Introduction
Dyssynergic defecation (DD), or anismus, is defined as paradoxical contraction or inadequate relaxation of the pelvic floor muscles during defecation, which causes functional constipation [1]. It is accepted as an acquired behavioural problem and reduces quality of life [2]. Along with the anal manometry and balloon expulsion tests, magnetic resonance (MR) defecography is widely used to diagnose or rule out pelvic dyssynergia. Besides the functional abnormality, structural pathologies like rectocele, rectal intussusception, or rectal prolapse accompanying DD can also be well demonstrated by MR defecography [3].
The aim of this manuscript is to demonstrate the MR defecography findings of DD and to emphasize the key points of the imaging method.
Before magnetic resonance defecography
Constipation is a chronic problem, and patients usually indicate that they have been seeking help for a long time before they are referred to the radiology department for MR defecography. Patients with DD complain about repeated and prolonged attempts of evacuation, excessive straining during defecation, a sense of incomplete evacuation, bloating, hard and lumpy stool, and the need for digital manoeuvre to facilitate defecation [4].
When a patient presents with these complaints, the first step is to enquire a detailed patient history including systemic disorders (Parkinson’s disease, diabetes, etc.), medications, dietary habits, previous surgery, pregnancy, and childbirth history. Digital rectal examination should not be underestimated. Colonoscopy is not a diagnostic tool for DD unless there is a suspicion of colorectal cancer [2].
Anal manometry and rectal balloon expulsion tests may be performed simultaneously. Measuring the time required to expel a rectal balloon filled with water or air is known as a rectal balloon expulsion test. It is a useful screening method but may not always exclude DD [5]. Manometry measures anorectal pressures during rest, squeezing, and straining and also assesses first/urge/maximum tolerated rectal sense while an inserted rectal balloon is increasingly inflated. Patients with DD demonstrate that anal canal pressures either fail to decrease or paradoxically increase during defecation. These patients also fail to evacuate the inflated balloon within 5 minutes while sitting on the toilet [4]. It should be kept in mind that even asymptomatic patients can have findings of dyssynergic defecation by anal manometry [5].
Ultrasound (US) using transperineal or transrectal approaches is suggested as a first-step technique to visualise the pelvic floor anatomy and to assess non-complicated patients with pelvic floor dysfunction [6]. Dynamic US may also be a diagnostic tool for patients with DD but should be performed by experienced hands [7,8].
Conventional defecography can provide us all the information we need to diagnose DD. It would be less time consuming, easier, and cheaper to perform a conventional defecography instead of MR defecography if our only concern was DD. Conventional defecography can demonstrate inadequate opening of the anal canal, impaired evacuation of the rectum, inappropriate narrowing in the anorectal angle, and even accompanying rectocele or intussusception [9]. Conventional defecography also has the advantage of imaging in the physiological defecation position. Ionising radiation is one of the main disadvantages of this method, but it is not the only reason why MR defecography is preferred over conventional defecography in many institutions. MR units are widely available now, and radiologists are familiar with the cross-sectional anatomy of the pelvic floor on MR images. Visualization of the bladder, vagina-uterus, and small intestine without contrast administration eases the examination and provides comfort for the patient. Evaluating both the anatomy and function of the entire pelvic floor with a single examination that has high soft tissue contrast, that is non-invasive, and that does not utilise ionising radiation is a widely accepted method but preference may be based on the local availability and level of expertise [9,10].
Patient preparation
A radiologist or a trained MR technician should interview the patient before MR defecography. This examination is an uncomfortable experience for the patient, so the imaging method and the importance of patient cooperation should be explained in detail. Also, obtaining clinical information directly from the patient before imaging is very useful for the radiologist in order not to overlook multicompartment involvement. No premedication, no preparation for bowel cleansing, and no intravenous or oral contrast administration is required in standard procedure. 120–250 cc of ultrasound gel is commonly used to fill the rectum. The patients are usually instructed not to urinate in the hour immediately prior to the examination [11,12].
Magnetic resonance defecography technique
As open magnet MR systems are not widely available, MR defecography is generally performed using at least a 1.5-T closed magnet MR unit with phased array coils with patients in supine position and the knees slightly elevated on a pillow [12]. The MR imaging table should be covered with disposable sheets and adult diapers, or inflatable plastic enema rings may be used to protect the MR unit.
After T2-weighted fast spin-echo images in sagittal, axial, and coronal planes are acquired at rest for anatomic evaluation, ultrasound gel is instilled using a catheter with the patient in the lateral decubitus position. In some institutions ultrasound gel is mixed with 1-2 ml of gadolinium-based contrast medium [13]. Then functional imaging is performed using cine-type true fast imaging with steady-state precession (TrueFISP) or single-shot fast spin-echo (SSFSE) sequences in the midsagittal plane during squeeze, strain, and defecation [14]. When patient co-operation is not optimal or instructions for squeeze and strain phases lead to confusion, these phases may be omitted, but 3 or more attempts of the defecatory phase are indispensable for evaluation. Inadequate effort should be ruled out before diagnosing DD [3].
Table 1 shows the MR defecography parameters used in our department.
Magnetic resonance imaging findings of dyssynergic defecation
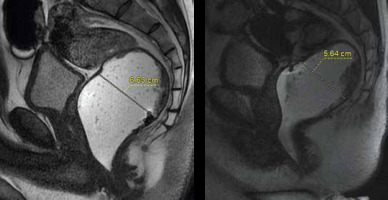
Normal evacuation should not last longer than 30 s, and more than 80% of the contrast media should be expelled. The most specific finding of DD is prolonged and incomplete evacuation during MR defecography [11]. Retention of more than 50% of rectal contrast at the end of defecation can be reported as clinically significant [4] (Figure 1A, B).
Figure 1
Rectal emptying can be assessed by measuring the maximum diameter of the contrast-filled rectum before (A) and after (B) defecatory attempts. Here we can see that most of the ultrasound gel is retained within rectum at the end of the examination
In healthy individuals the anorectal angle (the angle between the midline of the anal canal and the line parallel to the posterior rectal wall) increases by more than 20° during evacuation because of the relaxation of the puborectalis muscle. In DD, the puborectalis muscle is not relaxed during defecation, so a smaller increase or even a decrease in the anorectal angle can be seen on MR defecography (Figure 2A, B). Moreover, paradoxical contraction of the muscle may cause a prominent puborectal impression on dynamic images [15]. Due to the impression of the puborectalis muscle on the anorectal junction, a persistent narrowing, so-called “sandglass-like”, appearance has been described in the literature [16] (Figure 3).
Figure 2
There is no change in anorectal angle on sagittal cine images at rest (A) and during defecation (B). This is a significant finding in the diagnosis of dyssynergic defecation
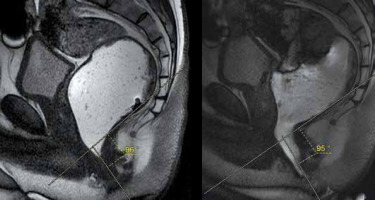
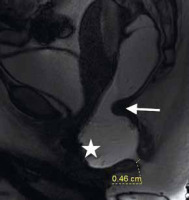
Figure 3
The impression of the puborectalis muscle on the anorectal junction during defecation causes a persistent narrowing (arrow). “Sandglasslike” appearance

Although there is no consensus about the usefulness of measuring the anal canal diameter, a diameter of less than 15 mm during defecation may indicate incomplete relaxation of the anal sphincter [17] (Figure 4). It has been reported that defecography can detect anismus more specifically when the straining sphincteral pressure exceeds 50% of the resting pressure [1].
Figure 4
On a sagittal cine image the impression of the puborectalis muscle on the anorectal junction (arrow), rectocele (asterisk), and minimal opening of the anal canal can be seen
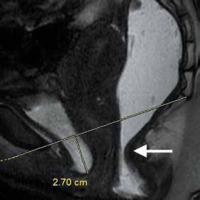
Besides the findings of DD, due to excessive straining during defecation, pelvic floor descent can also be seen on MR defecography (Figure 5). According to the “rule of 3”, the caudal descent of bladder base, fornix of vagina, and anorectal junction with respect to the pubococcygeal line is classified as mild (< 3 cm), moderate (3-6 cm), and severe (> 6 cm) [4].
Figure 5
Mild cystocele (< 3 cm) and “sandglass-like” appearance (arrow) are demonstrated during defecation
Another accompanying finding may be anterior rectocele, which is defined as abnormal bulging of the anterior rectal wall (Figure 4). Small rectoceles (< 2 cm) are not clinically significant, but moderate (2-4 cm) or severe (> 4 cm) rectoceles with contrast material retention after evacuation may cause a sense of incomplete evacuation [12].
Rectal intussusception may co-exist with DD, but it may not be demonstrated in patients with impaired evacuation because intussusception occurs when the rectum collapses [11].
Conclusions
MR defecography provides useful information about the morphological and functional integrity of the defecation process. There are key points for the diagnosis of DD, but optimal imaging criteria should be applied in order to make the diagnosis. Anal manometry can be suggested if patient co-operation is insufficient or if MR defecography findings are irrelevant.


