Introduction
Listeriosis is an infectious disease caused by Listeria monocytogenes – Gram-positive intracellular bacteria [1,2]. The estimated dose that could pose a threat of falling ill is 107-109 CFU for people who do not have any high risk factors; however, for the high-risk population the CFU is estimated to be 105-107 [2].
Listeria monocytogenes is a widespread pathogen that was isolated for the first time in 1918 from cerebrospinal fluid (CSF) [3]. This Gram-positive intracellular bacteria has a wide range of abilities – it is capable of enduring harsh environments such as low temperature, pH, and sanitisers [4,5], and of forming biofilm which, as a result, help bacteria survive the processing of food [5]. Thereby, it can be spread via numerous types of foods [4,5]. Studies have shown that both people and animals, including wild and domestic species, can be asymptomatic carriers of L. monocytogenes. It highly depends on the region; for example, the rate of L. monocytogenes found in the faeces of people from Austria, Germany, or the USA is below 1%, whereas in Iran it is 7.5% [6].
Infection of L. monocytogenes is typically limited to fever, diarrhoea, and gastrointestinal inflammation [4]. However, in people who are immunocompromised such as on post-transplant treatment, the elderly, patients with diabetes, or pregnant women, it might be linked to be a cause of meningitis [4,7]. Moreover, usage of stomach acid suppressors such as proton pump inhibitors can make the passage through the stomach and invasion of enterocytes easier for L. monocytogenes [4]. In addition, there is a high chance of infection in the population that is treated with infliximab [8]. However, immunocompetent people cannot be excluded from central nervous system (CNS) invasion by L. monocytogenes [9]. It is estimated that L. monocytogenes causes CNS infections in 47% of infected patients, leading to death for 37% of them [10].
The CNS infections can be demonstrated in the form of meningoencephalitis, rhombencephalitis, brain abscesses, or meningitis [11]. It is said that L. monocytogenes is the second agent after Streptococcus pneumoniae responsible for acute bacterial meningitis (ABM) in immunocompromised patients. The majority of the group are people with cancer, corticosteroid treatment, and people who undergo immunosuppressive treatment [12]. It is more common to find abscess caused by L. monocytogenes in subcortical grey matter than for other reasons [13]. In adults, L. monocytogenes is one of main reasons for bacterial meningitis [14].
There are several methods for the laboratory diagnosis of L. monocytogenes, including blood culture, cerebrospinal culture, and metagenomic next-generation sequencing (mNGS) of the CSF, which is a relatively new method of diagnostics. In comparison to other methods, the mNGS is characterised by high sensitivity, wide range of detection, and faster results [15]. There were also investigations into the use of real-time PCR targeting the hly gene, which encodes listeriolysin O, the main factor of virulence of the bacteria. A significant advantage of this method over the isolation of bacteria in CSF is the fact that this method can help us find bacteria in the CSF even after starting antibiotic therapy, whereas isolation could give a negative result. What is more, in comparison to isolating bacteria from CSF, real-time PCR, as well as NGS, is characterised by high sensitivity and rapid time of detection of the pathogen. However, real-time PCR is not a common form of diagnosing L. monocytogenes from CSF due to lack of prospective research confirming its accuracy [16]. Diagnosing the presence of L. monocytogenes in CSF using Gram stains and cultures is challenging. The low positivity rate of L. monocytogenes in CSF and the similarity in CSF findings between bacterial and viral infections make the diagnosis deceptive [17]. However, we can find some abnormalities that are characteristic to bacteriemia in CNS. Elevated cell counts, protein levels, and high intracranial pressure are commonly detected [17,18]. Moreover, CNS infections caused by L. monocytogenes are associated with an elevated monocyte count in the blood, which can substantially help in establishing a diagnosis [18].
Imaging methods
Computer tomography is an excellent imaging technique for detecting the pathologies of the central nervous system; however, due to significantly lower spatial resolution, it exhibits lower sensitivity in identifying lesions that are characteristic of a specific pathogen. Despite some limitations, computed tomography (CT) remains a widely available imaging method, with short acquisition time, which is crucial in emergency cases.
CT proved not to be useful enough in diagnosing encephalitis linked to L. monocytogenes [11]. However, in up to 50% of immunocompromised patients, macroscopic brain abscesses can be observed, located in pons, medulla, thalamus, or subcortical area [11]. In patients with meningoencephalitis caused by L. monocytogenes CT scans can present multiple microabscesses in the brainstem and cerebellum [19].
In recent years, MRI has undergone significant development, including modern imaging protocols that use artificial intelligence algorithms. This improvement highly accelerated individual sequences, without compromising their quality. Furthermore, MRI, because of its superior contrast resolution, allows us to visualise much greater detail in soft tissues, including the brain mass. This advantage is crucial in detecting brain pathologies, including the CNS invasion of L. monocytogenes. In comparison to CT, MR can more accurately identify ring-enhancement lesions or brain abscess; that is why MRI is considered to be a golden standard of diagnostics in CNS pathologies.
In MRI typical detected findings are rhombencephalitis and meningitis. It is not common to report features of abscesses [14]. MRI is considered to be more effective than CT for the detection of abnormalities in patients with brainstem diseases, such as rhombencephalitis [20]. However, rhombencephalitis is a rare form of neurolisteriosis [21]. It is claimed that complications such as hydrocephalus and intracranial haemorrhage may occur in 3% of patients with neurolisteriosis [22].
In a case report by Zhang et al. [23], on the day of admission a 64-year-old farmer with a history of tuberculosis and TIA (transient ischaemic attack) was initially diagnosed with acute ischaemic stroke according to cranial CT that exposed bleeding. However, further head CT-angiography did not confirm any indications of occlusion or stenosis of the cerebral artery. MRI of the brain revealed enhancement of the meanings and abnormal signals in the insula and left thalamus not associated with infarction. On the third day, CT and SWI indicated subarachnoid haemorrhage. Later, the mNGS test was performed on the patient to determine if L. monocytogenes was to blame for intracranial infection with arachnoid haemorrhage. Finally, this intracellular bacterium was detected.
The team led by Jiang et al. [24] reported a case of 71-year-old woman who had a history of type II diabetes for over 20 years. For the past 6 years she had been taking insulin aspart to control her blood glucose. Four months prior to her admission to the hospital, she had experienced chest tightness, which disappeared after rest and dyspnoea. One month before admission to the hospital, those symptoms were aggravating. In conclusion, the patient came to the emergency department and was diagnosed with heart failure. Doppler ultrasound indicated reduced left ventricular function value and ejection fraction (EF) of 34%. In the afternoon, the patient’s temperature rose to 40°C, and she had facial and limb convulsions, and disturbance of consciousness. An MRI of the brain was performed, which suggested an infarct lesion in a left temporal lobe. After admission to the intensive care unit, the lumbar puncture was done, and CSF was obtained. Blood culture, sputum culture, and CSF were firstly negative for Gram stain. However, on the third day after admission, the culture of CSF resulted as positive for L. monocytogenes. Diagnosis of L. monocytogenes infection was stated.
Frade et al. [25] unveiled a case in which a 74-year-old female was admitted to hospital. For the past 4 days she had been experiencing a headache. In her past medical history were post–traumatic seizure disorder treated with levetiracetam, coronary artery disease, supraventricular tachycardia treated with diltiazem and amiodarone, and migraines. Over the course of the day, the patient developed left–sided hemiparesis. T2-weighted MRI and FLAIR had increased signals in a subcortical right hemisphere lesion. A second MRI was performed, revealing hyperintense lesions in the right basal frontal and temporal lobes, brainstem, and thalamus. On the fifth day of admissions, the biopsy of a lesion was done, accompanied by lumbar puncture. MRI with contrast showed ring enhancing lesions in midbrain, thalamus, temporal, and right basal frontal lobes. The CSF culture came positive for L. monocytogenes.
A case report by Li et al. [26] involves a 37-year-old male who presented with fever over 38°C, headache, dystrophy, and dysphoria for one day. The CT scan of the head showed a reduction in density of the brain, swelling of it, and hydrocephalus. The CSF and blood culture tests resulted in the detection of L. monocytogenes. It is a rare case because these bacteria rarely have an effect on immunocompetent adults.
The team led by Xu et al. [27] demonstrates the case of a 2.5-year-old girl who was admitted to the hospital due to a 3-day history of fever and vomiting, complicated by a seizure lasting half a minute on the day after admission. In cranial MRI, which was done during the third day of admission, the right subdural effusion in T2 was revealed as well as a marked hyperintense lesion in the splenium of the corpus callosum. DWI (diffusion-weighted images) and FLAIR had reduced apparent diffusion coefficient mapping. From CSF L. monocytogenes was detected.
In a case report by Carrillo-Esper et al. [21] a 66-year-old man with a medical history of type 2 diabetes mellitus and cirrhosis was urgently taken to the emergency department with sudden worsening of his mental condition. The patient reported experiencing intermittent fevers and low–intensity headaches in the previous month. MRI of the head was performed. It revealed dilatation of both lateral and third ventricles accompanied by transependymal migration of the spinal fluid. After contrast administration, a T1-weighted MRI of the cranium revealed enhancement in the spinal medulla, cerebral peduncles, and cerebral fissures. Both blood and CSF cultures revealed L. monocytogenes. After finishing appropriate antibiotic treatment and achieving full recovery, the MRI was performed again and revealed remission of the previously observed abnormalities.
Liang et al. [22] described a case of a 29-year-old male who was admitted to the hospital complaining of forehead headaches and intermittent fevers that lasted for 2 days. His history of present illness included consuming unpasteurised cooked beef that had been stored in the refrigerator for a few days. After initial brain CT, which did not show any pathologies, MRI was performed on the fourth day of admission. Axial T2-FLAIR imaging revealed a hyperintense lesion in the right pons. What is more, there were noticeable prominent temporal horns along with the enlargement of the ventricles. In this case, complications such as hydrocephalus and haemorrhagia of the lateral ventricle occurred, leading to the patient’s death.
In a case report by Zhang et al. [28] a 59-year-old male had a diagnosis of acute cerebral infarction. His initial symptoms were weakness of the right upper limb accompanied by aphasia and numbness but no fever. The CT scan of the brain revealed a low-density cystic mass in the left frontoparietal lobe with an oedema zone. The patient also had a brain MRI, which revealed a cystic-solid mass of 3.0 cm in the frontoparietal lesion with equal mixed T2 signals and low T1. In the DWI sequence there was a high signal in the region of the lesion and ring enhancement around it. The patient had a needle biopsy of the left-side frontoparietal mass. A bacteriological test was performed, which revealed the presence of L. monocytogenes. The diagnosis was stated: cerebral abscess due to this pathogen. The patient had a history not only of glucocorticoid treatment, but also of dental treatment and diabetes, which are risk factors for infection of L. monocytogenes.
Sakarunchai et al. [29] reported a 36-year-old female who was taking prednisolone 30 mg/day due to SLE that was diagnosed in 2002, with a high-grade fever and intensifying headache for 4 days before admission to the hospital. She also had hemiparesis of the right side with no neck stiffness. The CT scan of the brain performed with contrast disclosed weakly determined rim enhancement in the left frontal lobe, with size 2.5 × 3.7 cm. The minimal midline shift was exposed due to marked vasogenic oedema around the lesion. The MRI of the brain revealed that the lesion was not restricted to the left frontal lobe, but also stretched to the left basal ganglia via the dorsal midbrain. The sagittal view T1-weighted imaging of both frontal lobes with contrast revealed an enhanced pattern, which was compared to bead-like serpiginous tubular lesion or tunnel sign. On DWI at the left basal ganglia and left frontal lobe there was a restriction and multiloculated rim enhancement. Infection of sparganum was suspected, which later turned out to be incorrect. After surgical removal of the brain abscess, the pus was collected and L. monocytogenes was cultured.
Similar MRI findings were seen in 2 case reports by Thiankhaw et al. [14]. The first of them describes a 56-year-old man with a present history of headache, low-grade fever, and aggressive personality, lasting for 3 weeks. MRI revealed tract-like enhancing lesions surrounded by vasogenic brain oedema, located at the right parietotemporal lobe. In the second case, the authors describe a 23-year-old woman suffering from systemic lupus erythematosus (SLE) with lupus nephritis (LN), who had been taking prednisolone and mycophenolate mofetil for the past 3 months. She complained of a headache and high-grade fever. Physical examination revealed left hemiparesis. As in the previous case, the MRI showed multiple track-like enhancements in the right frontal lobe extending to surrounding areas, with the brain oedema visible on FLAIR. Centrally restricted diffusion was observed within these lesions on DWI. In both cases L. monocytogenes was responsible for the patients’ condition.
In a case report by Zhang et al. [30] a 64-year-old female was suffering from weakness of the right arm and leg for 4 days before admission. That state developed into hemiplegia of the right upper limb and right lower limb, making her unable to walk independently. She had a 10-year history of diabetes, hypertension, and nephrotic syndrome. Moreover, she was diagnosed with membranous nephropathy 6 months before admission to the hospital, for which she was taking cyclophosphamide and glucocorticoids. She denied either intake of unpasteurised cheese or modifying elements of her diet. In the enhanced brain MRI there was an uneven, well-defined lesion in the left frontoparietal junction. On the T1-weighted images there was a longer signal on the frontal parietal region of the sagittal position. On T2-weighted images the longer signal was in the left frontoparietal junction area. In DWI and FLAIR sequence it was hyperintense. In the lesion area surrounded by local mass effect and vasogenic oedema enhancement, multiple high signals with cluster distribution could be seen. From the blood of the patient the L. monocytogenes was grown.
Flores-Perez et al. [31] described the case of a 40-year-old male who had a 5-day history of headache and gait disturbance. The patient had chronic alcoholism – his consumption per day was over 160 g. Two days before admission he suspended consumption of alcohol and presented a one-minute tonic-clonic seizure without postictal state of almost 2 minutes. A nonenhanced brain CT showed lesion in the right temporal lobe. Additionally, the mucoperiosteal thickening of the maxillary sinus and left anterior ethmoidal cells were found, which corresponded to chronic sinusitis. The abdominal ultrasound exposed splenomegaly and, moreover, findings of chronic liver disease that was classified as Child-Pugh B. Later, a contrast-enhanced MRI of the brain was performed. It showed a supratentorial, intra-axial mass in the right temporal lobe. The lesion had weakly restricted borders and oedema zone. Moreover, after gadolinium perfusion in T1, it was centrally hyperintense with uneven enhancement of the wall. In addition, the lesion had a volume of 34 ml and measurements of 3.9 cm × 1.7 cm × 1 cm. Blood cultures were negative, but CFS culture revealed L. monocytogenes.
In a case report by Carneiro et al. [32] a 75-year-old patient with myasthenia gravis, treated with pyridostigmine and prednisone, had a history of hypertension and regular ingestion of homemade artisanal cheese. He was admitted to the hospital due to one week of increasing weakness of muscles and dyspnoea. On the second day after admission, he had right-sided hemiparesis, respiratory distress, and altered mental status. A CT scan of the brain disclosed microangiopathy and global atrophy. A chest CT was also performed, which revealed bilateral ground-glass opacities with areas of consolidation and small bilateral pleural effusion. Blood cultures were drawn, and L. monocytogenes was identified. After 10 days of combination antibiotic therapy, the mental status of the patient had not changed, so an MRI of the brain was conducted. In T1-weighted images in the corpus callosum and in the parietal lobes multiple ring-enhancing hypointense lesions were found that corresponded with brain abscesses. In the next MRI, which was performed after 5 weeks of treatment, the improvement was minimal. Patient died 6 weeks after admission.
The team of Brisca et al. [33] described an 11-month-old, immunocompetent girl who was admitted to the hospital presenting symptoms of high-grade fever accompanied by vomiting and diarrhoea. Additionally, the girl experienced uncontrolled movement of the right leg and sudden onsets of lethargy. All of the mentioned symptoms started 3 days before entering the emergency. During examination she was evaluated with a generalised seizure. MRI was performed immediately and revealed restricted diffusion with reduced apparent diffusion coefficient (ADC) values located in temporoparietal regions of the brain. Additionally, no leptomeningeal contrast enhancement was seen. The authors claim that these MRI findings were connected with seizures. Suspicion of meningoencephalitis led to treatment with ceftriaxone, but, after 2 days, the girl was still in poor general condition. CSF culture confirmed infection with L. monocytogenes. Despite the initiation of ampicillin and drop in fever, her neurological status worsened, and MRI was repeated. It revealed widespread inflammation, seen as a diffuse cerebrospinal contrast enhancement, accompanied by ventriculitis. The girl also developed a severe, decompensated, communicating hydrocephalus. There were no seizure–related changes. After neurosurgical confrontation and treatment with dexamethasone, the girl’s state improved.
In a case reported by Steinbrecher et al. [34] a 51-year-old patient had facial palsy and right-sided hemiparesis. The patient reported rigidity of the right ankle 3 days before admission. He also had a progressing hemiparesis that started from the right leg. In the medical history of the patient there was no immunodeficiency confirmed. Moreover, the intake of either over-the-counter or prescribed or illicit drugs were denied. There was an indication of long-term nicotine abuse. A continuing consumption of dairy products was reported. The patient had an elevated HbA1c (value of 9.1%) and elevated serum glucose levels resulting in a diagnosis of diabetes mellitus type II. Treatment started with needs-based rapid-acting insulin; however, it was changed to oral intake of metformin according to endocrinological recommendation. Colour-coded duplex sonography was performed, and it denied the existence of haemodynamically relevant stenosis of the brain-supplying arteries that was first suspected in MRI. Moreover, the MRI of the brain was carried out – there was an enhancement of signal in the left frontal lobe that extended to the corona radiata. The uncertain diagnosis of an infarction of the anterior cerebral arteria was made. Hence the patient was taking 100 mg acetylsalicylic acid daily. In addition, he was admitted to the stroke unit. Moreover, the transcranial Doppler ultrasonography, which was done daily, denied accelerations of cerebral vessel flow. After one day the MRI was once more analysed, and the diagnosis was changed to angiocentric lymphoma. The cranial CT scan was performed 2 days after the first MRI. The CT scan showed lesions and denied cerebral infarction – due to which, the therapy with acetylsalicylic acid was stopped. Six days after admission, an open cerebral biopsy was performed – during the procedure, the irregular abscess that extended from the left medial frontal gyrus to the basal ganglia was resected. Cultural findings revealed L. monocytogenes infection.
The team of Ogunleye et al. [35] described a 70-year-old male who had acute alteration of mental state, and weakness of the right side that was linked to shuffling gait. He had a history of asthma, and chronic immune thrombocytopaenia that was resistant to high doses of steroids and fostamatinib. Moreover, the patient had diabetes mellitus. Additionally, one week earlier, he had a splenectomy for chronic immune thrombocytopaenia and right hemicolectomy for a caecal mass with high-grade dysplasia. CT scan of the head was performed without contrast. It exposed a mass effect in the left frontal lobe with an oedema zone that caused a midline shift from left to right. Later, an MRI of the brain was performed, which revealed irregular rim enhancement lesion in the left frontal lobe with oedema zone and mass effect. Craniotomy was conducted. The excision was made in a left frontal lobe due to suspicion of high-grade glial neoplasm. However, necrosis suggested cerebral abscess. Therefore, blood cultures were drawn, which revealed L. monocytogenes.
Nachmias et al. [36] described 2 cases. The first presented patient was a 72-year-old man who had a fever and felt general weakness for 2 days. From other symptoms the patient also had abdominal lymphadenopathy and sub-acute weight loss. Moreover, the laboratory tests exposed elevated LDH and pancytopaenia. Intravenous ceftriaxone and ciprofloxacin were given as empirical treatment. A bone marrow biopsy was performed – it revealed infiltration of diffuse large B-cell lymphoma. Brain CT was performed, and no aberration from norm was found. Later, a lumbar puncture was done, which revealed bloody CSF with high–level of protein (942 g/dl) and low glucose (16 mg/dl). Bacterial culture was negative due to the treatment. Ampicillin was added due to suspicion of L. monocytogenes. Four days later an MRI was performed. In T2 and FLAIR there were enlargement of the third and lateral ventricles with transependymal CSF oedema. There was neither mass effect nor haemorrhage to be found. After a 21-day course of ampicillin there was great neurological and clinical improvement. The second presented patient was a 56-year-old man who had metastatic lung adenocarcinoma. Two days before the admission, the patient had a low-grade fever and somnolence. Due to possible systemic infection, intravenous ceftriaxone and ciprofloxacin were initiated. Blood cultures were drawn, which revealed L. monocytogenes. Ampicillin was added. Head CT showed a non-obstructive ventriculomegaly.
In a case report by Lee et al. [37] a 7-year-old girl had a periodic fever of over 38oC, abdominal pain, and watery diarrhoea that lasted for 6 days. The patient also had a severe headache, vomiting, and lethargy. The patient was vaccinated against Haemophilus influenzae type b and had conjugated pneumococcal vaccines. The girl had never been introduced to domestic animals or contaminated food. The patient had Kernig sign, Brudziński sign, and neck stiffness positivity. Moreover, the reflexes of the lower limbs were hyper-reactive. She was treated with ceftriaxone and amikacin. Before the results of the cultures were presented, the patient also had steroid injections. On the second day of hospitalisation the vancomycin was added due to continued fever. An increase in the intracranial pressure was suspected. Therefore, a brain MRI was performed. There was no evidence of abnormalities in size of the ventricles and oedema. On the third day L. monocytogenes was confirmed from the blood test and CSF, due to which, ampicillin was added. On the fourth day, the patient had slowed pupillary reflexes and nystagmus was observed. There was also a decrease in muscle strength to grade 2. The girl was given ventilator support after transfer to the intensive care unit. The CT of the brain was performed. It revealed parenchymal oedema, hydrocephalus, and extrusion of the brain stem accompanied by increasing lateral, third, and fourth ventricles. Drainage was done. However, after a few days the condition of the patient was not improving. Moreover, the hydrocephalus was worsening, so on the 22nd hospital day a ventriculoperitoneal shunt procedure was done. On the 38th day in the hospital, a brain CT was performed, which revealed parenchymal oedema, and hydrocephalus communicating with ventriculostomy. After 61 days the girl recovered and was discharged.
Mahpara et al. [38] demonstrated fatal complications of L. monocytogenes invasion of the central nervous system. They described a 74-year-old female who had been hospitalised with a history of intermittent fever, vomiting, and diarrhoea for 10 days. Additionally, for the past 2 days she had experienced altered sensory perceptions, and while being hospitalised, she had one episode of generalised seizures. She had been treated with empirical antibiotics for bacterial meningitis at another hospital. Her past medical history included breast cancer accompanied by hypertension and type 2 diabetes mellitus. During the physical examination, she exhibited nuchal rigidity and tested positive for Brudzinski’s sign. CSF examination indicated elevated markers of infection, and Gram staining identified the presence of coccobacilli-like bacteria. On day 8 L. monocytogenes was cultured from the blood. After undergoing intravenous ampicillin treatment, her brain CT scan showed no abnormalities. Suddenly, after 3 weeks, the patient was admitted again presenting sudden deterioration of consciousness. Laboratory results were normal, with no growth from the blood culture. A non-contrast CT scan of the brain revealed an intracerebral haemorrhage. Three days later, a follow-up CT scan showed that the haemorrhage had extended to the right ipsilateral ventricle. Neurosurgical intervention was performed, and ventricular drainage was established. Unfortunately, the patient’s condition did not improve, and she died.
Mohan and Sufyaan [39] described a 56-year-old man who presented in the emergency room with slurred speech and generalised body weakness that had lasted for one week. He had no past medical history. Blood gas analysis showed an oxygen saturation (SpO2) 85%. Neurological examination revealed left facial asymmetry. Biochemical results indicated an increase in white blood cells, with C-reactive protein (CRP) levels at 40 mg/l. Additionally, troponin I levels were elevated, although there were no findings on the ECG. Chest radiography was performed, which revealed bilateral lower zone consolidations. What is more, brain CT revealed multifocal chronic infarcts. The patient developed respiratory distress, leading to intubation. He was given antiplatelet treatment and anticoagulants for a non-ST elevation myocardial infarction and multifocal old cerebral infarcts, as well as intravenous ceftriaxone for pneumonia. After 5 days, L. monocytogenes was identified in the blood culture. CSF was clear and PCR testing of the CSF did not reveal any pathologies. After improvement, on the 13th day of hospitalisation the patient developed haemoptysis and tachypnoea, and therefore had to be intubated. His haemoglobin level dropped to 9.5 mg/dl. An urgent CT pulmonary angiography (CTPA) was performed. It showed bilateral ground glass opacities with a crazy paving pattern and bilateral pleural effusion. Pulmonary embolism had been excluded. Echocardiography revealed large vegetation on the mitral valve, leading to worsening of the patient’s state. Vasopressor support was needed. Six days after the patient’s condition worsened, a CT angiography of the thorax revealed improving diffuse ground glass opacities. An MRI of the brain was performed, which revealed the enhancement along the right central sulcus (Rolando’s sulcus) surrounded by parenchymal oedema, which indicated cerebritis, associated with microhaemorrhages. The patient’s condition progressively deteriorated and, unfortunately, led to his death after 3 weeks of hospitalisation.
Feraco et al. [40] present a case report of a 72-year-old man, who was admitted to the hospital with high fever of 41.4°C, accompanied by vomiting, headache, and persistent hiccups. The patient was showing signs of lower limb asthenia, which led to difficulties in walking. What is interesting, none of the meningeal signs were detected. However, the worsening of his mental status led to the patient’s intubation. CSF had an infection-like appearance, and PCR of the CSF revealed the presence of L. monocytogenes. Despite the implementation of pathogen-appropriate antibiotic treatment, the patient’s condition worsened and upper-limb asthenia developed. An MRI of the brain revealed small oval lesions on the pons, bulb, and left middle cerebral peduncle. Among these smaller lesions, which exhibited typical ring-enhancement after the administration of intravenous contrast, a larger lesion was also detected. Within this larger lesion, T2-weighted imaging showed a blooming artifact with no restriction on DWI. This indicates a presence of a haemorrhage at acute-late stage, accompanied by perilesional oedema. Although the authors mention hemosiderin as the most popular cause of blooming artifacts of T2-weighted imaging, they also suggest that the free radicals from phagocytosis should be considered as another potential cause.
The team led by Acewicz et al. [41] described a case of a 52-year-old woman presenting with fever, diplopia, and left-sided weakness that started 3 hours before admission to the hospital. The woman had a medical history of schizophrenia and Crohn’s disease and was treated with methylprednisolone at a dose of 16 mg/day, along with other drugs for this autoimmune condition. There were some abnormalities in neurological examination, such as mild dysarthria, left-sided hemiparesis, central facial nerve palsy, along with right abducens nerve palsy. What is important, there were no signs of meningeal irritation. CT was performed – there were no pathologies. Diffusion-weighted MRI revealed restricted diffusion, along with decreased signal in ADC and increased signal on FLAIR. Flow changes encompassed structures such as right midbrain, upper part of dorsal pons, and right internal capsule. There were no abnormalities in brain arteries or chest radiography. Blood results revealed a white blood cell count of 13.49 mg/l with a neutrophil level of 78.3%. CRP was slightly increased at 15 md/l. Urine and blood cultures were taken. Given the patient’s history of Crohn’s disease and a single episode of bleeding, an intra-abdominal infection was suspected, leading to the initiation of treatment with ceftriaxone with metronidazole. After a few days, the patient’s general state worsened. The fever was still present (39.5oC), and a left oculomotor nerve palsy and right-sided hemiparesis emerged. Later there was deterioration of the patient’s consciousness level. DWI was repeated, demonstrating expansion of the previous midbrain lesion, and the appearance of new lesions. They were localised in the area of the right lateral ventricle and in the left globus pallidus. Due to the negative results of the blood culture, it was retaken. CSF parameters indicated an inflammation process. At that moment, there was suspicion of L. monocytogenes infection, and treatment with ampicillin was initiated. Unfortunately, the patient’s condition worsened the next day. The fever was high (41oC), and she was only able to respond to pain stimuli. She developed hypotension and hypoventilation. CT revealed hypodense lesions, encompassing both cerebral peduncle, both thalami, both internal capsule, and left globus pallidus. A few hours later, the patient passed away. Listeria monocytogenes grew from blood culture (but not from CSF culture).
Khan et al. [42] described the case of a 52-year-old woman who was treated with 400 mg/day of levodopacarbidopa for extrapyramidal syndrome and 50 mg/day of losartan for hypertension for the past few years. Upon admission, she presented with a one-week history of headaches, with no response on any treatment, and a progressive reduction of vision in both eyes. At the time of admission, the woman experienced an episode of tonic-clonic movements affecting each limb. Despite impaired vision, her ability to perceive light remained intact. Other cranial nerves did not reveal any abnormalities. She experienced cogwheel rigidity, more pronounced on the left side, and intentional tremors, which were more evident in the upper limb, especially on the left side. Her tandem walk was compromised. Laboratory results revealed elevated white cell count and elevated CRP. MRI was performed. It revealed multiple ring – enhancement lesions, localised in the right frontal, left parietal, and both occipital lobes. Intravenous ceftriaxone was given. In the meantime, CSF and blood cultures were ordered. After one week of treatment with ceftriaxone, MRI was repeated. Unfortunately, it revealed that the primary brain abscess had increased in size. Blood cultures revealed the presence of Gram-positive bacilli, which were sensitive to cotrimoxazole and resistant to cephalosporins. This led to a suspicion of L. monocytogenes, which was later confirmed. After oral cotrimoxazole treatment, the MRI revealed significant reduction of the brain abscess.
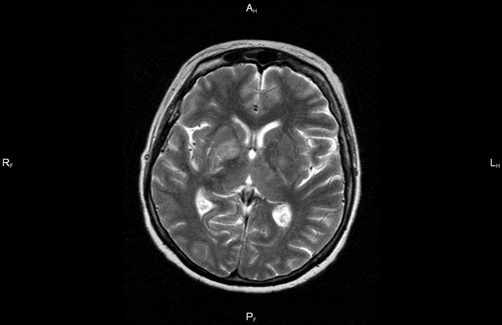
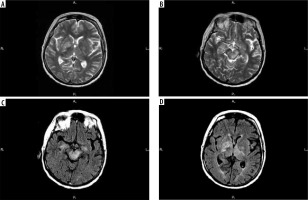
Czupryna et al. [43] presented a case of a 61-year-old woman with a history of headaches, vertigo, nausea, and drowsiness that started 2 weeks before admission to the hospital ward. Before admission to the infectious disease hospital, the patient had undergone 2 CT examinations – no pathologies were seen. Physical examination revealed fever, dehydration, and neck stiffness. Besides hyponatraemia, laboratory results were normal. CSF examination indicated a state of inflammation. A key clue was the fact that the woman lived in a tick-endemic area, which suggested a diagnosis of tick-borne encephalitis (TBE) or neuroborreliosis. Additionally, her family mentioned a recent tick bite. Therefore, ceftriaxone was given. However, based on serological results, the suspicions turned out to be wrong. The woman’s state worsened day by day – on the fifth day of hospitalisation she was unconscious, not responding to stimuli, with a weak response to light. MRI was performed. In T2 images, it revealed irregular, hyperintense lesions in the pallidum, internal capsules, cerebral pedunculi, and right cerebellum hemisphere. On the sixth day of hospitalisation, ampicillin-resistant L. monocytogenes was identified from blood culture (Figure 1).
Figure 1
T2-weighted images (A-B) and FLAIR (C-D) in the case of Czupryna et al. showing bilateral, asymmetrical, and irregular T2 and FLAIR hyperintense lesions especially in the brainstem, cerebral peduncles, basal ganglia, and left thalamus
Pereira et al. [44] presented a case report of a 29-year-old female who had erythematous lesions in the lower limbs and systemic arterial hypertension 7 months before admission. The patient did not have earlier pathological history. Anti–hypertensive therapy was started. After that she was admitted to the emergency department due to atypical chest pain; further investigation disclosed cavitary effusions, raising suspicion of a systemic disease. The hypothesis of active SLE was suggested due to serositis along with cutaneous and renal involvement. Moreover, the positive result of anti-nucleus factor at the level of 1 : 640 indicated a homogeneous nuclear pattern. Intravenous pulse therapy was started with methylprednisolone for 3 days, followed by prednisone and mycophenolate mofetil. After 3 months, she returned to the clinic complaining of diarrhoea and asthenia, additionally with oedema of the lower limbs and perineal lesions reminiscent of genital herpes. Laboratory tests revealed increased, inter alia, serum creatinine, proteinuria of 5 g, and dysmorphic haematuria, without evidence of haemolysis. Considering the activity score of the SLEDAI-based disease (Systemic Lupus Erythematosus Disease Activity Index), the patient had a score of 20. Results above 8 indicate active disease. She was treated with acyclovir and received a red blood cell transfusion. Renal biopsy revealed active/chronic class IV – global lupus nephritis. Due to an increase in serum creatinine, a new course of methylprednisolone was administered for 3 days. However, after 3 days of pulse therapy, the patient had altered mental status, developed a headache, and started to vomit. CT scan with contrast exposed a hypoattenuation area measuring about 7.0 × 5.0 cm in the left frontal white matter that had the mass effect on surrounding structures. A lumbar puncture was performed. L. monocytogenes was cultured. An empirical treatment was initiated with ceftriaxone, vancomycin, and acyclovir. After differentiation in culture, the intravenous ampicillin was started. The patient’s neurological status was aggravated, and she was transferred to the intensive care unit. The patient remained in a comatose state for 60 days. An MRI of the brain was conducted. In a T2 sequence there was an abnormality in the left frontal lobe, which was affecting mostly the middle and upper frontal gyrus. It had irregular contours that were bordered by deposits of hemosiderin, with an intense restriction on inside diffusion corresponding with an abscess. Considering the neurological condition of the patient, palliative care was started. After infection of the bloodstream, the patient died.
Tiri et al. [45] presented 2 case reports. The first one was a 62-year-old immunocompetent man with no significant previous medical history. He was hospitalised due to interscapular pain, high-grade fever, and intractable hiccups. Chest radiograph, abdomen ultrasound, and echocardiography were performed, and no abnormalities were found. However, the CT scan of the brain disclosed a diffuse abnormal pattern (presence of nonspecific inflammatory material). In the trigonum of the lateral ventricle there were hypodense lesions in an underlying condition of demyelination and gliosis, suspicious for chronic ischaemic vascular disease. Vancomycin and ceftriaxone were administered. After a few days, the patient did not have a fever or stiffness of the neck. Moreover, he had a headache and persistent hiccups. MRI of the brain was conducted. It exposed enhancement of white spot lesions on the pons, midbrain, thalamus, cerebral peduncle, and both trigeminal nerves. He was transferred to the neurological department. A lumbar puncture was performed. Therapy with ceftriaxone and vancomycin was stopped due to suspicion of viral aetiology. Acyclovir and steroids were administered. After 72 hours, he became aphasic and hyperpyretic – on the Glasgow Coma Score (GCS) he scored 9. CT of the brain was conducted. It showed the involvement of the subcortical left temporoparietal lobe. The patient was then transferred to the Infectious Disease Department. Blood cultures were drawn. Another lumbar puncture was performed. Therapy with ampicillin 3 g/6 h + gentamicin 80 mg/8 h was administered. After 72 hours, symptoms disappeared, resulting in complete recovery (GCS15). Listeria monocytogenes was isolated from the patient’s blood. After 8 weeks of antibiotic therapy an MRI was repeated due to fluent aphasia. An MRI scan of the brain revealed ring-enhancement in the left front-temporoparietal lobe corresponding with a brain abscess with perilesional oedema. After treatment, the patient’s condition improved, with a complete recovery of linguistic abilities.
The second presented case describes a 72-year-old man with a history of bullous pemphigoid. He was treated with a monoclonal antibody. His admission was due to a balance disorder. A neurological examination showed a left hemiplegia with no sensory impairment. CT scan of the brain exposed a ring-enhancing cortical-subcortical lesion on the right frontal-parietal hemisphere. Gadolinium MRI of the brain was conducted. MRI revealed a caudal extension of the lesion with irregular enhancement and a necrotic region. Blood cultures were drawn. A few days later, in the blood cultures L. monocytogenes was grown. Intravenous therapy with ampicillin, vancomycin, and gentamicin was administered. Due to moderate mass effect, steroid therapy was also included. However, after 20 days, the patient had hemiplegia, visual hallucinations, and frontal symptoms with disinhibition. An MRI scan of the brain exposed a relevant increase in lesion size. Moreover, there were new lesions located on the right temporal lobe and splenium of corpus callosum with a significant mass effect on the right lateral ventricle. Trimethoprim/sulfamethoxazole 160/800 mg/8 h was administered. A surgical biopsy of the lesion was performed. Listeria monocytogenes was identified with usage of PCR. After 5 weeks, imaging diagnosis was performed – it showed a reduction in the enhancement and size of the lesions. Gentamicin, ampicillin, and vancomycin therapy was discontinued. However, trimethoprim/sulfamethoxazole therapy was continued. After 8 weeks an MRI scan of the brain was conducted. It revealed improvement and a decrease in the amount of vasogenic oedema. A year after the listeria brain abscess diagnosis, the patient did not show any significant neurologic deficits and was able to perform all activities of daily living [45].
In a case report by Paranjape [46] a 46-year-old male had severe headache, lower and right-sided upper weakness, dysphagia, unsteady gait, blurred vision, and subjective fevers. Fever and headache had started one week before arriving in the emergency room, where he developed a respiratory failure and was intubated. In his past medical history was dermatomyositis for which he weekly received methotrexate. His last dose of the medicine before admission was 3 weeks prior. On the first day of hospitalisation, an MRI of the brain revealed ring enhancing lesions in the lateral medulla. Lumbar puncture was performed. From CFS cultures L. monocytogenes was grown. Ampicillin and gentamicin were initiated. Despite the treatment, the condition of the patients started to worsen. MRI, which was performed during the fourth day of admission, revealed multiple ring enhancing lesions in the brain stem. On the eighth day of admission, the patient became unresponsive. The CT scan of the brain showed a vast haemorrhage of the brainstem with resultant hydrocephalus. The patient had ventriculostomy; however, his condition did not improve. On the 10th day of the admission, the patient died.
In a case report by Trachuk et al. [47] a 56-year-old woman had been suffering from right arm and leg weakness, which developed into right hemiparesis. In her medical history: she was diagnosed with autoimmune hepatitis 3 months before admission, for which she was taking prednisone 20 mg daily and azathioprine 100 mg daily. Before admission, the patient had chills, rhinorrhoea, as well as frontal headache. She did not complain of abdominal pain, nausea, emesis, rash, diarrhoea, blurry vision, fever, or night sweats. She also did not travel recently, did not eat unpasteurised cheese, or change her diet. A CT scan of the head without contrast disclosed a left frontal mass with vasogenic oedema. The MRI of the brain with and without contrast was performed. It showed 2 lesions that were peripherally enhanced located in the left hemisphere. They measured 2.1 × 1.2 cm in size and were surrounded by hyperintense in the T2-sequence area of white matter oedema. Moreover, they had a local mass effect. On the third day of hospitalisation, the patient had chest X-ray that did not show abnormalities. Empiric antimicrobial therapy was initiated with ceftriaxone, metronidazole, and vancomycin due to suspicion of brain abscess. A lumbar puncture was performed. From blood cultures, over the next 2 days, L. monocytogenes was grown. On the fifth day, the patient had an MRI-guided stereotactic aspiration of the left frontoparietal brain abscess. Drainage was done. From the bacterial culture L. monocytogenes was also grown.
In a case report by Vettas et al. [48] a 70-year-old male had a fever up to 39oC for 3 days. From other symptoms, he had disorientation and confusion for the last 24 hours before admission to the hospital. In his past medical history: the patient had cholecystectomy, benign prostatic hyperplasia, and beta thalassaemia trait. Eight months before admission, he was on a missionary trip to Madagascar. Over the last 8 weeks the patient had been in different hospitals due to fever estimating from 38 to 39oC. It was accompanied not only by temporal headaches, but also transient ischaemic attacks manifesting as dysarthria, mouth dropping, hemiparesis, and numbness of the right upper limb that passed within hours. The patient had magnetic resonance angiography that showed potential inflammatory stenosis of left common carotid artery and right vertebral artery. He was diagnosed with temporal arteritis. However, biopsy of the temporal artery was negative, and, moreover, a CT scan of the brain did not confirm any anomalies. Intravenous steroids were initiated. CT scans of the brain did not expose any anomalies. However, 2 weeks after discharge, he came to the ward. He was treated with prednisolone 60 mg daily, clopidogrel 75 mg daily, folic acid 5 mg/week, and methotrexate 20 mg/week. CT scan of the brain was performed. In the frontal lobe there was a mild asymmetry of the subarachnoid spaces. Due to treatment with clopidogrel, the lumbar puncture could not be performed – methotrexate and clopidogrel were stopped. A brain MRI with gadolinium was conducted. It exposed 3 lesions, which had a maximum diameter of 1.3 cm, near the corpus callosum. Two of them were located on the right of the midline. One was located on the left side with perifocal cerebral oedema, constriction in the DWI sequence, and mild ring-shaped enhancement in the right posterior lesion. Two smaller lesions were also reported. They had peripheral enhancement close to the frontal horn and mild perifocal oedema. There was a suspicion of aspergillus infection or possible abscess. Lumbar puncture was performed. An infection due to L. monocytogenes was confirmed. The patient was treated with ampicillin for 6 weeks. Another MRI scan of the brain showed improvement. The patient was discharged on the 50th day of hospitalisation. He was prescribed prednisolone 15 mg q.d. and levetiracetam 1.5 g/d.
In a case report by Dragomir et al. [49] a 64-year-old male was hospitalised because of 2 episodes of the sharp right parietal headache, which each lasted under one minute, followed by temporary aphasia. The patient had hypertension, hyperlipidaemia, and stage III chronic kidney disease. Summing this up with the patient’s age, these were risk factors of stroke. Moreover, he had lupus nephritis treated with prednisone and mycophenolate. Two weeks prior to admission, the patient was on Caribbean vacation, when he had self-limited traveller’s diarrhoea. A coronal CT scan of the head with and without contrast was performed. It exposed a lesion, measuring 1.7 × 1.3 cm with surrounding oedema, in the left intra-axial frontal lobe. MRI of the brain with contrast was also conducted. It disclosed a mass that was peripherally enhancing in the left frontal intra-axial lobe. It was surrounded by vasogenic oedema. There was minimal mass effect and no midline shift. The lesion was suspected of being an abscess or neoplasm. In the right frontal lobe, there was a punctiform form of diffusion restriction that was associated with an acute embolic infarct. CT angiography did not show any abnormalities. From blood cultures L. monocytogenes was grown. The patient had a left frontal craniotomy with partial resection of the lesion. The patient was discharged home on dexamethasone, mycophenolate, trimethoprim-sulfa, levetiracetam, and ampicillin and was directed to follow up with neurology, infectious disease clinics, and neurosurgery.
Wang et al. [50] described a case report of a previously healthy adult patient who had a history of headache and fever for 6 days prior to hospitalisation. From other symptoms, he had emesis for one day and altered mental status for 4 hours. Neurological examination exposed bilateral, equally large pupils that were insensitive to light. Moreover, the Kernig’s sign was positive, and the patient had stiffness of the neck (3 horizontal fingers at the submental). CT of the head was performed. It disclosed swelling of the brain. Due to a CT scan of the chest, there was a suspicion of a pulmonary infection. Vancomycin, ceftriaxone, mannitol, and glycerol fructose were initiated. On the fifth day, another CT of the brain scan was performed; however, it did not indicate any important change. However, CT scan of the chest exposed infection of the right lower lung. On the seventh day of hospitalisation, lumbar puncture was conducted. Bacterial cultures were positive for L. monocytogenes. However, blood culture was negative. In addition, the sputum culture exposed hydrocarbon-resistant Acinetobacter baumannii. On the 14th day, the patient’s state worsened – there was drowsiness, limited left and right abduction, and slow light response. The CT scan of the head disclosed a new lesion in the right frontal lobe; it was oval and slightly low-density. On the 15th day, an MRI of the brain was conducted. Abnormal signals were found in lateral ventricle, pons, the right basal ganglia region, right bride-arm, left ventricle trigonometry, bilateral frontal lobes, and bilateral paraoccipital–temporal sulcus. Antibiotics included teicoplanin, cefoperazone, sulbactam sodium, and penicillin. On the 24th day of admission, the patient had, inter alia, electrolyte disorder and liver dysfunction. On the 27th day of the hospitalisation, the patient had lumbar puncture and an MRI scan of the head. MRI disclosed abnormal signals in thalamus, pons, medulla oblongata, left temporal horn, which became wider, and in the right basal ganglia region, lateral ventricle, left craniocerebral foot, and bilateral frontal lobe.
Typical topographical mapping of pathological MRI and CT findings in patients with confirmed neurolisteriosis: see Table 1.
Table 1
Typical topographical mapping of pathological MRI and CT findings in patients with confirmed neurolisteriosis
Conclusions
Despite the presence of many diagnostic methods for detecting invasion of the central nervous system by L. monocytogenes, radiological imaging techniques, including CT or MRI, play a significant role in establishing an accurate diagnosis in a relatively short time, which is crucial. Unfortunately, pathologies of the CNS are often non–specific and can be mistaken for many other conditions. However, in some cases, the unexpected pathologies observed in imaging diagnostics lead us to modification of the current treatment, and, in extreme cases, the intervention of neurosurgeons. Patients presenting neurological symptoms and poor test results that show no improvement should undergo diagnostic imaging if it is available.