Introduction
One of the most common complications of radical prostatectomy following vesicourethral anastomosis is urinary leakage, which has an incidence of 0.3% to 15.4% [1]. The healing of urinary leakage is usually self-limited and resolves in 2 or 3 days postoperatively [2]. However, in cases with persistent urinary leakage, urinary diversion or ureteral stenting is primarily considered. If these manoeuvres fail, occlusion of the fistulous tract is recommended because surgical repair may be challenging [2,3].
Endourologic or percutaneous approaches using a variety of devices and embolic agents have been used as minimally invasive treatments for postoperative urinary leakage [4,5]. Coils and N-butyl-2-cyanoacrylate (NBCA) are frequently used as embolic agents [6], and the most common routes for treating anastomotic leakage are percutaneous antegrade access or retrograde access through the urethra [3,6,7]. However, reports on the use of pre-existing Jackson-Pratt (JP) drainage tubes as the access for embolization are limited.
We present a case of vesicourethral anastomotic leakage embolization with an Amplatzer vascular plug (AVP) and NBCA through a JP drainage tube, in which the AVP was expected to block the anastomotic fistula and NBCA was expected to obliterate the urinoma cavity.
Case presentation
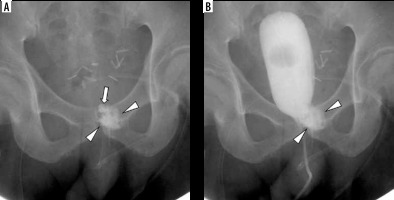
A 59-year-old male with rectal cancer invading the prostate and urinary bladder underwent low anterior resection and radical retropubic proctectomy 15 months ago. One month later, the patient presented with persistent urinary leakage at the posterior aspect of the vesicourethral anastomotic site, which was confirmed by cystography (Figure 1). The amount of urinary leakage through the JP drainage tube was 350 ml/day, and its nature was urine. Although the indwelling Foley catheter was retained for 1 month, the fistula persisted without infection.
Figure 1
Cystography (A) and axial computed tomography scan (B) 1 month after prostatectomy. Contrast agent leakage (arrows) is shown at the posterior aspect of the vesicourethral anastomotic site on the left side
At the time of interventional procedure consultation, there were 2 JP drainage tubes near the vesicourethral anastomosis, 1 of which was later changed with a short 65 cm 5 Fr Kumpe (Cook Medical, Bloomington, IN, USA) over a stiff guidewire (180 cm, Glidewire Terumo, Tokyo, Japan). The fistula consisted of a single moderately sized defect. Because embolization with coils carries a significant risk of migration, embolization with an AVP device was preferred. After the bladder was negotiated with a stiff guidewire, a short 8 Fr sheath with a radiopaque marker (Boston Scientific, Marlborough, MA, USA) was inserted into the bladder. The Foley catheter was clamped to retain contrast agent within the bladder, which helped in the identification of the fistula. Then, the AVP (type II, 12 mm diameter, 9 mm long; St. Jude Medical, Plymouth, MN, USA) was inserted across the fistula. The Kumpe catheter with side holes (by needle punching) was then inserted through the sheath into the urinoma cavity. The urine in the urinoma cavity was aspirated, and the contrast agent was readily delivered through the catheter. After flushing with D5W (5% dextrose), the cavity was obliterated with 3 vials of NBCA (Histoacryl; B.Braun AG, Melsungen, Germany) mixed at a ratio of 1 : 1 with ethiodised oil (Lipiodol; Guerber, Vellepinte, France). The cavity seemed to have been well-obliterated (Figure 2).
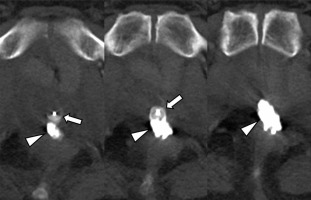
Figure 2
Radiograph (supine position) after embolization of the contained vesicourethral fistula. The fistula was embolized with an Amplatzer vascular plug (arrow), and the urinoma cavity was embolized with N-butyl-2-cyanoacrylate (asterisk) through the JP drainage tube

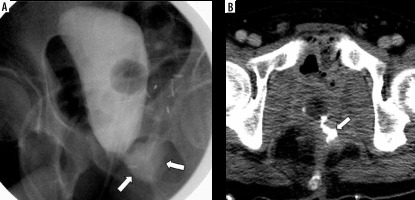
Cystography carried out 4 days after embolization showed the NBCA density and AVP (obscured by overlapped NBCA) at the anastomotic site without contrast agent leakage (Figure 3). CT scans acquired at 1-month and 1-year follow-ups showed stable AVP position and complete obliteration of the cavity by NBCA (Figure 4).
Discussion
Persistent vesicourethral anastomotic leakage is a significant loss of urine, usually above 100 or 200 ml, after the third day postoperatively. The prevalence of persistent vesicourethral anastomotic leakage is low, and there are only a few published cases reporting that the leakage is difficult to control and increases the possibility of extended hospital stay in addition to the risk of other complications [8-10].
Vesicourethral anastomotic leakage is primarily diagnosed by the presence of contrast agent extravasation in conventional cystography. However, CT scans can provide more information, especially with 3-dimensional volume estimates, which allows better delineation of the size and configuration of the fistula and cavity for determining treatment details [11,12].
Treatment of vesicourethral anastomotic leakage is challenging, and this complication can indefinitely prolong the hospitalization period and add the risk of adverse events such as secondary infection by resistant germs [8]. Approaches for managing this leakage include proximal or distal urinary diversion, endoscopy, laparoscopic or open surgical repair, and minimally invasive techniques.
The application of NBCA has recently been reported in different branches of surgery as well as for the management of urinary fistulas [3-7]. NBCA is a strong tissueadhesive material that can seal the wall of urinoma cavities and consequently obliterate the space of urine accumulation [6]. A sealant (Glubran 2™) composed of NBCA monomer and metacryloxysulpholane monomer showed good biocompatibility and progressive reabsorption without causing foreign body granulomas, and it has shown high success rates with few complications in several clinical series [6,7].
AVP was approved for use in endovascular embolization of medium-to-large vessels as an alternative to coils and detachable balloons. Accordingly, several nonvascular applications of the AVP have been described, including the treatment of bronchopleural fistulas and, only recently, urinary tract fistulas [13-15]. In our current case, AVP was used to block urine flow as much as possible to the urinoma cavity because the urine flow pressure is known to be low.
The urethra is commonly used as an access to a vesicourethral anastomotic fistula, but cavity obliteration may be difficult after fistula embolization. If the guidewire can reach the fistula through the cavity, cavity obliteration would be easy after fistula embolization; therefore, considering that surgical drains are used as an alternative route for postoperative abdominal abscess [16], surgical drains such as a JP drainage tube may also be used as a viable alternative to the urethra. As shown in our case, if the urinoma cavity is contrasted with a contrast agent through the JP drainage tube, the guidewire may be able to access the anastomotic fistula through the JP drainage tube.