Introduction
Seven years after the MERS epidemic in the world, a new disease has been identified in China that has been announced as an international emergency worldwide by the World Health Organization (WHO) [1]. Although China was originally the center of the disease, the virus quickly spread to many parts of the world, leading to tremendous mortality [2]. This novel virus belongs to the coronavirus family causing flu-like symptoms as well as SARS and MERS. The most important forms of transmission are droplets and physical contact [3]. On February 11, 2020, the WHO named the new virus coronavirus disease 2019 (COVID-19) [4]. The clinical manifestation of the disease include fever, cough and dyspnea representing pneumonia, acute respiratory syndrome and death in severe disease [5]. The risk factors of infection include diabetes mellitus, hypertension, and cardiovascular disease [6,7]. The number of COVID-19 patients is still rising, with 22,524,291 infected worldwide on April 22, 2020 [8].
The gold standard test for the disease is known as real-time polymerase chain reaction (RT-PCR) assay, but false-negative results may be reported due to the low viral load of samples and manner of sampling. On the other hand, the chest computed tomography (CT) scan is employed as an important diagnostic supplement to verify the COVID-19 disease [9]. The advantages of this method are being more time-saving than RT-PCR [10], and high sensitivity (97%) in early diagnosis [11-13]. Nevertheless, positive RT-PCR may occur in normal chest CT in COVID-19 patients [14]. Furthermore, the chest CT scans of COVID-19 patients have shown low positive predictive value [15].
According to the rapid spread of the disease and the importance of preventing and controlling COVID-19, the primary diagnosis is crucial. This study was conducted to compare between CT scan and RT-PCR test in patients suspected to have COVID-19 infection. Sensitivity and specificity of CT scan were also evaluated based on RT-PCR.
Material and methods
This study was a cross sectional design on patients with COVID-19 admitted to Vali-e-Asr Fasa Hospital. Sensitivity and specificity of the chest CT scan, and oropharyngeal and nasopharyngeal RT-PCR were considered in 54 suspected COVID-19 patients. Demographic information including sex and age was also collected. Chest CT scan results were categorized as ground-glass, consolidation and normal. Cohen’s kappa coefficient was considered for RT-PCR and CT scan.
Results
Of 54 patients, 27 (50%) were female and half were male, with the mean age range of 51.75 ± 18.63.
RT-PCR assay was carried out on the 54 suspected COVID-19 patients with the subsequent result of 23 (42.6%) negative and 31 (57.4%) positive cases.
The patients with an abnormal chest CT scan comprised 37 (68.5%), while normal chest CT results were obtained in 17 (31.5%) of the patients. 23/54 (42.6%) patients showed ground-glass opacity (GGO), while 28/54 (51.85%) cases were with consolidation opacities. Patients demonstrating both GGO and consolidation opacities comprised 13/54 (24.1%) in chest CT scan.
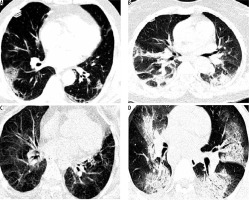
The sensitivity and specificity of chest CT scan based on the RT-PCR test (as a gold standard) for COVID-19 are presented in Table 1. The sensitivity and specificity of abnormal CT scan were 78.6% and 42.3%, respectively, based on the RT-PCR method. In the cases with GGO, the sensitivity and specificity of CT scan were calculated as 67.9% and 53.8% respectively, whilst CT scan findings of consolidated lungs showed 35.7% sensitivity and 65.4% specificity based on RT-PCR. These amounts were 53.8% sensitivity and 64.7% specificity for the simulations of GGO and consolidation opacities in suspected COVID-19 patients. CT scan images according to PCR findings are presented in Figure 1.
Table 1
Results of real-time polymerase chain reaction (RT-PCR), chest computed tomography (CT) scan and also sensitivity and specificity of chest CT scan based on RT-PCR test are presented for diagnosis of COVID-19
Discussion
Analyzed data of 54 (f = m) suspected COVID-19 patients, 42.6% (n = 23) showed GGO on chest CT; 57.4% (n = 31) had consolidation, 24.1% had both and only 16.6% had normal chest CT findings. 87.4% of the suspected cases tested positive in RT-PCR, reporting as the principal and accepted method in diagnosing COVID-19.
Our data on sensitivity and specificity of ground glass opacity showed 67.9% and 53.8% respectively (k = 0.218). For chest CT with only consolidation, the sensitivity was 35.7% with the specificity of 65.4% (k = 0.11), and for the both GGO and consolidation the sensitivity and specificity were found to be 53.8% and 64.7% respectively in diagnosing COVID-19, based on RT-PCR.
Data on the correlation of chest CT and RT-PCR in COVID-19 diagnosis are located at the two extremes. Some studies, especially those from the radiology community, support a pivotal role for chest CT in diagnosing COVID-19. A report of 1014 patients from China proposed 97% sensitivity and specificity of 25% of CT scans based on RT-PCR results [11]. Another study from Wuhan, China, tried to determine the misdiagnosis rate of chest CT; among 51 confirmed cases of COVID-19, 3.9% were found to be missed diagnoses. They suggested the use of chest CT as the standard method for screening and diagnosis of the disease [16]. Predominant findings in the CT scan of suspected patients were ground glass opacities and consolidation, local and bilateral patchy shadowing, and also crazy-paving patterns detected and associated with the disease [17-19].
In the extremely progressive outbreak of the COVID-19 pandemic, an accessible, accurate, sensitive, and specific diagnostic method is crucial. However, the RT-PCR kits, despite their high specificity and acceptable sensitivity, are not accessible worldwide. Chest CT scans, based on promising reports mostly from China, have been advocated, but are criticized. It is suggested that the CT findings of COVID-19 lack sufficient specificity to the disease, and they have been seen in a variety of infectious and noninfectious conditions. High specificity reports of CT scan in China may be due to the high incidence, while they are likely to be different in other regions with a lower incidence of the disease. Meanwhile, in seasonal flu (ground glass opacity and consolidation as chest patterns of diagnosis as well as H1N1 influenza, MERS, and SARS), the sensitivity of the chest CT scan would not be accurate enough. However, the criticizers also reported some scientific flaws in the previous discussed articles. The American College of Radiology and the Centers for Disease Control do not currently suggest chest CT for diagnosis of COVID-19 [20-22].
We suggest that a proper diagnosis of COVID-19 should be based on a mixture of clinical manifestation, nucleotide viral testing, history of contact and occupational and social exposure. Other techniques alongside CT scan and RT-PCR are also advocated for accuracy of the disease diagnosis. Moreover, considering the low diagnostic value of the chest CT scan may help the health care providers to determine the severity and course of the disease.