Introduction
Acute superior mesenteric artery (SMA) occlusion is the most common cause of acute mesenteric ischaemia, which is a life-threatening condition with a potentially high mortality rate [1]. Although the overall survival has been increasing in recent years, approximately 63% of patients with SMA occlusion do not survive [2]. According to European guidelines, endovascular therapy (EVT) in most cases should be the initial approach before any bowel surgery [3]. Compared to open surgery, EVT presents lower inpatient mortality and overall morbidity [4]. The aim of this study is to retrospectively evaluate single-centre experience in EVT of acute SMA occlusion by assessing technical success and mortality as well as its dependence on the level and aetiology of occlusion.
Material and methods
Study design and patients
This study analysed medical data retrieved from the procedural databases and hospital registry of patients who presented to our centre from January 2018 to December 2020 with acute abdomen and diagnosed with acute thromboembolic SMA occlusion. We did not include patients with chronic, non-occlusive, venous mesenteric ischae-mia and other rare causes of acute mesenteric ischae-mia. The clinical diagnosis of acute SMA occlusion was established by triphasic contrast-enhanced computed tomography (CT) with a slice thickness of 1-1.25 mm.
This retrospective observational analytical study was approved by the local Ethics Committee (protocol No. BEC-MF-209).
Treatment approaches
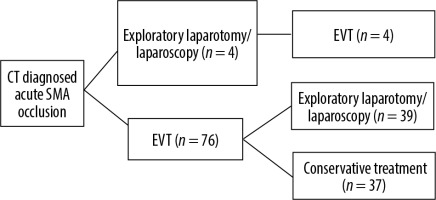
After computed tomography angiography (CTA) established the diagnosis of acute SMA occlusion some patients, due to advanced peritonitis, subsequently had a primary exploratory laparotomy and EVT (n = 4). Stable patients were primarily submitted straight to EVT (n = 76). In cases of unimproved clinical condition after the primary EVT, exploratory laparotomy (n = 38) or diagnostic laparoscopy (n = 1) was performed (Figure 1). Some cases required multiple exploratory laparotomies (n = 13) and/or resection of unviable bowel (n = 10).
Endovascular techniques
In all cases, if an occlusion site could be reached with an aspiration catheter, a primary aspiration thrombectomy was performed. In those cases, where the blood flow was not fully restored, additional percutaneous transluminal angioplasty (PTA)/stenting was performed. In cases where the site of obstruction could not be reached with the aspiration catheter, PTA/stenting was performed as a primary EVT method.
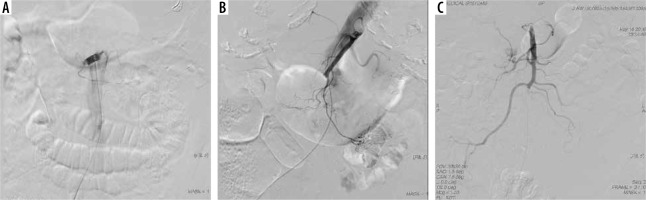
In all cases femoral access was used. Mechanical aspiration thrombectomy was performed as follows (Figure 2): a Destination 7F angled guiding sheath (Terumo Corporation, Tokyo, Japan) was placed in the aorta. And over the 5F C2 (or similar shape) diagnostic catheter Imager II (Boston Scientific Corporation, Marlborough, USA) and 0.035-inch hydrophilic steerable guide wire (Terumo Corporation, Tokyo, Japan) the sheath was inserted into the main stem of the SMA as far as possible. Manual aspiration using a 60-ml syringe (VacLok®, Merit Medical Systems, South Jordan, USA) was started through the sheath if the thrombus could be reached. The aspiration was then continued through flexible angled 6F aspiration catheters – FARGOMAX MP (Balt Extrusion, Montmorency, France) or Chaperon (Microvention, Tuslin, USA) – inserted into the large branches over the steerable guide wire. The cathe-ter was withdrawn under continuous suction and flushed. Several passes through the occluded stem and branches were necessary to restore the vascular patency. In cases of failure to restore blood flow to the SMA stem or when there was residual stenosis/thrombus, the revascularisation procedure was continued as “bail out” PTA. Balloon angioplasty was performed over the 0.035-inch wire with an Armada 35 peripheral balloon (Abbott Vascular, Santa Clara CA, USA) of size equal to the artery. In cases of postangioplasty adequate flow and less than 40% residual stenosis, stenting was not considered. In cases with an unacceptable postangioplasty result stenting was considered. An ISTHMUS balloon-expandable stent (CID S.p.A., Saluggia, Italy) was used for proximal short lesions, and an Epic self-expandable stent (Boston Scientific Corporation, Marlborough, USA) was used in long, distally located lesions.
Figure 2
A 90-year-old female suffering from abdominal pain, emesis, and haematochezia for less than 12 hours. Abdominal computed tomography angiography revealed an occlusion of the superior mesenteric artery (SMA). A) Digital subtraction angiography confirmed a proximal embolic occlusion of the SMA. B) Mechanical aspiration using a 6F catheter through a distally placed 7F guiding sheath. C) After a few passes the flow in the main stem and all large branches was restored
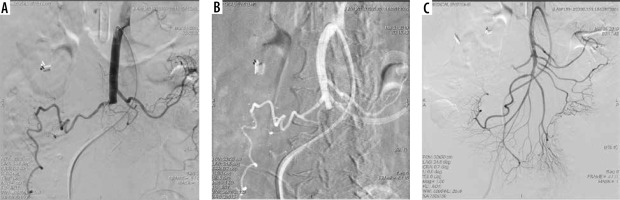
Primary PTA/stenting was performed in cases where critical ostial SMA sub-occlusion was found (Figure 3). The lesion was passed with a 0.014-inch guide wire. The angl-ed 7F guiding sheath was used for support in the ostium of SMA. Pre-dilatation was usually performed with an under-sized PTCA balloon (Powerline, Biosensors Europe SA, Morges, Switzerland). A RADIX2 balloon-expandable stent (CID S.p.A., Saluggia, Italy) was used for ostial/proximal short lesions.
Figure 3
A 76-year-old female with abdominal pain ongoing for over 24 hours. A) Computed tomography angiography 3D reconstruction showing a sub-occlusion of the superior mesenteric artery (SMA). B) Digital subtraction angiography confirmed a critical ostial SMA stenosis. C) Pre-dilatation of the lesion with an under-sized balloon was performed. D) Final result after stenting with a balloon-expandable stent
Procedures were performed under anticoagulation (5000 I.U. of heparin IA) with IV administration of heparin (1000 IU/h) for 24 hours after the procedure. Dual anti-platelet therapy with clopidogrel 75 mg/day for 6 weeks and aspirin 100 mg/day lifelong was recommended. All patients also received a loading dose of 300 mg clopidogrel immediately after the endovascular procedure, except for those patients who were transferred to the ope-rating room, because the clopidogrel loading dose was withheld until after surgery in these patients.
Classification of the level of occlusion
Based on the findings of computed tomography angiography (CTA) and digital subtraction angiography (DSA), we classified all of the cases by the number of SMA large branches that remained non-occluded and continued to provide perfusion to the bowel: ostial occlusion (0 patent branches), proximal occlusion (1, 2, or 3 patent branches – most commonly inferior pancreaticoduodenal, middle colic, and jejunal arteries), and distal occlusion (4, 5, or 6 patent branches – most frequently additionally ileal, right colic, and ileocolic arteries) (Figure 4). The idea of this classification was to determine whether the proximality of the occlusion has an impact on the selection of endovascular technique, and the technical and clinical results of the EVT procedure.
Classification of the aetiology of occlusion
Based on the findings of CTA and DSA, we classified the aetiology of the occlusion into thrombosis and embolism. Thrombotic aetiology was defined as ostial/proximal SMA and/or nearby aorta calcification on non-contrast CT and stenosis with adjacent thrombus on CTA and DSA. Embolism was determined where non-calcified ostium, poor or absent collateral circulation, and round/oval clot surrounded by contrast material or filling defect with an abrupt cut-off was observed.
In all cases where thrombectomy was the primary and only EVT method, the occlusion was due to embolism. Conversely, where the occlusion was due to atherosclerosis, the primary and only EVT method was PTA/stenting.
Measures of outcome
Restored flow to the SMA stem and all the large branches was considered to be a technical success. Residual occlusion in small distal branches was tolerated. Restored stem flow with at least one large, occluded branch was assumed as a partial success. Ultimately, failure to restore blood flow in the SMA stem was defined as a failure.
Mortality was defined as intrahospital mortality. For a more thorough comparison with other studies, 30-day-mortality was also calculated.
Perioperative complications directly associated with EVT, which prolonged hospital stay, caused a technical failure, and/or affected overall clinical outcome were recorded.
Statistical analysis
Data analysis was performed using SPSS Statistics 28.0. Nominal data were compared using Fisher’s exact test or Pearson’s c2 test. The Mann-Whitney U test, Kruskal-Wallis H test, and Spearman’s rank correlation were used for nonparametric data. P-values < 0.05 were considered as statistically significant.
Results
Demographic data
During a period of 3 years, EVT for acute SMA occlusion was performed on 80 patients. Their median age was 81 years (IQR 75-86). There were 35 (43.8%) males and 45 (56.3%) females. Most patients (86.1%) had comorbidity: arterial hyper-tension (57.0%) and atrial fibrillation (54.4%) were the most common. Out of 43 patients with atrial fibrillation, only 16 (37.2%) affirmed to have been taking anticoagulants regularly. All the patients were presented with abdominal pain (n = 80; 100%), and many of them had nausea/emesis (n = 33; 42.9%). The interval from the onset of the symptoms to EVT varied greatly, and in many cases it was impossible to determine the exact interval; therefore, we defined 3 groups: up to 12 hours (29.9%), from 12 to 24 hours (14.3%), and beyond 24 hours (55.8%) from the onset of symptoms. 65.0% (n = 52) of patients were transferred from another city/hospital. After clinical examination, 64.9% had signs of peritoneal irritation. Arterial lactate concentration (mmol/l) was documented in only 34 cases, and its median was 2.55 (IQR 1.60-5.25) (Table 1).
Table 1
Demographic data
It was noted that males (median age: 79 years) were significantly younger than females (median age: 83 years) (U = 512.0; p = 0.007). Females more often than males had ischaemic heart disease (c2 = 5.27; p = 0.022; OR = 5.5 [95% CI: 1.13-26.76]) and presented with diarrhoea (c2 = 4.51; p = 0.034; OR = 7.54 [95% CI: 0.89-63.63]). Also, females spent fewer bed-days (median = 6) in hospital than males (median = 11) (U = 522.5; p = 0.010).
CTA and DSA findings
When analysing DSA and CTA findings, thrombotic aetio-logy was identified in 20 (25.0%) and embolic aetiology in 60 (75.0%) patients. We noticed a tendency that thrombosis appeared more frequently in males, while embolism was more frequent in females (OR = 2.41 [95% CI: 0.86-6.79]), but these results were not statistically significant (p = 0.091). Patients with thrombosis were statistically significantly younger (median = 78; IQR = 67.50-82.00), while patients with embolism were older (median = 82; IQR = 77.00-86.75; U = 417.00; p = 0.042). Embolism was also associated with higher arterial lactate levels (median = 3.10), while thrombosis was more frequent with lower arterial lactate (median = 1.68; p = 0.034). The duration between the onset of symptoms to EVT procedure was longer for patients with thrombotic occlusion, and vice versa (p = 0.006). According to CTA and DSA findings, we defined the quantity of residual non-occluded large branches of the SMA and classified all cases into 3 occlusion types: ostial occlusion (0 patent branches) (n = 19; 23.8%), proximal occlusion (1-3 patent branches) (n = 38; 47.5%), and distal occlusion (4-6 patent branches) (n = 23; 28.7%). Thrombosis was associated with more proximal (less patent large branches) occlusion, while embolism was associated with more distal (more patent branches) occlusion (p < 0.001).
Endovascular treatment
Mechanical thrombus aspiration was the chosen primary technique in 87.5% (n = 70) of cases. Out of those, 23 cases required a secondary PTA/stenting approach. In other cases (n = 10; 12.5%) PTA/stenting was the primary and only method (Table 2).
Table 2
Endovascular techniques used and technical success evaluation
Mechanical thrombectomy was performed statistically significantly more frequently, when more non-occluded large branches were present, whereas PTA/stenting was performed in cases with fewer intact large branches (H = 15.49; p < 0.001). Also, mechanical thrombectomy was more often performed when the period between the onset of the symptoms and EVT was shorter, and PTA/stenting was more frequently performed in cases where the period of time between the onset of the symptoms and EVT was longer (H = 6.40; p = 0.038).
67.5% of cases (n=54) were technically successful, 12.5% (n = 10) were partially successful, and 20.0% (n = 16) were a technical failure. EVT technical success did not statistically depend on the type of endovascular technique (H = 3.48; p = 0.175), the aetiology (U = 552.0; p = 0.519), or the type (number of patent large branches) of occlusion (δ = –0.05; p = 0.653). However, technical success statistically significantly depended on the arterial lactate concentration (δ = 0.47; p = 0.005): a lower arterial lactate level at the time of presentation indicated a higher probability of a successful procedure, and vice versa.
There was tendency for mechanical thrombus aspiration to be followed by subsequent PTA/stenting more frequently in cases of a technical failure (n = 7/15; 46.7%) compared to technically successful and partially successful cases (n = 16/55; 29.1%; p = 0.199).
Mortality rates
Despite the endovascular, surgical, and conservative treatment, the intrahospital mortality was 58.8%. The median number of days from EVT to death was 2 (IQR 1-8). We also evaluated overall the 30-day mortality rate after EVT to be 55.0%.
Patient’s age (p = 0.258), comorbidity (p = 0.512), the time from the onset of symptoms to EVT (p = 0.242), aetiology of occlusion (p = 0.359), and EVT technique (p = 0.273) had no statistical significance on intrahospital mortality.
Intrahospital mortality significantly depended on EVT technical success. The more successful the EVT, the lower the mortality rate (U = 532.50; p = 0.004). 87.5% of cases of EVT failure ended fatally, and even when the procedure was successful, almost half (48.1%) of the patients did not survive (Table 3).
Table 3
Intrahospital mortality based on endovascular therapy (EVT) technical success
| Variable | Intrahospital mortality, n (%) | |
|---|---|---|
| All cases (n = 80) | 47 (58.8) | |
| EVT technical success | ||
| Success (n = 54) | 26 (48.1) | |
| Partial success (n = 10) | 7 (70.0) | |
| Failure (n = 16) | 14 (87.5) | |
It was discovered that in the EVT failure group, the final clinical outcome depended significantly on the quantity of undamaged large branches of the SMA. Fewer non-occluded large branches meant more fatal cases, and vice versa: more undamaged large branches were related to lower intrahospital mortality (U = 2.00; p = 0.041). This did not apply to groups of technical success (p = 0.572) and partial success (p = 0.285) or in overall intrahospital mortality (p = 0.447).
Even though arterial lactate data were available from only 34 cases, it showed statistical significance in intrahospital mortality: the higher the level of arterial lactate, the higher the intrahospital mortality (U = 38.00; p < 0.001). Also, the same tendency applied in cases where an EVT was technically successful (n = 22; p = 0.002). However, there was no statistical significance in cases where partial success (n = 4; p = 0.439) or failure (n = 8; p = 0.739) was observed.
Complications
There were 2 serious complications in our study related to EVT (total complication rate 2.5%): one case of inguinal haematoma, which was successfully treated conservatively, but it prolonged the patient’s hospital stay; and one case of perforated left common iliac artery. The latter evolved from a problematic access to the SMA and caused a massive bleeding. The bleeding was managed by stent implantation. No objective data indicated further bleeding. Eventually, due to unspecified shock, the patient died on the same day.
Discussion
Main points
Mortality rates of acute SMA occlusion remain high. Successful endovascular reperfusion seems to reasonably improve the patients’ clinical outcome. In the case of EVT failure, the quantity of non-occluded large SMA branches may be clinically significant, because fewer patent branches seems to raise the mortality rates even higher. EVT technical success seems not to be influenced by aetiology or by level of occlusion.
We established that higher arterial lactate concentration may act adversely on EVT technical success and intrahospital mortality. However, the data for this finding were only available from 34 cases; thus, potential prognostic significance should be assessed carefully.
Our study did not find the time from the onset of symptoms to EVT to be clinically important, but this might be misleading because the exact time of onset was unknown in many cases.
Failures
Overall, in our study there were 16 cases (20%) that were technically unsuccessful. It means that during those procedures no flow improvement was achieved and/or the main stem of the SMA remained occluded. In 5 of those cases the reason for failure was proximal occlusion of the SMA opening, which made access to the SMA extremely difficult and in these cases unfortunate. In another 7 cases EVT failed due to long thromboembolic segments of the artery, which in some cases were old and organised thrombi. Because no stable flow could be achieved, revascularisation in these cases proved to be only temporary. In 4 cases atypical vascular anatomy was mainly responsible for a failed procedure. Arterial tortuosity and inconveniently angled origin of the SMA were observed. These anatomical features impeded the access and endovascular manipulation, which eventually led to technical failures. It should be recognised that in some of these cases brachial or radial access as well as usage of a steerable sheath could have potentially granted access to the occlusion site, thus improving the outcome of the procedure. Moreover, a tendency for subsequently exploiting PTA/stenting after mechanical thrombectomy in cases of technical failure indicates the necessity of additional endovascular measures in cases of complex SMA occlusion and/or difficult vascular anatomy. These measures may also include additional mechanical thrombectomy devices, such as Aspirex or Angiojet for long occluded segments and/or massive thrombi. Furthermore, in the case of an EVT failure and the bowel being sufficiently viable, surgical thrombectomy or aorto-mesenteric bypass might be a possible revascularisation option.
Comparison with similar studies
To compare our study results to other studies we searched for similar articles in the PubMed database, published in the last 10 years, in English language. The search keywords were “endovascular treatment and acute superior mesenteric artery occlusion”. The search results provided 114 results. We excluded articles about chronic mesenteric ischaemia, review articles, articles about surgical approach, single case reports, retrograde open mesenteric stenting (ROMS) procedures, and articles with less than 20 patients in the study. Finally, there were 5 articles that matched our criteria [5-9].
We compared our study to other similar studies about the endovascular treatment of acute SMA occlusion; the results are shown in Table 4. When comparing the numbers of patients included in the studies (ranged from 21 to 50), our study appeared to have the most patients (n = 80). Moreover, the median age of the patients in other studies varied from 70 to 79 years, while in our study the median age was 81 years. Atrial fibrillation is one of the most common comorbidities, it ranged from 38% to 71%, and in our study it was similar to others (54%). Hypertension is also very common between patients with SMA occlusion, ranging from 68% to 80%, while between the patients of our study hypertension was diagnosed in 57%. The most frequent symptom among all studies was abdominal pain. Ostial and proximal SMA occlusion as well as embolic aetio-logy occurred the most often in all the studies. In terms of EVT method, mechanical thrombectomy was the most commonly used in almost all the studies, while PTA/stenting was more of a complementary approach. However, in the study by Pedersoli et al. [8], in which the level of occlusion in all cases was within the proximal 4 cm of the artery, the only EVT technique used was PTA/stenting. Our EVT technical success as well as the need for subsequent laparotomy/laparoscopy was similar to other studies.
Table 4
Comparison with other similar studies
| Author | Year | Number of patients | Median age (years) | Comorbidities | Symptoms | Duration from onset of symptoms to intervention | Level of occlusion | Aetiology | 30-day mortality | Intrahospital mortality | Treatment tactics | Technical success | Subsequent laparotomy/laparoscopy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jia [6] | 2014 | 21 | 71 | AF 71% | AP 100%, ATR 14% | < 18 h 100%, median 9 h | Main trunk occlusion 81%, branch occlusion 19% | – | 10% | – | MT 33%, MT+THR 62%, MT+THR+STENT 5% | Success 29%, partial success 71% | 24% |
| Kar¨kkaïnenn [8] | 2015 | 50 | 79 | AH 68%, CAD 52%, AF 38%, PAD 38%, DM 34%, STR/TIA 30%, MI 14%, CRI 4% | AP 94%, EM 56%,DIAR 48%,AD 26%,IL 20%,GIB 14% | < 24 h 38%, 1-3 days 32%, > 3 days 36% | – | Embolism 64%, thrombosis 36% | 32% | – | MT 40% (adj. THR 8%, adj. STENT 6%), PTA/STENT 60% | Success 88%, failure 12% | 40% |
| Raupach [7] | 2016 | 37 | 76 | AH 73%, AF 70%, DM 46%, CHF 32%,MI 27%, COPD 14% | AP 97%, NAU/EM 62%, DIAR 35%, BD 30% | Median 24 h | – | Embolism 100% | – | 27% | MT 100% (adj. THR 5%, adj. STENT 5%) | Success 92%, failure 8% | 73% |
| Freitas [9] | 2018 | 20 | 70 | AH 80%, AR/AF 60%, DM 35%, CAD 30%, RI 15%, OB 15%, CD 10% | AP 65%, IL 35%, SE 25% | – | Aortic ostium 30%, proximal to middle colic artery (MCA) 35%, distal to MCA 20%, peripheral branches 15% | – | 40% | – | MT 100% (adj. PTA 35%, adj. STENT 25%), THR 20% (adj. MT 10%) | Success 100% | 70% |
| Pedersoli [5]* | 2021 | 40* | – | – | – | – | 100% within the proximal 4 cm of coeliac artery (CA) or SMA* | Thrombosis 100%* | 63%* | – | PTA/STENT 100%* | Success 90%* | 63%* |
| Our study | 2021 | 80 | 81 | AH 57%, AF 54%, STR 23%, CAD 17%,CHF 15%, DM 13%, MI 6% | AP 100%, NAU 43%, EM 38%, DIAR 12%, HC 5% | < 12 h 30%, 12-24 h 14%, > 24 h 56% | Ostial occlusion (0 patent branches) 24%, proximal occlusion (1-3 patent branches) 47%, distal occlusion (4-6 patent branches) 29% | Embolism 75%, thrombosis 25% | 55% | 59% | MT 59%, MT+PTA/STENT 29%, PTA/STENT 12% | Success 68%, partial success 12%, failure 20% | 49% |
* Results for the Pedersoli study [5] were calculated for the cohort of patients with occlusion of the CA and/or SMA. AF – atrial fibrillation, AH – arterial hypertension, CAD – coronary artery disease, PAD – peripheral arterial disease, DM – diabetes mellitus, STR – stroke, TIA – transitory ischaemic attack, MI – previous myocardial infarction, CRI – chronic renal insufficiency, CHF – chronic heart failure, COPD - chronic obstructive pulmonary disease, AR – arrhythmia, RI – renal impairment, OB – obesity, CD – cerebrovascular disease, AP – abdominal pain, ATR – abdominal tenderness and rebound, DIAR – diarrhoea, AD – abdominal distention, IL – ileus, GIB – gastrointestinal bleeding, NAU – nausea, EM – emesis, BD – bloody diarrhoea, SE – sepsis, HC – haematochezia, MT – mechanical thrombectomy, THR – thrombolysis, adj. – adjunctive, STENT – stenting
When comparing mortality rates, ours were higher than in most other centres. However, we believe this was mainly due to a few key differences between the studies. Our study represented a real-world population and included all comers by combining 2 main aetiologies of occlusion (thrombosis and embolism) with different clinical evolution; therefore, this might limit an accurate comparison to other similar studies. A few other studies were conducted with specific populations. Comparing to the study by Jia et al. [6], most of our cases took a distinctly longer period of time from the onset of symptoms to the treatment. Regarding the aetiology of the occlusion, it differed massively from Raupach et al. [7] and Pedersoli et al. [8]. Most importantly, our patients were considerably older than in all other studies. Also, most of our patients with atrial fibrillation had not received adequate anticoagulation therapy prior to presentation.
From our perspective, there are a few areas that may potentially improve the clinical outcomes of our future patients. We believe that by performing PTA/stenting more frequently and exploiting brachial/radial access more actively in difficult cases, we may slightly improve the EVT technical success rate. Also, we intend to utilize arterial lactate measurement more often due to its potential prognostic possibilities.
Conclusions
This study contributes to research on acute SMA occlusion. Despite adequate EVT technical success rates and successful endovascular reperfusion appearing to reduce fatal outcomes, the mortality rate of this condition remains extremely high. While the occlusion level appears to have no influence on EVT technical success rates, it is a potentially useful prognostic factor in cases of failed recanalization. The aetiology of the occlusion seems to have no impact on technical success or mortality.