Introduction
Intracranial aneurysms are estimated to occur in 3% or even up to 5-10% of the global population [1]. Traumatic intracranial aneurysms are uncommon and constitute less than 1% of all cases. Pseudoaneurysm after penetrating head injuries are more often located peripherally. Iatrogenic aneurysms are usually a result of direct trauma to the arterial wall during various neurosurgical procedures for tumours, aneurysms, and trauma of the skull base and most often involve the internal carotid artery [2,3]. The real incidence of these lesions is uncertain and the discovery of them may depend on the timing of performed angiographic examinations [4].
Single cases of pericallosal posttraumatic and postsurgical aneurysms were previously reported [5,6]. Herein, we report the first confirmed case of an iatrogenic pericallosal artery aneurysm (periAA) caused by an arterial wall injury during the endovascular treatment of another aneurysm. A dissecting unruptured aneurysm that was detected in control examination was successfully treated with stent-assisted coiling.
The treatment strategies of iatrogenic aneurysm include both surgical and endovascular procedures and should be based on the patient’s clinical data [5]. Because traumatic aneurysms are fragile, prone to rupture, and surrounded by arachnoid scarring, endovascular treatment seems to be the primary option.
Case presentation
Initial treatment
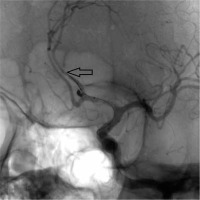
A 50-year-old woman with subarachnoid haemorrhage (4 in the FISHER Scale) was admitted to the Department of Neurosurgery. Computed tomography angiography confirmed the presence of a small (3 × 1.5 mm) anterior communicating artery aneurysm (ACoA). The patient was qualified for endovascular treatment. Balloon-assisted coiling of the ACoA was performed under general anaesthesia. Digital subtraction angiography (DSA), performed after the procedure, showed the contrast opacification within the neck of the aneurysm, which equals class II of Raymond-Roy Occlusion Classification (RROC). During the procedure the tip of a microwire (Traxces 14, Microvention Terumo Inc.) inserted into the balloon catheter (Scepter XC, Microvention Terumo Inc) placed in the left pericallosal artery caused local irritation of the inner layer of the vessel wall and vasoconstriction over a length of 1.5 mm, without bleeding, dissection, or flow disturbances visible in DSA (Figure 1).
Follow-up after 1 year
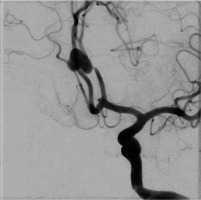
The control DSA examination performed 12 months after the endovascular procedure of the ACoA revealed a dissecting saccular aneurysm, irregular in shape, about 12 × 6 mm in diameter, in the place of the previous vasoconstriction of the left pericallosal artery in the A2 segment (Figure 2). The occlusion of coiled ACoA was similar as after the procedure.
The treatment
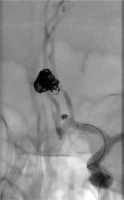
After 5 days of standard dual antiplatelet oral preparation (ASA 150 mg, clopidogrel 75 mg) stent-assisted coiling of the periAA was performed. DSA showed 3-mm-long stenosis of the vessel lumen at the level of the aneurysmal neck (Figure 3). Using the jailing technique a Leo baby stent 2.5 × 25 mm was implanted into the A2 segment of the pericallosal artery, and the aneurysm was embolised with platinum coils. Control angiography showed residual filling of the base of aneurysmal sac (RROC III). Occlusion of the previously treated ACoA remained the same. The patient had no neurological impairments, and the procedure appeared to be without complications.
Follow-up after 6 months
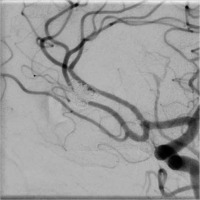
After 6 months the patient underwent a control DSA examination, which showed entirely cured pericallosal artery aneurysm (RROC I) and improvement of the expansion of the parent vessel. Anterior communicating artery aneurysm remained stable, with inconsiderable residual neck (RROC II) (Figure 4).
Discussion
Technical development of endovascular neurointerventions allows treatment of a greater number and anatomically more complicated aneurysms using additional balloon catheters, stents, and other instruments. The growing number of devices inserted at the same time inside the artery lumen in a single procedure increases the risk of complications such as perforation, dissection, or thrombus formation.
Until this case there had not been any documented iatrogenic cerebral aneurysm after endovascular procedure. Most reported aneurysms appeared after different neurosurgical vascular and nonvascular procedures [2,3].
Successful endovascular treatment of iatrogenic pericallosal aneurysm was previously reported, and this method seems to be the first-choice treatment [5-7]. In our case, endovascular stent-assisted coiling allowed safe exclusion of pericallosal dissecting aneurysm from circulation, and the implanted stent enabled reconstruction of the parent artery, restoring the normal lumen diameter. The second considered endovascular treatment option was implantation of a flow-diverted stent into the pericallosal artery [8,9]. However, we found this method to be riskier, causing more potential complications due to the need to use greater force to deliver a larger microcatheter and flow diverter stent into the pericallosal artery with coexisting artery stenosis and not completely cured ACoA aneurysm.