Introduction
Endovascular procedures have become standard practise for many cardio-vascular diseases in recent years [1,2]. Procedures such as endovascular aneurysm repair (EVAR), thoracic endovascular aneurysm repair (TEVAR), or transcatheter aortic valve implantation (TAVI) have become an alternative for surgical operations [1,2]. The importance of all these methods is increasing because of less patient injury. In addition, endovascular procedures allow the use of local anaesthesia or shortened general anaesthesia, which can be essential in patients with co-morbidities.
During endovascular procedures like EVAR or TAVI, there is a need to use large-bore sheath devices with a dia-meter up to 24F ID (8 mm) [3,4]. Classical vascular access for the mentioned procedures is surgical cutdown in groins. After preparation of the artery, a large sheath is inserted into the artery and the treatment is performed. At the end of the operation, the access site is sutured by the surgeon.
Percutaneous access is an alternative method that can be used during EVAR, TEVAR, or TAVI. There are 2 possibilities of closure of the large-bore access site percutaneously. Both fascia suture technique and vascular closure devices can be used [5]. A more common method is percutaneous access with suture-mediated closure devices, especially the Perclose Proglide (Abbott Vascular, Santa Clara, CA, USA) preclosure technique [6-9].
Following the instruction of use of this device, it can be used even in large-bore access sites [10]. In the study group, different access sites sizes, from 12F to 22F, were evaluated. According to previous studies, opinions vary on the relationship between the size of the sheath used in the procedure and the complication rate [11-15].
The aim of the study was to assess correlation between size of the arterial access site and the complication rate. The second goal was an evaluation of the effectiveness of haemostasis with a Perclose Proglide closure device after percutaneous procedure with a large arterial access site. The study assessed the complication rate and type related to this technique.
Material and methods
Group
There were 202 patients (162 male and 40 female, median age 73.5 years) with abdominal aortic aneurysm (AAA) included in the study, who were treated percutaneously from 2013 to 2017 in the authors’ hospital. Percutaneous EVAR was performed in all these patients with 384 large-sheath access sites, from 12F to 22F in diameter. Patients were qualified to percutaneous stentgraft implantation after evaluation of computed tomography angiography (CTA) of the abdomen and pelvis. The exclusion criteria were occlusion of the common femoral artery, massive calcified atherosclerotic plaques in common femoral arteries, and history of groin surgery.
Procedure
In all cases at least one large-bore arterial access site was performed percutaneously using a modified Seldinger method without posterior wall puncture. The closure system in all cases was the Perclose Proglide. According to the instructions for use of the Perclose Proglide, it is necessary to use 2 devices per access site in the preclosure technique [10]. Once the initial 5F introducer sheath was in the artery, 2 closure devices per vascular access were implanted with the sutures left undone. Afterwards, percutaneous implantation of an aortic stentgraft to the aneurysm was performed. At the end of the procedure, during large sheath removal, both Perclose Proglide sutures previously left undone were tied up. In cases without effective haemostasis an additional Perclose Proglide device was applied. The treatment was confirmed as successful in cases where haemostasis was achieved. Treatment was categorised as unsuccessful in cases without haemostasis after deployment of a third closure device. Conversion to surgical repair was applied in such cases.
Post-operative assessment
The post-operative management was carried out routinely, just like the assessment of the standard patient, who underwent EVAR in the authors’ Institution.
The post-operative assessment included early complications that occurred during the hospitalization and late complications.
During hospitalization, haemostasis, presence of pseudoaneurysm or well-defined haematomas, and signs of acute lower limb ischaemia were evaluated.
Post-hospital assessment included clinical observation in 1-3 months where once again the presence of pseudoaneurysm or haematoma in groins were investigated. In addition, the presence of acute lower limb ischaemia or exacerbation of chronic limb ischaemia were evaluated.
The last examination was follow-up CTA after 6 months. The CTA was carried out as control of aortic aneurysm, presence of endoleak to the aneurysm sac, integrity and location of stentgraft, patency of stentgraft, and visceral and access arteries. CTA protocol included the range from the diaphragm to lesser trochanter of the femur.
In this study evaluation of femoral artery stenosis was taken into consideration. Pre-procedure and post-procedure CTAs were compared, and a reduction of 50% or more in cross-sectional flow area between both CTAs was considered significant. In the study, all found stenoses were stated to be post-procedural complications.
The main aim of the study was to evaluate the vascular access site and the presence of related complications. Other information such as the presence of endoleak to aneurysm sac, aneurysm diameter, and stentgraft information were not included because they were considered not to be dependant on vascular access type.
Statistical analysis
The qualitative variables were characterized by providing the number of observations for each category and the corresponding percentage (structure index). The data has been summarized in tables and presented by means of graphs.
The c2 independence test was used to test the independence of the variables with regard to the qualitative variables. The Fisher-Freeman-Halton test was used when Cochran’s assumptions were not met, especially in correlation between access diameter and a lack of haemostasis.
Results
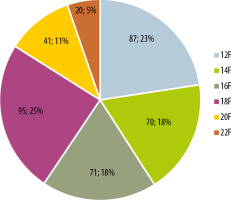
From January 2014 to December 2017, 202 patients (162 male and 40 female, median age 73.5 years, range 55-90 years), were underwent percutaneous endovascular aortic repair (pEVAR). Percutaneous implantation of a stentgraft was performed in each patient after exclusion of contraindications to this treatment. In most cases (n =182), bilateral femoral percutaneous access was performed. In 20 patients, percutaneous access was performed unilaterally. In 14 cases, unilateral percutaneous access was performed due to impossibility of a bilateral percutaneous approach, because of one-sided massive calcifications, recent surgery, or occlusion. In these patients, second access was achieved surgically. In 6 cases unilateral percutaneous access was caused by the chosen treatment method, which demanded only one large-bore access site. The total number of performed large-bore vascular accesses was 384. The diameter (ID) of each one is shown in Figure 1.
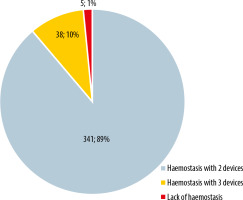
Haemostasis was achieved in 379 vascular accesses (98% of all). In 341 cases, the procedure was effective using 2 closure devices. In 38 cases (10%), it was necessary to use an additional, third closure device. In 5 percutaneous vascular approaches (1.5%), haemostasis was not achieved with Perclose Proglide devices and the conversion to surgical repair was performed. Figure 2 presents the structure of the group considering haemostasis achievement.
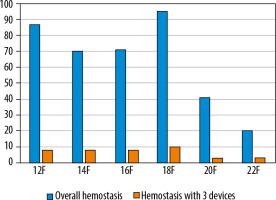
Large-bore vascular access was successfully closed with 2 closure devices in 88.8% of cases. For most of the used sheath diameters, the percentage of efficient haemostasis was 88-93% (Table 1). However, the percentage of haemostasis in the 16F group and the 22F group was lower, at 84% and 80%, respectively (Table 1).
Table 1
The number of effective haemostases with 2 Perclose Proglide devices per sheath diameter
| Sheath diameter | Overall access sites n = 384 | 2 closure devices sufficient n = 341 (88.8%) |
|---|---|---|
| 12F | 87 | 77 (88.5%) |
| 14F | 70 | 65 (92.9%) |
| 16F | 71 | 60 (84.5%) |
| 18F | 95 | 85 (89.5%) |
| 20F | 41 | 38 (92.7%) |
| 22F | 20 | 16 (80.0%) |
In 38 cases (9.9%) haemostasis was achieved using 3 Perclose Proglide devices for one access site (Table 2). The distribution of specific sheath diameters is shown in Table 2 and Figure 3. The number of access sites with 3 devices used comprised from 7% to 15% for each diameter. Statistical analysis shows no dependence of the number of closure devices used on the diameter of the sheath used (c2 = 2.436; df = 5; p = 0.786).
Table 2
Structure of vascular accesses with deviation from norm (3 closure devices used, lack of haemostasis, and sum of deviation) due to sheath diameter
In the study, bleeding and use of an additional closure device were estimated as the sum of the deviation from norm. It was observed in 43 (11.2%) of vascular accesses (Table 2). Statistical analysis showed no correlation between all problems together and the diameter of the used sheath (c2 = 4.704, df = 5, p = 0.453).
The lack of haemostasis was observed in 5 cases, which is 1.5% of overall vascular access sites and 11.6% of overall approaches with deviation from norm, including the lack of haemostasis and the need for an additional closure device. Bleeding that lead to surgical repair was observed twice with 12F and 16F sheaths and once with a 22F sheath (Table 2). To estimate the correlation between bleeding and access diameter, the Fisher-Freeman-Halton test (p = 0.122) was used. Statistical analysis suggests that there is no relationship between bleeding and access diameter.
There were 10 post-procedural complications observed in the study group, which is 2.6% of all access sites performed. There were 7 (1.82%) early complications including 4 groin haematomas, one pseudoaneurysm of the femoral artery, and 2 external iliac artery dissections (Table 3). Although both dissections were found in control CTA 6 months after implantation, they were classified as early complications because the authors assumed they were the result of the Perclose Proglide system manipulation. In each case of dissections, it was clinically irrelevant and did not demand additional treatment.
Table 3
Type and number of complications
Furthermore, there were 3 (0.78%) late complications found (Table 3). Two femoral artery stenoses were seen in control CTA, which were not found in pre-operative CTA. In addition, one groin haematoma demanding additional surgical treatment was observed one month after the procedure.
Discussion
The authors evaluated whether the diameter of the vascular sheath affects the efficiency of haemostasis achievement. The results show that there is no correlation between haemostasis and sheath size, and it does not decrease with enlargement of the access site diameter [12]. The statistical analysis also proves that there is no correlation between the diameter of the used sheath and the number of used closure devices to achieve haemostasis [12]. However, in 15% of cases with the largest sheath (22F ID) 3 Perclose Proglide devices were necessary. It suggests that in very large bore access sites the operator should consider using 3 closure devices instead of 2 [11].
In the study group, a high percentage (over 98%) of haemostasis was achieved. In most of vascular accesses (89%) 2 Perclose Proglide closure devices were sufficient, which corresponds with the instructions for use of this product [10]. In 10% of vascular accesses, an additional, third closure device was necessary. In spite of use of a third Perclose Proglide device, there were cases without haemostasis achievement. Bleeding demanding surgical repair was found in 5 cases, which is about 1% of all vascular accesses performed. In all these cases, the reason for unsuccessful haemostasis achievement were atherosclerotic non-calcified changes in the arterial wall. Calcified atherosclerotic changes are a well-known contraindication to percutaneous large-bore access with suture-mediated devices [8,11,12,16-19]. In the study, patients were excluded if severe calcifications in femoral arteries were found in pre-operative CTA. Patients without calcifications were included in the study. The authors consider non-calcified atherosclerotic plaques as a potential risk factor for bleeding [20].
The overall quantity of early and late complications was 2.6%. Early complications were rare and include haematoma of the access site (n = 4) and pseudoaneurysm of the femoral artery (n = 1). Similar complications were observed in previous studies [11]. Dissection of the external iliac artery (n = 2) was also included as an early complication. The authors deem that the dissection found in control CTA is the result of introducing the Perclose Proglide device, which is moving in the vessel without guide wire support in particular moments [16] and it can hook against the atherosclerotically changed arterial wall. In both cases, the dissection found in the study was clinically negligible and it did not impact the patients’ condition. No additional procedures were needed.
Late complications found in the study were rare. There were only 2 stenoses of the access site found in the control CTA, which is lower than other studies [16]. In the observation period, there was no acute limb ischaemia or exacerbation of chronic limb ischaemia in any patient, which is similar to the result of previous studies [11,21]. There was one case of massive haematoma of the groin in a patient admitted to hospital one month after implantation. This patient required surgical repair of the femoral artery [12].
In the study, evaluation of the percutaneous approach due to curvature and calcification of the iliac arteries was not performed because of the difficulties of statistical characterisation. However, anatomical conditions of iliac arteries, considering calcifications or curvature, did not lead to conversion from a percutaneous approach to surgical repair. The low number of complications in the study group and the lack of intraprocedural problems suggests the substantial role of experienced operators and the importance of the learning curve [12,21]. All the implantations in the study group were performed by 2 interventional radiologists with extensive experience in Perclose Proglide closure device usage.
Wound infection or seroma were not found in any of the cases. The use of percutaneous large-bore access to vascular procedures instead of classical surgical access entails less patient injury, limited to a small skin incision. This is the reason for the decreased risk of infection or seroma at the access site and rapid wound healing [17,22]. These factors, in the authors’ opinion, suggest potential benefits from a percutaneous large-bore approach in obese patients, where wound infections and seromas are a severe problem [12]. However, other authors consider obesity as a contraindication to the percutaneous approach, with higher risk of complications [11,13,15,18-20].
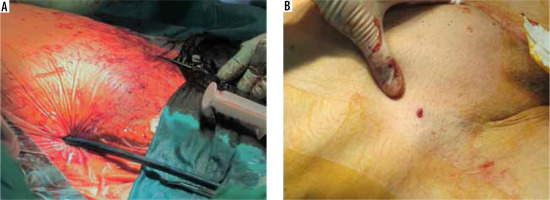
Small skin incision (Figure 4) is also the reason for a good cosmetic effect, which is important especially for younger patients. On the other hand, procedures such as EVAR or TAVI are preformed mostly in older patients, often with co-morbidities, which obstructs general anaesthesia. Minimally invasive percutaneous access allows these procedures to be performed often under local anaesthesia, which is the first choice option in the authors’ institution.
Due to a lack of surgical intervention and scarring in the groin, percutaneous procedures with large sheath devices simplify the performance of renewed endovascular treatment. This is very important, especially nowadays, when more and more cardiovascular diseases are treated using minimally invasive techniques. Renewed vascular access is often necessary not only to perform another treatment, but also to manage with complications of previous methods [19]. Percutaneous access with suture-mediated closure devices, like the Perclose Proglide, allows for further vascular access without restrictions [23].
Conclusions
The usage of closure devices during procedures with large arterial access, such as pEVAR, results in a substantial percentage of successful haemostasis (98% in the study group) together with a low rate of complications (2.6% in the study group).
There was no correlation between the sheath size and the complication rate reagrding the number of devices used to close the vascular access or unsuccessful achievement of haemostasis.
Percutaneous access to procedures with large-bore sheath equipment is effective and safe. Taking into consideration the great number of advantages and the small percentage of complications, percutaneous vascular access to procedures like EVAR, TEVAR, or TAVI, in the authors’ opinion, should be considered in all patients without contraindications.