Introduction
Pleural lymphoma is a medical condition characterised by shortness of breath and obscure chest pain, which may be a diagnostic challenge, especially when it occurs in children. Plain chest X-ray and computed tomography (CT) scan are the main imaging techniques and are the initial diagnostic methods utilised.
Case report
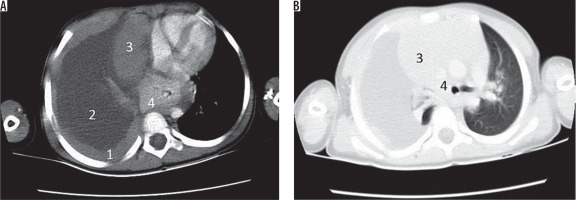
A four-year-old boy was admitted to the emergency ward with persistent pain in the right thoracoabdominal region, which had been present for at least two months. The patient had recently developed dyspnoea and was complaining of extreme sweating, which had started a week ago. The patient was normotensive, had a heart rate of 80 bpm, respiratory rate of 21 breaths per minute and was not febrile. Blood oxygen saturation was 92% without external respiratory support. The patient had no history of recent infections or any documented immune deficiency syndromes. The patient did not have a significant past family medical history, and he was not a passive smoker. On clinical examination, the patient was agitated and had decreased respiratory sounds on the right chest. Percussion of the right thorax was dull. The patient’s weight was 15 kg, down from 19 kg six months earlier. The patient was admitted to the general paediatrics ward and underwent diagnostic imaging. Figures 1 and 2 illustrate the imaging results. Chest X-ray showed an opaque right thorax, with no other significant findings. CT scan revealed a nodular thickness of the pleura, with no mediastinal lymphadenopathy. After consultation from the surgical team, the patient underwent thoracotomy, and a biopsy was taken from the pleura. Macroscopic evaluation showed a cream tan mass with a heterogeneous cut surface. Microscopic evaluation showed a small cell malignant tumour, which consisted of monomorphic lymphoid cells with fine granular nuclear chromatin, with high mitotic rates and infiltration of the surrounding fat tissue and vascular structures with considerable necrosis. Immunohistochemistry resulted in the specimen staining positive for CD99, CD3, vimentin, and Ki67, while negative for CD20, CD34, CD79a, NSE, synaptophysin, and chromogranin. This was consistent with the diagnosis of acute lymphoblastic pre-T cell leukaemia. After the diagnosis was made, the patient received the BFM-NHL treatment protocol, which consisted of two months of induction protocol, 50 days of consolidation protocol, 50 days of re-induction protocol, and finally 24 months of maintenance therapy [1]. Figure 3 illustrates the CT results after treatment. The patient was followed up for three years, and in this interval, periodic clinical examinations and PET-scans have shown that he remains disease free.
Figure 1
Initial computed tomography scan obtained from the patient. A) Mediastinal window, B) lung window. 1 – shows a diffuse right sided pleural thickening, 2 – shows a massive pleural effusion, 3 – shows the right lung which has collapsed because of the massive effusion, 4 – shows the shifting of the mediastinum to the other side
Discussion
Pleural lymphoma is a rare form of primary lymphoma, which presents with symptoms such as dyspnoea, pain on the effected hemi-thorax, night sweats, decreased exercise capacity, and weight loss. Previous studies have shown that a considerable number of individuals with pleural lymphoma have risk factors such as a history of smoking, pulmonary tuberculosis, exposure to radiation, exposure to asbestosis, infection with Epstein-Barr virus (EBV), immunodeficiency, presence of chronic inflammation, and probably more [2,3]. Most cases reported are male and are usually over 40 years old. The diagnosis of primary lymphoma of the pleura is usually made by a combination of physical examination, imaging modalities, and biopsies. In physical examination, the patient may be without any significant findings or may present with decreased respiratory sounds. Percussion of the chest cavity may also illicit dullness on the effected hemi-thorax. After the initial examination, a combination of chest X-rays, CT scans, magnetic resonance images (MRIs), and positron emission tomography (PET)/CT scans may be used to investigate the pathology and to facilitate the act of obtaining a biopsy. Usually the biopsy shows an infiltrate of large B-cell lymphomas and marginal lymphomas. After the definite diagnosis, suitable treatment is initiated. The majority of cases presented to date have been treated with the CHOP regimen (cyclophosphamide, doxorubicin, vincristine, and prednisone), which is the standard treatment for non-Hodgkin’s B-cell lymphoma. This regimen has proven to be of beneficence for cases with diffuse large B-cell lymphomas, but has also shown considerable mortality, especially because of neutropaenic fever [4] (Table 1). In this case report, we discuss a four-year-old Azeri boy who was diagnosed with primary pleural lymphoma. The patient had no history of the aforementioned risk factors and was considerably younger than almost all patients previously reported with primary pleural lymphoma. Of note, the pathology of the lymphoma was of pre-T-cell lymphoma type, again a rare finding. In scientific literature, only a single similar case has been reported before. Karadeniz et al. reported a 2.5-year-old girl who was admitted to the Paediatric Hospital with the chief compliant of dyspnoea. CT scan showed a mass in the left thoracic cavity, and biopsy revealed that the malignant mass was indeed an infiltrate of lymphocytes positive for UCHL-1, a marker of T lymphocytes. The patient received the modified LSA2L2 therapy regimen and after the last cycle of chemotherapy, received 1800 cGy of cranial radiotherapy. After 11 months of remission the patient experienced an isolated relapse in the nervous system, which was treated with re-induction and more radiotherapy. The patient died four months after the relapse due to neutropaenic fever [5]. As the case presented in this report, the patient had no history of exposure to common risk factors and presented in a young age.
Table 1
Reported cases of pleural lymphoma
| Country | Age | Past medical histroy | Sex | Chief complaint | Biopsy results | Radiologic modality/Radiologic findings | Treatment | Reference |
|---|---|---|---|---|---|---|---|---|
| China | 65 | Chronic obstructive pulmonary disease | Male | Mild dull pain on the right side of the chest | Diffuse large B cell lymphoma | CT/Inhomogeneous pleural thickening on the right without mediastinal lymph node enlargement | R-CHOP | 12 |
| Spain | 78 | Chronic empyema | Male | Weight loss and dyspnoea | Non-Hodgkin lymphoma | CT/Pleural mass with pleural effusion and empyema | CHOP | 13 |
| Portugal | 80 | N/A | Male | Dyspnoea, anorexia and asthenia | Primary pleural lymphoma with cells staining positive for CD20, Bcl2, Bcl6, PAX5 and CD70a, CD10, MUM1, and p53 | CT/Extensive right pleural effusion, without mediastinal or hilar lymphadenopathies | N/A | 14 |
| India | 18 | N/A | Male | Left-sided chest pain | Diffuse large B-cell non-Hodgkin’s lymphoma | CT/Pleural effusion | ATT + oral prednisolone | 15 |
| Korea | 80 | N/A | Male | Cough | Marginal zone B-cell lymphoma | CT/Pleural sandwich sign | N/A | 6 |
| Korea | 68 | N/A | Male | Dyspnoea | Diffuse large B-cell lymphoma | N/A | 6 | |
| China | 74 | N/A | Female | Right-sided chest pain | Small B-cell lymphoma expressing CD20 | CT/Bulky pleural mass and pleural effusion | Pleurodesis without radiation therapy | 16 |
| France | 72 | Pulmonary tuberculosis | Male | Chest pain and axonal neuropathy | B cell lymphoma | CT/Pleural tumour invading the chest wall | The patient received corticosteroids and did not receive chemotherapy because of poor functional status | 17 |
| Greece | 63 | N/A | Male | Progressive dyspnoea and non-productive cough | Extranodal follicular lymphoma of the pleura | CT/Plaque-like thickening of the pleura without mediastinal lymphadenopathy | R-CHOP | 18 |
| India | 20 | Smoker | Male | Left-sided chest pain | High grade diffuse large B cell type | CT/Pleural-based soft tissue mass with irregular margin with no visible effusion | Cyclophosphamide, vincristine, adriamycin, and prednisolone | 19 |
| Korea | 65 | N/A | Female | Dermatomyositis | Diffuse large-cell lymphoma | PET scan/Increased absorption of F18-FDG in the pleura and the limb griddles | R-CHOP | 9 |
| Oman | 58 | N/A | Male | Shortness of breath and left hypochondrial pain | Diffuse large B cell lymphoma | CT/Circumferential nodular masses involving the left parietal pleura gallium scan/Increased uptake in the left thoracic cavity | N/A | 20 |
| Turkey | 2.5 | N/A | Female | Fever and dyspnoea | T-cell lymphoblastic lymphoma | Solid mass and pleural thickening in the left hemi-thorax | Modified LSA2-L2 | 5 |
| China | 71 | Pyothorax resulting from tuberculosis | Male | Haemoptysis, dyspnoea, purulent sputum, discomfort on right chest | Diffuse large B cell lymphoma | CT/Collections of gas inside the large pyothorax, which was lined by a calcified wall/MRI – a mass was seen | Cyclophosphamide, vincristine, procarbazine, and prednisolone | 21 |
| Japan | 81 | Epstein-Barr virus | Male | Right chest pain and dyspnoea | B-cell lymphoma staining positive for CD45 and CDw75 | N/A | Modified CHOP | 22 |
| Japan | N/A | Epstein-Barr virus | N/A | N/A | T-cell-rich lymphoid infiltration | N/A | N/A | 23 |
| United Kingdom | 59 | Exposure to asbestosis | Male | Left sided chest pain and dyspnoea | Low grade marginal zone lymphoma | CT/Irregular thickening of the pleura coupled with sclerosis of the pleura | Chlorambucil | 24 |
| United Kingdom | 49 | Tuberculosis | Male | Weight loss, non-productive cough, and dyspnoea | Low-grade marginal zone lymphoma | CT/Subcarinal nodes and left pleural effusion coupled with a collapsed upper lobe | Chlorambucil and prednisolone | 24 |
| China | 57 | Previous DLBC lymphoma | Male | Dyspnoea and decreased exercise tolerance | DLBC lymphoma | CXR/Left sided pleural effusion | N/A | 25 |
| China | 49 | N/A | Male | Left chest wall pain | DLBC lymphoma | PET/Multiple lymphoid invasions of the left axillary, internal mammary, and intercostal lymph nodes | CHOP | 26 |
| India | 12 | N/A | Female | Cough | DLBCL lymphoma | Multi-loculated pleural collections, thick and thin septae and a partially collapsed lung | MCP 842 regime for non-Hodgkin lymphoma with alternating regimes including cyclophosphamide, adriamycin, vincristine, and ara-C and another regime consisting of etoposide, vincristine, methotrexate, ifosfamide, and mesna | 27 |
| France | 67 | N/A | Male | Weight loss | Diffuse large B-cell NHL | N/A | Pleurodesis and CHOP-Rituximab | 28 |
| Turkey | 14 | N/A | Male | Dyspnoea and cough | Lymphoblastic lymphoma of T-cell origin | CT/Bilateral thickening of the pleura coupled with atelectasic regions | LMT89 group B | 28 |
| France | 87 | Infection with HHV-8 | Male | Dyspnoea | T-cell origin NHL | N/A | N/A | 29 |
| Spain | 52 | N/A | Male | Dyspnoea | MALT lymphoma | MRI/Homogeneous pleural masses that showed hypointense signal on T1-weighted sequences and were hyperintense on T2-weighted sequences | N/A | 30 |
| Greece | 37 | N/A | Female | Dyspnoea | Nodular sclerosis classical HL | N/A | N/A | 31 |
| Greece | 63 | Smoking | Male | Dyspnoea | Extra-nodal follicular lymphoma of the pleura | N/A | N/A | 31 |
Use of imaging modalities for pleural lymphoma
Chest X-rays and CT scans
Usually, a chest X-ray is the initial diagnostic procedure undertaken. Pleural lymphoma could present with a malignant pleural effusion, thickening of the pleura, and rarely a discrete nodule. The thickening of the pleura could be circumferential and present at the posterior aspect of the chest. Usually these findings are not accompanied by mediastinal lymphadenopathy. A rather specific finding observed in pleural lymphoma is the pleural sandwich sign, which is composed of a thin, highly enhanced central segment comprising mesenteric vessels, which is surrounded by enlarged pleural lymph nodes [6]. Although CT scans are considered the most helpful imaging technique in guiding the diagnosis of pleural lymphoma, the mentioned findings are not specific and other conditions such as bronchogenic cancers, metastasis, infections, chronic inflammatory processes, organising pneumonia, sarcoidosis, and lymphangitic carcinomas may have similar findings, making biopsy necessary for the diagnosis [7].
PET/CT scan
As mentioned, multiple benign lesions are listed as differential diagnosis of pleural lymphoma. PET scan is a suitable method to distinguish benign pleural lesions such as solitary fibrous lesions, lipomatous tumours, and adenomatoid tumours. Furthermore, it is an ideal tool to investigate individuals with no risk factor for pleural malignancies and cases with no obvious clinical diagnosis. Patil et al. reported the beneficence of PET/CT scan in detecting primary effusion lymphoma (PEL)-like lymphoma of the pericardium. PET scan revealed increased uptake in the pericardium, pleura, and the abdominal cavity, suggesting the presence of a primary pathology of the aforementioned locations and their serous linings [8]. Lee et al. reported another case in which PET scan was instrumental for the diagnosis. In this case report, PET scan was used to diagnose the relapse of a primary pleural lymphoma, which had manifested as a case of dermatomyositis [9]. PET scan was able to show the increased uptake of radiotracers in anatomical sites involved with dermatomyositis, and a nodular lesion with high uptake in the supraclavicular and retroperitoneal spaces.
Ultrasonography
Ultrasonography is the preferred method for the examination of pleural effusions because it is widely available (compared to CT-scans) and can detect small amounts of fluid in the pleural cavity. Ultrasonography is also a suitable method for the study of pleural lesions because it can detect masses in the pleura by their different echogenic characteristics. This imaging modality can also show signs of chronic inflammation in the pleura, such as fibrous bands and septa with encapsulated liquid, and is efficient in differentiating long-standing pleural effusion and thickening in pneumonia with malignant conditions such as primary lymphoma of the pleura or metastatic tumours. Ultrasonography may be useful in detecting lesions of the chest wall and differentiating them from lesions of the pleura. This is important because many chest wall lesions present with chronic pain in the thoracic region, a common finding in malignancies of the pleura [10].
Ultrasonography is also a suitable method for guiding biopsies of the pleura and can have important diagnostic implications in patients even after CT scans have been performed [11].
Conclusions
Pleural lymphoma is a rare presentation of lymphoma. This condition is usually seen in older men with risk factors such as smoking, previous tuberculosis infection, and contact with asbestosis. In this case report we describe a child with pleural lymphoma, which was not associated with any risk factor. Pathological examination showed that the lymphoma was of T-cell origin, in contrast to most cases, which are of DLBCL origin. This patient was treated with the BFM-NHL protocol and remained disease free in three years of follow-up. Medical imaging techniques are the first line of any paraclinical examination series, and they guide further diagnostic and therapeutic actions.