Dear Editor,
I read with great interest and joy the article in the last issue of Insights into Imaging: “The role of radiologist in the changing world of healthcare: a White Paper of the European Society of Radiology (ESR)” [1]. I agree with every word and view of our specialty from all sides, and I wish that as many fellow radiologists and radiologists in spe as possible read it with understanding. This is extremely important for any radiologist who is struggling not to drown in a burnout syndrome. However, I see two problems that are not in this position paper of the European Society of Radiology:
it should reach out to the representatives of other specialties who use our “services” (i.e. virtually everyone);
there is no idea in it (and probably cannot be, as it is not a simple matter) of how – according to the law and all the rules – to make us co-decision makers about the way, time, and method of diagnosing our patients (or not imaging them if they have already been diagnosed and their disease or, worse, developmental variant does not require it [e.g. annual MRI follow-up of a pineal cyst that has a diameter of a few millimetres or of a non-ossifying fibroma] or if continued follow-up is of no use [e.g. annual MRI follow-up of degenerative disease of the spine in a patient who does not wish to have surgery or who no orthopaedist or neurosurgeon will operate on because of the severity of the disease]).
By writing the latter I mean both the welfare of our patients, i.e. the welfare of the patients referred to us for diagnostic tests, their welfare at the time of imaging and in the future, as well as the welfare of other patients who require financial outlays for treatment.
The tremendous development of imaging modalities has resulted in what the authors write about: “often-unsustainable demand for increasing numbers of studies”. These studies are, to put it mildly, not infrequently completely unnecessary and unwarranted. This has been my “hobby” for years [2], and although I constantly talk about it in lectures and conversations with colleagues (radiologists and representatives of other specialties, like Cato the Elder, an implacable enemy of Carthage, who ended all speeches in the Roman Senate with this sentence: Besides, I believe that Carthage should be destroyed), it is not enough.
There are not many countries in the world, or in Europe, where financial resources for health care are in-exhaustible. If huge outlays are incurred on expensive unnecessary imaging tests, then there must be a lack of money for something else, such as treatment. More than once I have taken part in fund-raising and I have paid money for the treatment of a sick person from my family or from among my close friends and acquaintances, because their treatment was not reimbursed. The financial system of any country cannot bear the burden of diagnostics and treatment if a big part of it is unjustified. And how, after such an expense, can we not be frustrated when reporting another, e.g. the fifth brain MRI scan of a patient with a diagnosis of “headaches”?
This should be taught to fellow clinicians as well as radiologists. Perhaps the solution to this problem would be – thanks to IT development – to create a central regi-ster of patients and their examinations, so that claimant patients could not force referrals, and doctors unaware of their previous history do not issue subsequent referrals for examinations that have already been repeatedly, and often unnecessarily, ordered and performed.
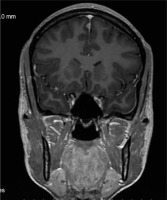
Finally, there is the question of what legal conditions would have to be created for a radiologist – being a clinical doctor – to refuse to perform an unnecessary imaging study that has already been performed many times and/or does not contribute anything. Our problem is that we cannot refuse a senselessly ordered study on an outpatient basis (whereas we have that chance in the hospital, after consulting with the referring physician) (Figure 1). We do not do this for fear of lawsuits, and this is one of the reasons why “47% of radiologists are suffering from burnout”, including myself. Yet I still occasionally feel the urge to fight.