Introduction
In the anterior knee area there are three fat pads: infrapatellar (Hoffa fat pad), pre-femoral, and suprapatellar (quadriceps fat pad). The relationship between acute or recurrent microtrauma, meniscal or knee joint ligamentous damage, and Hoffa fat pad has been demonstrated in various studies [1-3]. Studies about hyperintensity related to oedema in quadriceps fat pad, which we frequently encounter in our magnetic resonance imaging (MRI) practice, are limited. The quadriceps fad pad is in close relationship with the patellofemoral joint (PFJ). It is located posterior to the quadriceps tendon patellar insertion and superior to the retro-patellar cartilage. It is triangle shaped. Due to this anatomical location, it has a close anatomical relationship with the knee extensor mechanism. In this MRI-based study, we aimed to evaluate the relationship between MRI signal and morphological features of quadriceps fat pad, and various pathologies of PFJ including trochlear asymmetry, dysplasia as well as patellar morphology and localisation.
Material and methods
In total 457 knee MRIs performed between September 2018 and October 2018 in our clinic for various reasons were evaluated retrospectively, after obtaining Ethics Committee approval. Patients with a history of open or arthroscopic surgery, severe trauma, and tumour were excluded. As a result, a total of 61 knee images from 51 patients in whom suprapatellar quadriceps fat pad oedema was detected among 403 MRIs were included.
All MRI examinations were performed using phased-array knee coil with a 1.5-Tesla device (Achieva, Philips Medical Systems, Best, The Netherlands). In our institution standard knee MRI protocol is as follows: axial fat-suppressed turbo spin echo (TSE) proton-weighted images (TR/TE 3000/30; NEX 4; slice thickness 4 mm; interslice gap 0.5 mm; matrix 320 × 256; FOV 14 cm), sagittal proton-weighted images (TR/TE 1500/30; NEX 3; slice thickness 4 mm; interslice gap 0.5 mm; matrix 352 × 256; FOV 16 cm); coronal proton-weighted images (TR/TE 3600/30; NEX 3; slice thickness 4 mm; interslice gap 0.5 mm; matrix 384 × 320; FOV 16 cm); sagittal T1-weighted spin-echo images (TR/TE 500/20; echo-train length 1; slice thickness 4 mm; interslice gap 0.5 mm; matrix 320 × 256; FOV 16 cm).
Examination results were evaluated by two radiologists with over five years of experience in the field of musculoskeletal radiological assessment. Image analyses were made on PACS system (Infinitt Healthcare, South Korea).
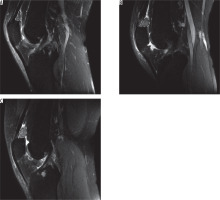
Patients were divided into three groups according to the severity of the quadriceps fat pad oedema (Grade 1: slight signal increase, Grade 2: Similar signal characteristics with cartilage, Grade 3: Signal intensity greater than the cartilage) (Figure 1). In cases of interobserver disagreement the final decision was made on consensus with consultation of the third radiologist.
Figure 1
Quadriceps fat pad signal intensity grading. Quadriceps fat pad borders are indicated by white dotted line. A) Grade 1: slightly increased signal intensity. B) Grade 2: Signal intensity similar to cartilage. Also, there is indentation to the prefemoral fat pad. C) Grade 3: Signal intensity more than the cartilage
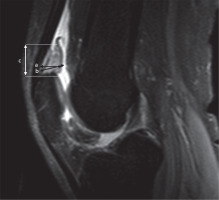
Quadriceps fat pad sizes were measured in sagittal sections in millimetres, including transverse, craniocaudal, and oblique. The mean values of the two measurements were used for statistical analysis. The transverse dimension was obtained from the posterior of quadriceps tendon towards the fat pad dorsal border, parallel to the patient’s axial plan. The craniocaudal dimension was obtained from the superior border of the fat pad to the inferior border, perpendicular to the patient’s axial plan. The oblique dimension was obtained from the anterior border to the posterior border, parallel to the superior border of the patella (Figure 2).
Figure 2
34-year-old man with increased quadriceps fat pad signal intensity. Sagittal proton-weighted magnetic resonance imaging showing quadriceps fat pad dimensions: a – anteroposterior, b – oblique, c – craniocaudal
The indentation of the fat pad on the suprapatellar recess was evaluated according to the presence of the posterior convex contour of the fat pad. Two independent radiologists evaluated these measurements. In the event of noncompliance, a final decision was reached with the help of a third radiologist. The relation between the sizes of the fat pad oedema and presence of posterior indentation as well as the correlation between quadriceps fat pad oedema and pre-femoral fat pad oedema, patella morphology, patellar tilt, quadriceps tendon injury, and meniscal and patellar cartilage pathology were evaluated.
The morphology of patella was evaluated according to Wiberg classification in the axial plane [4]:
type 1: roughly equal medial and lateral facets,
type 2: slightly smaller than lateral-medial facet,
type 3: distinctly small medial facet.
Patella localisation was evaluated by using the Insall- Salvati ratio in sagittal sections. The patella was evaluated as patella Baja when the patellar tendon/patellar height ratio was < 0.8, and as patella Alta when the patellar tendon/patellar height ratio was > 1.2. The length of the patellar tendon was measured from the patella lower pole to the point of tibial insertion, and the patellar height was measured as the length between the upper and lower poles of the patella [5] (Figure 3).
Figure 3
41-year-old woman. Midsagittal T1W magnetic resonance imaging slice. Insall-Salvati ratio; patellar tendon length/patellar height (b/a) is shown

Axial sections were used for patellar subluxation evaluation. The patella was considered abnormal when the distance between the furthest lateral point of the lateral facet and the lateral border of the lateral trochlear facet was > 2 mm [6].
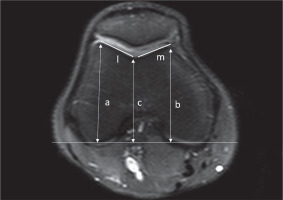
In the evaluation of trochlear depth, the line passing tangentially to the posterior portions of both femoral condyles was considered a reference. Then, when the length of the perpendicular line from the floor of trochlea to the reference line was extracted from the average length of the perpendicular lines from the most anterior parts of medial and lateral facets to this line was smaller than 3 mm, the trochlear groove was considered as shallow [7] (Figure 4). In the evaluation of trochlear dysplasia, trochlear facet asymmetry, medial facet to lateral facet ratio less than 0.4 (< 0.4) was accepted as dysplasia [7] (Figure 4). The angle of the trochlear groove was evaluated as hypoplastic when the angle between the medial and lateral facets was > 144° [8]. Also, patellar and trochlear morphology were evaluated in terms of age and gender differences.
Figure 4
Same patient as in Figure 2. Right knee axial proton-weighted magnetic resonance imaging slice passing through femoral condyles. Patellar facet dimensions: lateral (l) and medial (m). Femoral trochlear depth measurement: Line from the floor of femoral trochlea perpendicular to the reference line extracted from the average of the lines from the most anterior parts of lateral and medial femoral trochlea perpendicular to the reference line (a + b/2 – c)
Statistical analysis
Statistical analyses of the data were performed with SPSS (Statistical Package for the Social Sciences) version 15.0. Data for continuous variables were expressed as mean ± standard deviation, and data for categorical variables as frequency and percentage. For the categorical variables the χ2 test and Fisher test were used, for the continuous variables for comparing two groups Mann-Whitney U test, for comparing more than two groups Kruskal-Wallis H test, and for correlation the Pearson correlation test was used. The results were evaluated with a 95% confidence interval and a significance level of p < 0.05 (*p < 0.05, **p < 0.01, ***p < 0.001). Interobserver reliability was assessed with the Cohen kappa coefficient.
Results
A total of 61 cases were studied, of which 51 were bilateral, 10 were bilateral, 28 (45.9%) were female, and 33 (54.1%) were male. Their ages ranged from 16 to 70 years with a mean of 39.61 ± 10.78 years. Twenty-nine right knees (47.5%) and 32 left knees (52.5%) were evaluated.
In comparison by gender, the severity of the trochlear groove, trochlear medial, and lateral facet dimensions were significantly higher in males than in females. Statistically, a significant difference was not found between male and female cases, regarding trochlear groove angle, trochlear medial/lateral facet ratio, shallowness according to the angle of trochlear groove, shallowness according to the depth of the trochlear groove, facet asymmetry, patella morphology, patella placement, and patellar subluxation (p > 0.05).
There was no statistically significant relationship between age and trochlear groove angle, trochlear groove depth, trochlear medial facet, trochlear lateral facet, trochlear medial/lateral facet ratio, shallowness according to the angle of the trochlear groove, shallowness according to the depth of trochlear groove, facet asymmetry, and patella localisation type (p > 0.05).
There was no statistically significant relationship between the severity of quadriceps fat pad oedema and the presence and severity of pre-femoral fat pad oedema, patella morphology, the presence of patellar tilt, and the presence of quadriceps tendon damage (p > 0.05).
When the grade of quadriceps fat pad oedema and posterior indentation was compared, the posterior indentation of the fat pad was statistically lower in patients with Grade 1 than Grade 2 and 3. On the other hand, no statistically significant difference was found between the patients with and without posterior indentation regarding measurements (AP, CC, oblique) of fat pad (p > 0.05).
The relationship between the severity of quadriceps fat pad oedema and the trochlear groove angle, trochlear depth, and trochlear facet ratio is shown in Table 1.
Table 1
The relationship between the severity of quadriceps fat pad oedema and the trochlear groove angle, trochlear depth, and trochlear facet ratio (p > 0.05)
There was no significant relationship between the severity of quadriceps fat pad oedema and patellar localisation disorder, meniscal damage, and chondromalacia (Table 2). There was no correlation between patellar morphology and trochlear groove angle and trochlear facet ratios.
Table 2
The relationship between the quadriceps fat pad oedema and patellar localisation, meniscal pathology, and chondromalacia
The distribution of the different pathologies is shown in Table 3. Six of the knees (9.8%) had none of these pathologies, and 55 (90.2%) had at least one of these pathologies. The ratio of at least one of these pathologies was statistically significantly higher than those without (p < 0.0001).
Table 3
Frequency of various pathologies, their percentages, and p-values
Discussion
In this study, the relationship between quadriceps fat pad oedema and various pathologies in the knee extensor mechanism was evaluated. According to the results, quadriceps fat pad posterior indentation was associated with fat pad oedema. While none of the parameters evaluated in the extensor mechanism had a relationship with quadriceps fat pad oedema individually, it was found that there was a significant relationship between the presence of at least one of these parameters in people with fat pad oedema.
Quadriceps fat pad is a fat tissue located between the quadriceps tendon and the suprapatellar recess and is the smallest fat pad in the anterior knee region [9]. Standard sizes have been demonstrated in various studies, with an average size of 8 ± 2 mm in men and 7 ± 2 mm in women [10]. The posterior aspect of the fat pad is located at the anterior of the suprapatellar recesses; thus, the posterior surface is covered with synovium. The knee is in contact with the femoral trochlea during flexion-extension movement [10].
The relationship between quadriceps fat pad oedema and anterior knee pain has been evaluated in various studies, and it has been established as a cause of pain [11,12]. In this study, we considered the presence of convexity in the quadriceps fat pad posterior contour as the criteria of indentation to suprapatellar recess, and it was found to be significantly higher in patients with higher grade oedema. However, in our study, quadriceps fat pad anteroposterior diameter was found to be larger (10.2 mm) compared to other studies with mass effect, whereas there was no significant relationship between mass pad size and mass effect [13]. This supports the studies that advocate that visual assessment in quadriceps fat pad mass effect is a more appropriate assessment method than AP numeric value [11,12,14].
In our study, the surface size and angle values of the bony structures were compared between the genders. Accordingly, there was no significant correlation between angular values and patellar morphology, facet asymmetry and patellar localisation and trochlear asymmetry or trochlear groove depths. This shows that dysplasia and hypoplasia, which may affect the extensor mechanism, are independent of gender. Also, no correlation was found between these parameters and age. Accordingly, in comparison to the higher size values of women compared to men, there was no significant relationship between angular values of genders, and thus there was no significant relationship between patellar morphology, facet asymmetry, patellar localisation, and trochlear asymmetry or depth of the trochlear groove. This shows that dysplasia and hypoplasia, which may affect the extensor mechanism, are independent of gender. Also, no correlation was found between these parameters and age.
Infrapatellar fat pad was described by Hoffa in 1904 [15], and various studies have demonstrated the relationship between MRI signalling properties and inflammation and anterior knee pain [1,2,16,17]. In our study, unlike Hoffa’s disease in which pathologies such as trauma, malalignment, and impingement serve as aetiological factors, we investigated the presence and the possible relationship of the nontraumatic mechanisms like structural/anatomical disorders. We did not find a separate relationship between quadriceps fat pad oedema and patella localisation, patellar morphology, the presence of patellar tilt, femoral trochlear asymmetry, trochlear angle, and the presence of trochlear dysplasia according to depth. In our study, while the cause of fat pad oedema was unknown, at least one of these pathologies was present in 55 (90.2%) of the 61 patients included. This result contradicts with the study of the patellar malalignment parameters of Tsavalas et al. [14]. In addition, the study by Roth et al., which evaluated pathologies associated with increased signal intensity in quadriceps fat pad, suggested that the existence of a developmental problem in the extensor anatomy as a result of the presence of fat pad oedema in patients with no history of direct trauma or overuse, could be the underlying cause but did not find a significant relationship [12].
In addition to the intact patellar retinaculum, the normal articular pattern of patella and trochlea are important factors contributing to PFJ stability [18]. In addition to these, localisation disorders, such as the patella Alta, can also provide a basis for patellofemoral instability [18,19]. In our study, the rate of patients with patellar Alta was 57.1%. Although there was no significant relationship between patella localisation and quadriceps fat pad oedema, the fact that the reference limit value we used in the diagnosis of patella Alta was lower than the higher limit values accepted in different studies may have affected the overall number [20]. The quadriceps muscle is also an active stabiliser of the PFJ. In instability cases, the abnormal contraction of the quadriceps muscle may cause oedema in the quadriceps fat pad, which is associated with this tendon. This may be an indirect finding of instability.
Furthermore, patellofemoral contact with high knee flexion is at the upper pole level of the patella and in this position, it is in contact with the trochlea suprapatellar fat planes [10]. However, in our study there were not sufficient data to evaluate this. More extensive studies should be conducted in order to support this hypothesis, in which patients’ daily activities and occupations are also questioned. Falkowski et al. showed that the increase in the lateral patellar facet cartilage in people with instability was due to chronic friction of the lateral facet of the patella with the lateral femoral condyle and suggested that this could be an indicator of instability [21]. A similar hypothesis can be considered for the quadriceps fat pad as an adjunct to any pathology in the extensor mechanism.
There have been contradicting results about quadriceps fad pad oedema in different studies, and there is no apparent reason. In light of the results we obtained in our study, we demonstrated that quadriceps fat pad oedema is associated with pathologies related to the extensor mechanism. Khajuria et al. showed that the pathologies related to PFJ were frequently underreported in MRI [21]. In this study, we concluded that quadriceps fat pad oedema, which can easily be observed in sagittal MRI sections, maybe a warning factor in the pathologies related to the PFJ, which is frequently ignored in MRI reports.
Limitations
Our study was a retrospective study, and each patient had an indication for MRI. Thus, we could not compare with the findings in asymptomatic individuals. Also, because our study was MRI based, we could not correlate the examination findings with quadriceps fat pad oedema. Finally, histopathological and clinical correlation of quadriceps fat pad is a prominent limitation of this study.


