spinal interventions varied on a case-by-case basis and included CT-guided core needle biopsy with or without aspiration of the vertebrae, intervertebral disc, and sampling of paravertebral or epidural abnormalities. The most accessible abnormality was targeted for tissue sampling. All interventions were performed by 2 experienced interventional neuroradiologists. All specimens were sent for pathology and microbiology analysis.
Analysis of MRI before the first and repeat spinal interventions was performed. Imaging findings in patients who were diagnosed as having recurrent or repeat infection were compared with those not diagnosed with recurrent or repeat infection following repeat imaging and intervention. The dia-gnosis of recurrent infection was made by infectious disease clinicians based on pathology/microbiology results and clinical presentation. Moreover, all patients who were allocated to the non-infectious cohort following repeat spinal intervention received no further treatment with antibiotics.
The following MRI features were examined: vertebral and paravertebral changes that included expansion/disruption of the vertebral body cortex and surrounding collections, best seen on axial T1 fat-saturated (FS) post-contrast images; epidural changes including thickening or collections, best seen on sagittal T1FS images; and bone marrow signal changes on T1 and T2 FS/short tau inversion recovery (STIR) sequences; vertebral body destruction, assessed by analysing changes in height, measured in craniocaudal dimensions on sagittal images from the most depressed areas of the end plate, which was thought to be associated with the infectious process and not degenerative; intervertebral disc changes including abnormal T2 hyperintensity and loss of disc height.
Results
Seventeen patients met our inclusion criteria; 10 out of 17 patients were diagnosed with recurrent infection, and 7 patients were categorized as having no recurrent infection by the clinicians following repeat imaging and spinal intervention. The patients’ demographics and prepon-derance of thoracic and lumbar spine involvement in the 2 cohorts were similar (Table 1).
Table 1
Patients’ characteristics
The initial and repeat MR imaging were reviewed for changes in the selected imaging parameters, and a comparison was made between the 2 cohorts (Table 2). Worsening paravertebral changes were seen on repeat MRI in 8 out of the 10 patients with recurrent infection; however, these were not seen in any patient without recurrent infection (p = 0.006). Out of 7 patients with no recurrent infection, there was improvement in the paravertebral soft tissue changes in 6 patients and near-complete resolution of paravertebral changes in one patient. Two out of 10 patients in the recurrent infection cohort showed improvement in the paravertebral changes. New or worsening epidural soft tissue thickening and fluid collection was seen on repeat MRI in 9 out of 10 patients with recurrent infection; however, this was not seen in any patient without recurrent infection (p = 0.002). The repeat MRI of 6 out of 7 patients without recurrent infection cohort demonstrated improvement in epidural soft tissue changes, and there was complete resolution in one patient. One subject in the recurrent infection cohort had improvement of epidural findings on repeat study.
Table 2
Assessment of worsening MRI findings on repeat examination
Worsening vertebral marrow signal changes on follow-up MRI were seen in 5 out of 10 patients with recurrent infection and 3 out of 7 patients without recurrent infection, with no statistically significant difference (p = 0.838).
Follow up MRI of majority of patients in both cohorts demonstrated worsening destruction of the vertebral body (90.0% vs. 57.1%, p = 0.321) and intervertebral discs (90.0% vs. 86.0%, p = 0.621). Abnormal intervertebral disc signal was seen in 8 out of 10 patients with recurrent infection and 3 out of 7 patients without recurrent infection (80.0% vs. 43.0%, p = 0.288).
The rate of vertebral body height loss per day was also analysed (Table 3) for both superior and inferior vertebral body height loss, as well as the average loss of both. The average rate of loss of vertebral body height per day was 0.553% in the recurrent infection cohort and 0.103% in the non-recurrent infection cohort (p = 0.050). The rate of loss of height per day of inferior vertebral body was greater in the recurrent infection cohort than the non-recurrent infection cohort (0.632% vs. 0.085%, p = 0.043). There was no statistically significant difference between the 2 cohorts in the rate of loss of height per day of the superior vertebral body (p = 0.073).
Table 3
Percentage of loss of vertebral body height per day
Discussion
Infectious spondylitis can cause serious neurological disabilities and can prove fatal; therefore, prompt and definitive diagnosis is of paramount importance. Plain radiographs are the first-line investigation in suspected cases but have low specificity, and loss of vertebral body height is the most common finding. CT scan is more sensitive in detecting vertebral osteolysis; however, it takes 3-6 weeks after the onset of symptoms for bone destruction to appear on imaging, thus causing a significant delay in the diagnosis [3]. The ability of MRI to show early bone marrow oedema with high sensitivity (96%) and high specificity (94%) makes it the modality of choice for early detection [3]; T1 and short tau Inversion recovery (STIR) are the most sensitive and specific sequences, and they can detect alteration of normal bone marrow as early as 1 to 2 days after the onset of infection [4]. Moreover, better spatial resolution and tissue characterization of MRI provides details of paraspinal soft tissues and epidural space (Figure 1).
MRI is also frequently performed during the course of treatment, to evaluate the efficacy of treatment or when there is suspected complication or relapse of infection. The utility of MRI in the diagnosis of infectious spondylodiscitis is undoubted; however, its utility in the follow-up of spine infection has not been proven. Multiple studies have shown that radiological improvement lags behind clinical improvement. In fact, in many cases follow-up MRI shows stable or worsening bone destruction despite clinical improvement [6]. Persistent or recurrent backpain in patients on medical treatment is a diagnostic dilemma for clinicians, which prompts them to investigate for treatment failure or relapse of infection. Relapse or recurrent infection is not uncommon and has been noted in 1-22% of cases even with the use of modern antibiotics [7]. However, 2 separate studies by Kowalski et al. and Carragee have shown that in follow-up MRI in such patients performed within 4 weeks of commencement of treatment, imaging findings are either unchanged or appear worse, overestimating the treatment failure [8,9]. Worsening imaging findings prompt clinicians to request repeat spinal biopsies.
The yield of repeat percutaneous biopsy is variable in the literature. A systematic review of 8 studies by Kasalak et al. showed that the positive culture yield of a second CT-guided biopsy ranged from 10 to 50% [10]. Another study of 30 patients with negative initial spine biopsy and blood culture demonstrated a repeat biopsy yield of 60% [11].Differences in the biopsy technique, target anatomic structure, provider, and above all previous or ongoing anti-biotic therapy are important reasons for the variable and low yield of the biopsy [12]. Not only does repeat intervention add to medical costs, but also complications are more likely in repeat sampling, especially in patients with debilitating illness or comorbidities [13].
We studied the imaging features of spine infection on 2 successive MRIs and attempted to differentiate the changesof healing and worsening infection or relapse. This, in turn, can help select appropriate patients for repeat spine biopsy.
In our experience paravertebral and epidural soft tissue changes on MRI can help differentiate between the 2. We observed that in patients with recurrent/persistent infection, the paraspinal soft tissue thickening and enhancement was worse than or similar to the initial scan. Similar changes were seen in epidural space, with increased soft tissue thickening and new or worsening epidural fluid collections in the recurrent infection group. Conversely there was improvement in paravertebral and epidural soft tissue changes in patients with no recurrent infection [14]. The difference was statistically significant and supported by studies by Gillams et al. and Veillard et al.Gillams et al.postulated that a decrease in the amount of soft tissue and enhancement was the first sign of healing, which was seen in 8 out of 14 patients (57%) in their study [15]. Veillard et al. observed improvement in paraspinal and epidural abscess as the only sign of healing in the first month of antimicrobial treatment [16]. Kowalski et al. showed improvement in comprehensive soft tissue findings in 21 out of 32 patients; however, they could not find a single statistically significant MR finding to differentiate between a group of successfully treated patients and patients with no clinical improvement and treatment failure [8].
We calculated the rate of loss of vertebral body height involving the superior and inferior end plates and the aver-age of the 2. The rate of loss of inferior vertebral body and the average of both was significant in the recurrent infection group, suggesting that this parameter can also be used for differentiation. To our knowledge, no other study has analysed this finding, and although it is statistically significant, this is a crude observation that requires a greater sample size to establish a precise rate at which height loss is suggestive of recurrent infection and not a result of expected mechanical failure.
It is interesting that the most visible changes on follow-up MRI, including destruction of vertebral body and intervertebral disc, abnormal vertebral marrow signal changes, and abnormal signal in intervertebral disc, do not indicate worsening infection or recurrence. Progression of vertebral and disc destruction and signal changes are routinely seen in patients with good clinical response to antimicrobial therapy. Carragee found overall worsening of MR imaging findings in 7 out of 8 patients despite clinical improvement [9]. Kowalski et al. found no significant difference in vertebral body collapse, and marrow and disc signal changes on follow-up MRI between patients with recurrent infection and patients with clinical improvement [8]. The pathophysiology of vertebral changes in patients with clinical improvement is unknown; however, this may be related to increased vascularity and granulation tissue as a healing response. This can also weaken the bone, resulting in mechanical fracture, which can be perceived as worsening infection. In a study by Gillams et al., 8 out of 14 patients demonstrated decreased soft tissue changes with clinical improvement; however, 6 out of these 8 patients showed worsening signal changes and destruction of vertebral bodies and disc space [15].
Spinal epidural abscess in the setting of spine infection is a known complication due to septic thrombosis of epidural veins [3]. Other known MRI features of intramedullary abscess and subdural empyema are extremely rare, with only 120 of the former reported cases since 1830, and the latter being a neurosurgical emergency [3]. These features were not present in our subjects, and they were not the target of our study.
Limitations of our study include its retrospective nature and small sample size. Inherent limitations of accuracy of spinal biopsy exist in our study, and thus patients were allocated to either the recurrent infectious cohort or non-recurrent infectious cohort based on the established diagnosis of the clinician, who considered all factors of the patient (clinical presentation, laboratory findings, MRI findings, and pathology results). Negative pathology results from a specimen acquired at the time of spinal intervention did not necessitate a non-infectious diagnosis. Moreover, all patients in the no recurrent infection group received no further antibiotic treatment, and thus there was no impact on the clinical course as a result of the negative repeat spinal biopsy.
Conclusions
In patients of infectious spondylitis with suspected recurrence, the most common and pronounced MRI findings can be deceiving and can result in repeat spinal biopsy. Repeat biopsy has no better yield, and its usefulness has not been proven. Our study has shown that increased destruction and signal changes in vertebrae and intervertebral discs is not a definitive indicator of worsening or recurrent infection and could also be due to healing response. However, changes in paraspinal and epidural soft tissues can help differentiate the cause of worsening bone destruction. Improvement in paraspinal and epidural soft tissue thickening indicates a favourable response to treatment in spite of worsening changes in vertebrae and disc space. It is suggested that risk stratifying patients clinically with pain, fever, focal, or worsening neurologic signs, and inflammatory markers and observing soft tissue changes on follow-up MRI is a more reliable way to identify patients who may benefit from repeat spine biopsy.


