Introduction
Intramedullary tumours (IMTs) of the spinal canal are relatively uncommon neoplasms, which constitute only about 2-5% of all spinal canal tumours [1].
The vast majority of IMTs consist of two neoplasms: ependymoma (the most common IMT in adults) and astrocytoma (the most common IMT in children). Ependymomas and astrocytomas comprise about 80% of all IMTs [1,2]. The third commonest IMT is haemangioblastoma. The other types of neoplasms in the spinal cord are relatively rare.
In the past, IMTs were considered inoperable due to the risk of severe damage of the spinal cord during a surgical procedure. Nowadays, due to the progress in neurosurgical techniques (including neuro-navigation and intra-operative neurophysiological monitoring of spinal cord tracts) IMTs are commonly operated on. Therefore an accurate diagnosis has become very important.
Imaging is the crucial diagnostic method in IMTs. The imaging method of choice is magnetic resonance imaging (MRI), while other imaging modalities such as computed tomography (CT), vascular studies (Doppler sonography, CT angiography, MR angiography, intraarterial angiography), and positron emission tomography (PET/CT, PET/MR) are supplementary methods. CT myelography used to be performed in patients with contraindications to MR, which are nowadays very limited [3].
Magnetic resonance imaging in intramedullary tumours – technical considerations
MRI of the spinal cord is generally challenging due to the small size of the spinal cord and many artefacts, e.g. from the cerebro-spinal fluid, aorta and other vessels’ flow, as well from breathing or swallowing, chemical shift artefacts or truncation artefacts.
The basic MRI protocol in IMTs includes:
spin-echo (turbo spin-echo, fast spin-echo) T1-weighted and T2-weighted sagittal images;
spin echo T2-weighted axial images;
spin-echo (turbo spin-echo, fast spin-echo) T1-weighted fat suppression contrast enhanced, sagittal, axial and coronal images.
It has to be stressed that contrast enhanced images in all three main planes are mandatory in patients with IMTs [4,5].
This basic protocol might be expanded by fat suppression T2-weighted sagittal images and spin-echo (turbo spin-echo, fast spin-echo) T1-weighted non-enhanced axial and/coronal images.
Supplementary MRI sequences include susceptibility weighted imaging (SWI) to detect haemorrhagic foci (e.g. in ependymomas) and MR angiography to differentiate IMT from vascular malformations.
Advanced MRI sequences are not used commonly in IMTs, because of the technical difficulties and consumption of time. Among them the most promising is use of diffusion tensor imaging (DTI), which could help in differentiation between expansile and infiltrating IMTs [6,7]. Other advanced techniques, such as diffusion weighted imaging (DWI), MR perfusion (PWI), MR spectroscopy (MRS) and functional MRI (fMRI), have provided interesting research data regarding IMTs, but due to technical problems are rarely used in clinical practice [5,8].
Imaging of particular IMTs
It has to be emphasized that the first important step in assessing IMTs is to differentiate intramedullary location of the spinal canal tumour from the intradural extramedullary and extradural compartments [1,4]. This allows differentiation from typical extramedullary tumours, such as meningioma or neurofibroma. Establishing the location of the tumour in one of the three compartments is usually easy, provided that all three basic planes have been acquired. After confirming the intramedullary location of the tumour, the next step is an attempt to diagnose its histopathological type, which is possible on the basis of imaging features, as discussed below.
Ependymoma
Ependymomas are the most common IMTs in adults [1]; they are rare in children.
The typical MRI features of ependymomas are (Figures 1-4) [1,9,10]:
Figure 1
Ependymoma. Male, 45 years. MR sagittal T2-weighted (A), fat suppression sagittal (B), coronal (C) and axial (D) images. Note the typical peripheral rim of hemosiderin (arrows)

Figure 2
Ependymoma. Female, 45 years with progressive paraparesis. MR sagittal T2-weighted (A), T1-weighted post-gadolinium sagittal (B), coronal (C) and axial (D) images. Note the central location of the tumour in the spinal cord (arrows)

Figure 3
Ependymoma, WHO, grade 2. Female, 41 years. MR sagittal T2-weighted (A), T1-weighted (B) and T1-weighted post-gadolinium (C) images. Note the syringomyelic cavity above the tumour (arrows)

Figure 4
Anaplastic ependymoma, WHO, grade 3. MR sagittal T2-weighted (A), and T1-weighted (B) images. Tumour is located in the conus medullaris (arrows). C) Intraoperative photo of the tumour (courtesy of Mr. Marcel Ivanov, MD, Consultant Spinal Neurosurgeon, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK)

central location in the spinal cord (opposite to astrocytomas), most commonly (about 50%) in the cervical segment of the spinal cord;
well-defined borders (opposite to astrocytomas), may enlarge spinal cord’s contour;
low to intermediate signal in T1-weighted images, intermediate to high signal in T2-weighted images;
may contain cystic components (widening of the spinal cord central canal);
may contain haemorrhagic components (peripheral rim of hemosiderin), which are considered a pathognomonic finding, but are present in a minority of cases;
high contrast enhancement (about 90% of patients).
Ependymoma may be associated with neurofibromatosis type 2 (NF2); in these cases it is often accompanied by multiple spinal schwannomasas as well as spinal meningiomas as well as spinal meningiomas (Figure 5). Patients with IMTs who have intraspinal schwannomas and present typical clinical signs of intracranial NF2 such as hearing loss, tinnitus or balance problems, should undergo brain MRI to look for bilateral vestibular schwannomas and other intracranial features of NF2 [11].
Figure 5
Neurofibromatosis type 2. MR sagittal T2-weighted (A, B), and T1-weighted post-gadolinium (C, D) images. Intramedullary tumour (ependymoma) in the cervical spinal cord (arrows). Multiple schwannomas/meningiomas in the intradural extramedullary space (arrowheads)

A specific type of ependymoma is myxopapillary ependymoma, which originates from ependyma in the filum terminale and therefore is located in the conus medullaris or cauda equina of the spinal cord. Myxopapillary ependymomas usually demonstrate intense contrast enhancement and may be heterogeneous due to haemorrhage and cyst formation (Figure 6) [12].
Astrocytoma
Astrocytoma is the second overall most common IMT (about 30% [4]), but the most common in children (40-60%) [4,13]. The majority of astrocytomas are low grade tumours. The most common histopathological types are pilocytic astrocytoma and diffuse astrocytoma [13].
The typical MRI features of astrocytomas are (Figures 7-10) [1,9,10]:
Figure 7
Astrocytoma. Male, 6 years with progressive paraparesis. MR sagittal T2-weighted (A), T1-weighted (B), post-gadolinium T1-weighted sagittal (C) and coronal (D) images. Note the eccentric location of the tumour, marked widening of the spinal cord, irregular contrast enhancement as well as multiple intratumoural cysts (arrow on A)

Figure 8
Pilocytic astrocytoma, WHO, grade 1 in the thoracic spinal cord. MR axial T2-weighted (A), axial T1-weighted post-gadolinium (B), sagittal T1-weighted (C), sagittal T1-weighted post-gadolinium (D) images (arrows). (E) Intraoperative photo of the tumour (courtesy of Mr. Marcel Ivanov, MD, Consultant Spinal Neurosurgeon, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK)
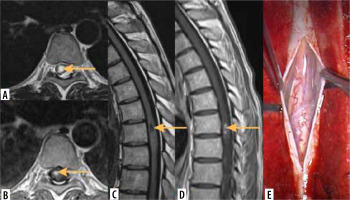
Figure 9
Astrocytoma in upper cervical spinal cord. Male, 20 years. MR sagittal T2-weighted (A, B), coronal T2-weighted (C) and post-gadolinium T1-weighted sagittal (D) images. Note the eccentrical location of the tumour, widening of the spinal cord and small intratumoural cysts (arrows)

Figure 10
Astrocytoma in thoracic spinal cord. MR sagittal T2-weighted (A), coronal (B) and sagittal (C) diffusion tensor tractography (DTT) images. Note the smooth margins of the tumour in DTT images (arrows), which suggest its expansion without infiltration of the adjacent spinal cord tissue

ill-defined, expanding lesion, typically located eccentrically in the spinal cord;
low to intermediate signal on T1-weighted images; intermediate to high signal on T2-weighted images;
involves several segments of the spinal cord (in extreme cases the whole spinal cord – so-called whole cord glioma);
most commonly located in the cervical or cervicothoracic region of the spinal cord;
may be surrounded by oedema;
in about 50% of cases may contain cysts (syringo/hydromyelia);
no haemorrhage (opposite to ependymomas);
irregular enhancement after gadolinium injection.
Astrocytoma may be associated with neurofibromatosis type 1 (NF1) [11]. Therefore patients with IMTs who present typical clinical signs of NF1, such as cutaneous neurofibromas, café-au-lait spots, axillary freckling or Lisch nodules, should undergo brain MRI to look for optic gliomas and other brain features of NF1.
Haemangioblastoma
Haemangioblastoma is the third most common IMT in adults.
The typical MRI features of haemangioblastomas are (Figure 11) [14]:
Figure 11
Haemangioblastoma. MR sagittal T2-weighted (A), T1-weighted (B) and T1-weighted post-gadolinium (C), axial T2-weighted (D) and T1-weighted post-gadolinium (E) images. Note large cystic component (arrows) and small enhancing marginal nodule (arrowhead)

superficial location in the spinal cord (can also be seen in the extramedullary space, but the majority of them are intramedullary);
high vascularization, with many hypointense flow void foci, compatible with vessels;
otherwise intermediate signal on T1-weighted images; intermediate to high signal on T2-weighted images;
marginal nodules which demonstrate strong enhancement.
Multiple haemangioblastomas are commonly seen in von Hippel-Lindau (vHL) syndrome, a genetic autosomally dominant disease, predisposing to multiple central nervous system tumours. The typical locations of tumours in vHL are the cerebellum and spinal cord. Detection of multiple cystic tumours with enhancing marginal nodules are almost pathognomonic to vHL [15]. In cases of solitary tumours with atypical appearance, MR angiography, CT angiography or conventional spinal angiography should be considered to differentiate haemangioblastoma from vascular malformation.
Other, less common intramedullary tumours
Paraganglioma is typically located in the lumbar segment of the spinal canal: in the conus medullaris of the spinal cord or in the cauda equina. The common features of spinal paragangliomas are, like in other locations of this tumour, multiple flow voids, compatible with abnormal vessels, which could be seen both in the tumour itself and its vicinity (Figure 12) [16].
Figure 12
Paraganglioma of filum terminale. MR sagittal T2-weighted images (A, B). There are multiple linear signal void foci compatible with abnormal vessels both within and above the tumour (arrowheads)

Dermoid cyst is a non-neoplastic tumour, which is more common in the intracranial space. In the spinal canal it is often located, like paraganglioma, in the conus medullaris or cauda equina. Dermoid cysts typically include a fatty component, and therefore they may be entirely or partially hyperintense on T1-weighted images and hypointense in fat saturation images (Figure 13) [17].
Intramedullary lipomas not associated with spinal dysraphism constitute about 1% of IMTs and present on MRI as lesions with a homogeneous signal with a typical fat pattern, including a chemical shift artefact [18].
Figure 13
Dermoid cyst of conus medullaris. MR sagittal T2-weighted (A) and T1-weighted (non-enhanced) (B) images. Note high signal focus on T1-weighted image, compatible with fatty component (arrow on B)

Epidermoid cysts of the spinal canal comprise 0.5-1% of all spinal tumours. They demonstrate a cerebrospinal fluid signal on T1 and T2-weighted images, but DWI and ADC reveal restriction of the diffusion, which is helpful in differentiation from arachnoid cysts [19].
Other spinal cord tumours are extremely uncommon and include ganglioglioma, mixed glioma, glioblastoma multiforme, germinoma, lymphoma and metastases [1]. The latter may originate from lung cancer, breast cancer, melanoma and lymphoma [20].
Differentiation of intramedullary tumours
Demyelinating diseases of the spinal cord such as multiple sclerosis or neuromyelitis optica spectrum disorder (NMOSD) could sometimes mimic IMTs. However, demyelinating foci are usually multiple, do not produce a mass effect and do not enhance (except for early lesions, which may demonstrate ring enhancement) (Figure 14). In doubtful cases brain and orbital MRI as well as clinical, electrophysiological and CSF findings should provide a proper diagnosis [21].
Figure 14
Differentiation: multiple sclerosis. MR sagittal (A) and coronal (B) T2-weighted images. Multiple hyperintense foci in the spinal cord (arrows)

Syringomyelia should always be taken into account in differentiation of IMTs, because syringomyelic cavities accompany many tumours of the spinal cord (e.g. ependymoma, astrocytoma). In fact, CSF-filled cavities associated with IMTs are caused by widening of the spinal cord’s central canal above and/or below the tumour due to its occlusion by IMT. Therefore it could be actually called hydromyelia, but the terms syringomyelia and syringohydromyelia are also correct [22].
Syringomyelia can be associated with many entities apart from IMTs, e.g. with Chiari 1 malformation, spinal dysraphism, previous trauma or infection; also, some cases of spinal cord syringomyelia are idiopathic [17]. The most important differentiating feature is enhancement of the majority of IMTs, while in other causes of syringomyelia the enhancement is not present. Therefore if IMT is suspected, post-contrast MRI is mandatory (Figure 15) [10].
Figure 15
Differentiation: syringomyelia. MR sagittal T2-weighted (A), T1-weighted (B) and T1-weighted post-gadolinium sagittal (C) and axial (D) images. Note syringomyelic cavity without contrast enhancement (arrows on C and D)

Inflammatory diseases of the spinal cord such as transverse myelitis can also mimic IMT, because they commonly demonstrate diffuse hyperintensity on T2-weighted images and enlargement of the spinal cord, as well as contrast enhancement in some cases. The most helpful features in differentiation are the clinical course (more rapid in inflammatory diseases) and laboratory findings [17,23].
On the other hand, spinal cord infarction is usually easily differentiated from IMT on the basis of clinical features (rapid severe paraplegia) and MRI pattern with long segment hyperintensity located typically in the anterior part of the spinal cord [24].
Vascular malformations of the spinal canal should also be considered in the differentiation of IMTs. The most common spinal vascular malformation is spinal dural arteriovenous fistula (SDAVF). SDAVF usually involves a long segment of the spinal cord. It leads to reduced perfusion and ischaemia of the spinal cord due to venous hypertension. This in turn causes progressive spastic paraparesis as well as thickening and an increased MRI T2 signal of the spinal cord, which could mimic IMT. The most important differentiating MRI finding of SDAVF is the presence of multiple flow voids which are consistent with abnormal vessels. They are typically located on the posterior surface of the spinal cord. Therefore in each case of diffuse hyperintensity and thickening of the spinal cord, this area should be carefully checked. In doubtful cases the imaging could be supplemented by MRA, CTA or spinal angiography (Figure 16) [25].
Figure 16
Differentiation: spinal dural arterio-venous fistula (SDAVF). MR axial (A) and sagittal (B) T2-weighted images. Diffuse enlargement and hyperintensity of the spinal cord with multiple tiny linear signal void foci on the posterior surface of the spinal cord (arrows), compatible with abnormal vessels. (C) Spinal angiography confirms diagnosis of SDAVF

The less common types of spinal vascular malformations are arteriovenous malformation (AVM) and cavernoma. AVMs are characterized by multiple abnormal tortuous vessels presenting on MRI as flow voids, which commonly are located both in the spinal cord and in the extramedullary compartment of the spinal canal. The diagnosis is usually obvious, but some AVMs could mimic haemangioblastoma; thus again, magnetic resonance angiography (MRA), CTA or spinal angiography should be considered to establish the final diagnosis [26].
Cavernomas of the spinal cord are much less common than in the brain. On MRI cavernomas present as small foci of the abnormal signal of the blood products caused by previous haemorrhages, e.g. hyperintense T1-weighed foci compatible with methemoglobin and/or hypointense T2-weighed foci consistent with hemosiderin (salt and pepper appearance) [27].
Summary
IMTs are relatively rare, with astrocytomas and ependymomas constituting the majority of them. The imaging method of choice is MRI, which enables precise assessment and differentiation of IMTs. Advanced MR techniques, especially diffusion tensor imaging (DTI), might potentially provide additional diagnostic information and help in deciding which patients may be suitable for surgery.




