Introduction
Coronary artery disease (CAD) is the most prevalent type of cardiovascular disease and one of the most common causes of death worldwide. Early diagnosis makes early intervention possible for the modifiable risk factors of the disease [1]. Coronary artery calcification (CAC) is a marker of intimal atherosclerosis. The amount of calcification on the vascular wall indicates the prevalence and chronicity of the disease [2]. Most previous studies have reported that in addition to the information obtained, in reference to the standard risk factors, the total amount of coronary artery calcium can predict future CAD events [3,4]. Coronary artery calcification has been found to be the most robust risk prediction tool for CAD events, and it serves as the basis for new concepts, such as coronary and cardiovascular age, to improve risk communication between health care providers and patients [5]. Patients’ awareness of their own coronary calcium burden may also potentially play a role in convincing people to make correct lifestyle choices [6] and to improve compliance with disease-modifying medications [7]. As a result, this may trigger an assessment of modifiable cardiovascular risk factors and guide the appropriate use of preventative medications [7].
Currently, standard noncontrast chest computed tomography (CT) is widely used for the diagnosis of cancer and pneumonia. Calcium in the coronary arteries is easily identified through this imaging method and is defined as incidental CAC. The most common method employed for CAC scoring in clinical practice is the Agatston method [8]. Although Agatston is the reference method, it is not routinely used for incidental CAC scoring. It requires customized software as well as ECG-gated scanning, and it is only applied for specific indications; it is not used routinely. The Weston score (WS), a visual approach, is used for the evaluation of CAC detected on chest CT. The WS is an easy and fast calculation method that does not require any specific software. Some previous studies have reported that the WS and Agatston score are compatible [9,10].
Each year, millions of chest CTs are performed for various reasons. These images serve as a significant means for the early diagnosis of CAD and obstructive CAD (OCAD). The purpose of the present study was to demonstrate that CAC should be routinely reported during the evaluation of thoracic CT examinations. Routine reporting of CAC will contribute to the early diagnosis of CAD.
Material and methods
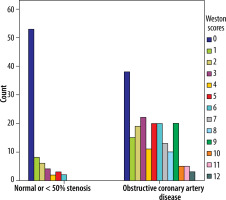
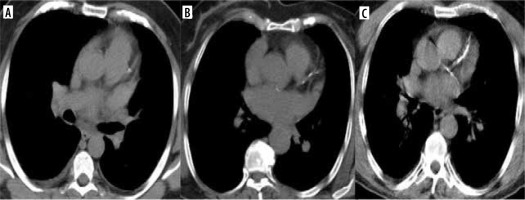
Patients aged > 40 years who underwent CAG between 1 January 31 and December 2021 at Malatya Training and Research Hospital (n = 2796) were retrospectively included using the hospital’s information system. Out of these patients, those who underwent noncontrast chest CT for any reasons within one month before CAG were identified using the hospital’s radiology information system. The number of patients who underwent CT within this one-month period was 383. A total of 24 patients who previously underwent bypass surgery, 75 patients with a stent inserted, and 5 patients whose images had artifacts were excluded from the research. The remaining 279 patients were included. CT images of the patients were collected using 16- and 128-slice multidetector CT systems (MX-128-Slice and 16-Slice Multidetector, Philips Medical Systems). The voltage of the tube was 110 kV, and the slice thickness was 5 mm. The CT images were retrospectively obtained from the hospital’s picture archiving and communication system (PACS). They were evaluated with a joint decision by 2 radiologists with 7 and 16 years of experience in radiology, who were blinded to the clinical and CAG information of the patients. The radiologists agreed on the WSs together. Based on visual assessments of the existence and amount of calcium in each major coronary channel (LMCA, LAD, LCx, and RCA), the WS method assigns the following scores: 0, no visually detected calcification; 1, a sole high-density pixel; 3, the calcification is sufficiently dense to create a blooming artifact; and 2, calcification representing a condition between 1 and 3. The score was determined by summing the scores for every vessel (range 0-12) [11]. Figure 1 contains the CT image used for scoring.
Figure 1
Standard axial chest computed tomography demonstrating left anterior descending artery with a Weston score of 1 (A), of 2 (B), and of 3 (C)
The CAG images obtained from the PACS were evaluated by a cardiologist who was blinded to the clinical and WS data of the patients. When an artery had many aberrant segments it was categorized according to the section that had the most pronounced abnormality [12]. The presence of one major coronary artery with ≥ 50 stenoses at least was defined as OCAD [13].
Statistical analysis
IBM SPSS Statistics for Windows version 22.0 was used to analyse the data. Numbers and percentages were used for categorical variables. Previous studies defined a WS of ≥ 7 as severe calcification [6,7]. Therefore, the patients were divided into 2 groups: those with a WS of < 7 and those with a WS of ≥ 7. Then the CAG findings were used to create 3 groups of patients: those with normal vessels, those with vessels with < 50% stenosis and those with vessels with ≥ 50% stenosis. c2 and t-tests were used for the statistical analyses. Statistical significance was determined at p < 0.05.
Results
This research included a total of 279 patients. Their aver-age age was 63.2 ± 11.5 (range, 41-93) years, and 172 (61.6%) of them were men. Ninety (32.3%) had non-ST-elevation myocardial infarction, and 61 (21.9%) had ST-elevation myocardial infarction (Table 1), while 188 (67.4%) patients had CAC. Based on the evaluation of the main coronary vessels for CAC incidence, the left anterior descending (LAD) was the vessel with the highest incidence rate of CAC and the highest CAC score. The left main coronary artery (LMCA) had the lowest incidence rate of calcification (Table 2).
Table 1
Participants’ clinical and demographic characteristics
Table 2
Coronary artery calcification (CAC) and relevant score
According to the CAG findings, and 27 (9.7%) patients had normal coronary arteries. Fifty-one (18.3%) patients had wall irregularities or < 50% stenosis, whereas 201 (72.0%) had OCAD. Of the 201 patients with OCAD, the WS was 0 in 38 (18.9%) and ≥ 7 in 56 (27.9%). All patients with a WS of ≥ 7 had OCAD. The WSs according to the CAG scores of the patients are shown in Figure 2. Patients with a WS of ≥ 7 were significantly older than those with a WS of < 7 (p < 0.001). The incidence rate of having a WS of ≥ 7 was significantly higher in males than in females (p = 0.046). The WS was < 7 in all patients without OCAD (Table 3).
Table 3
Demographic and clinical characteristics of the patients according to Weston score
Discussion
It is important to identify individuals at risk of CAD because it is a preventable cause of morbidity and mortality. If not diagnosed in time, CAD can result in sudden death [14]. Studies show that the CAC score has diagnostic and prognostic importance in CAD [15,16]. The visual evaluation and ordinal scoring of CAC are useful in predicting disease prognosis [11,17,18]. The CAC score correlates with coronary atherosclerotic load [19].
Chest CT scans performed for other reasons may provide useful data for CAC evaluation, thereby facilitating the diagnosis of CAD. In patients with high CAC scores, early detection enables necessary examinations and early interventions for OCAD. However, studies have reported the lack of a standard format for reporting calcification detected on CT. If calcification is included in the patient report, it is often described as present or absent; if described as present, its severity is not specified [20-22]. Studies indicate that radiologists should routinely report the presence of CAC. Not only the presence of calcification but also the calcification score should be specified [10,11,23]. To ensure that the severity of calcification is also included in patient reports, a standard reporting system and set of guidelines for clinicians are needed. For this purpose, the Society of Cardiovascular Computer Tomography and Society of Thoracic Radiology has published guidelines that recommend reporting any CAC that is identified on noncontrast, noncardiac chest CT, as well as informing about the relevant methods and risk classification [19].
Radiologists can quickly and easily calculate the WS when reporting the findings of chest CT, without the requirement of any additional processing. If they include this scoring information, it can be lifesaving, particularly for those with asymptomatic OCAD. In the present study, to assess the WS for its predictive value in diagnosing OCAD, we compared the scores of 279 symptomatic patients with their CAG findings. CAG is the gold standard for the diagnosis of CAD. Hence, it is significant that we evaluated the CAG results of the same patients together with the calcification score in our study.
When the main coronary vessels were evaluated in terms of CAC incidence, LAD showed the highest incidence rate (64.5%) and LMCA showed the lowest (15.1%). This finding is consistent with those of previous studies [11,24].
In a study conducted by Kirsch et al. [6], a WS of ≥ 7 correlated well with an Agatston score of ≥ 400. In reference to this previous study, WS ≥ 7 was considered to indicate severe CAC. The incidence and severity of CAC increase with age. Furthermore, CAC is more common in men than in women [25,26]. In our study, the mean age of the patients with a WS of ≥ 7 was signi-ficantly higher than that of patients with a WS of < 7. In addition, the incidence rate of severe CAC was higher in the men than in the women.
In our study, all patients with a WS of ≥ 7 had OCAD. Based on this finding, a WS of ≥ 7 is a strong predictor for indicating that a patient is prone to OCAD development. The fact that patients with a high CAC score have a higher rate of OCAD compared to the CAG score is an important result. Therefore, we think that patients with a WS of ≥ 7 should undergo coronary CT angiography, myocardial perfusion scintigraphy, or CAG. To decide on the examination method to be performed, the clinical state of the patient should be considered.
A WS of ≥ 7 is indicative of OCAD, whereas a WS of < 7 does not necessarily suggest that the patient does not have OCAD. In our study, a large proportion (72.1%) of the patients with OCAD had a WS of < 7. Therefore, while evaluating patients with a WS of < 7, a holistic approach should be used to examine them while considering their risk factors, clinical findings, and WS.
Patients with a CAC score of 0 have a low risk of suffering a cardiac event in the future [27,28]. However, a CAC score of 0 does not guarantee that the patient will not develop CAD. There may be false negative results. The absence of coronary calcification does not exclude obstructive stenosis in symptomatic patients [29,30]. In the present study, the WS was 0 in 18.9% of the patients with OCAD.
Our study was designed as a retrospective study. The study group comprised patients with CAD or individuals at high risk of the disease.
Conclusions
Coronary artery calcification scoring can be performed using standard noncontrast chest CT, without the requirement of any additional equipment. The CAC score is useful for the early diagnosis of CAD and OCAD. Radiologists should assess patients’ CT findings to detect any possible CAC. If CAC is detected in the CT images, it should be scored and reported accordingly.