Introduction
The temporomandibular joint (TMJ) is a bilaterally symmetrical structure connecting the mandible to the cranium. It includes the temporal bone’s mandibular fossa and the mandible’s condylar process, incorporating an articulation disc of soft tissue within this space [1]. The TMJ is essential for mastication, requiring harmonised movements among its components for effective functionality [2]. The mastication muscles significantly influence the TMJ’s operation, with any deviations in the bony structure, articulation disc, or muscles potentially impairing its function. Such impairments can lead to temporomandibular disorders (TMDs) [3]. Therefore, a thorough understanding of the TMJ’s biomechanics and associated elements is crucial for comprehending the origins and management of TMDs [4].
TMDs encompass a range of conditions characterised by pain and dysfunction in the muscles and TMJ. The rising prevalence of TMDs is partly attributable to modern society’s stressful lifestyle, excessive work demands, and limited personal time, all of which place excessive stress on the TMJ system [5]. TMDs are the second most common musculoskeletal disorders causing pain and disability, only surpassed by chronic low back pain, affecting an estimated 5 to 12% of the population [6]. This statistic highlights the importance of TMDs as a primary reason for seeking dental care. Diagnosing TMDs involves a comprehensive evaluation, including clinical and radiographic examinations [7,8]. However, the diagnostic process is complex and faces challenges such as varying clinical expertise and limited access to advanced diagnostic tools like computed tomography (CT) [4].
Since 2014, the diagnostic criteria for TMDs (DC/TMD) have been the gold standard for diagnosing and classifying TMDs [7,8]. This evidence-based protocol aids in systematically examining patients, enabling accurate categorization of symptoms into specific diagnostic groups. The DC/TMD divides disorders into pain-related (PT) and intra-articular (IT) TMDs based on whether the cause is muscular or joint-related [7,8]. PT conditions include arthralgia, myalgia, and headaches attributed to TMD, while IT disorders encompass various types of TMJ disc displacements, degenerative joint disease, and subluxation [7,8].
Following the clinical examination, the subsequent step involves the radiological assessment of the temporomandibular joints. A limited array of imaging modalities proves valuable in the diagnostic process of TMDs. Panoramic X-rays evaluate degenerative bone changes, asymmetries of the condyles, hyperplasia or hypoplasia, trauma, or tumours [9]. However, its utility is primarily confined to more advanced stages because it is inadequate for detecting early osseous lesions [10]. Although CT is well known for its accuracy in visualising TMJ bony structures, accessibility in dental offices and increased radiation exposure are limitations [11].
On the other hand, cone beam computed tomography (CBCT) has gained popularity in dental practices due to its technological advancements. CBCT offers a cost-effective solution with three-dimensional imaging capabilities, covering the mandible and TMJ [12]. Its reduced radiation exposure and high diagnostic efficacy make it a preferred modality for qualitatively assessing osseous structures within the TMJ [13]. Typically, CBCT images offer enhanced reliability and heightened precision compared to panoramic radiography and conventional tomography [14]. Nonetheless, the primary drawback associated with CBCT lies in poor visualisation of the soft tissues of TMJ (disc, synovial membrane, ligaments, lateral pterygoid muscle) [9]. In such instances, magnetic resonance imaging (MRI) emerges as the preferred modality of choice. MRI exhibits particular utility in cases involving degenerative processes or alterations in the position of the TMJ disc [9].
Still, with CBCT’s increasing accessibility, it stands out as a potential tool for enhancing diagnostic efficiency and supporting timely therapeutic interventions. As the prevalence of TMD grows, understanding diagnostic modalities is vital for effective treatment strategies, ultimately improving patient outcomes. This review aims to systematically analyse CBCT’s diagnostic accuracy in detecting bony disorders within the TMJ, offering practitioners an evidence-based comparison with CT imaging.
Material and methods
This systematic review adhered to the methodological framework prescribed by the Joanna Briggs Institute (JBI) for diagnostic test accuracy [15] and followed the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [16]. The main goal of this review was to systematically look at studies that compared CT and CBCT in the examination of TMJ bone conditions, focusing on checking how well CBCT worked for diagnosis.
The mnemonic PIRD (population, index test, reference test, and diagnosis of interest) was employed to structure the critical components of the study design [17]. The assignment of these components is detailed as follows:
population – the target group comprised human patients diagnosed with TMDs and dry skulls with TMJ bone lesions;
index test – CBCT served as the diagnostic tool under investigation;
reference test – CT was selected as the benchmark against which CBCT was evaluated;
diagnosis of interest – evaluation of the TMJ bony structure.
This systematic review aimed to provide a comprehensive synthesis of evidence within a rigorous methodological framework, contributing to advancing knowledge in diagnostic imaging for TMJ analysis.
Searching strategy
The investigation included a comprehensive electronic search across 5 databases (PubMed, Medline, Web of Science, Cochrane, and Scopus) up to 14 July 2023. A meticulously tailored search strategy (supplementary) was employed, with the customisation performed for each database following an initial limited primary search. The search encompassed specific medical subject headings (MeSH) keywords, including “Cone-Beam Computed Tomography” or “CBCT” or “C-arm CT” or “Cone Beam Volume CT” or “Flat Panel CT” or “Digital Volume Tomography” or “DVT” or “Cone-beam CT” and “Temporomandibular Joint Disorders” or “Temporomandibular Joint Dysfunction Syndrome” or “TMD” or “TMJD” or “Temporomandibular Joint Osteoarthritis” or “Temporomandibular Joint Osteoarthrosis” or “Temporomandibular Joint Arthritis” or “TMJ inflammation” or “TMMJ Degradation” or “Condyle Osteophytes”.
Subsequently, all identified articles were imported into Rayyan, a cloud-based research collaboration library (http://rayyan.qcri.org) [18]. By using Rayyan’s (http://rayyan.qcri.org) deduplication functionality, the library underwent a deduplication process. This rigorous approach ensures the elimination of redundant data and enhances the reliability of the dataset for further analysis and interpretation.
Eligibility criteria
The selection criteria have been based on the mnemonic PIRD [17]. Inclusion includes retrospective clinical trials, cross-sectional analyses, and case-control investigations specifically addressing the diagnostic precision of CBCT compared to CT for TMD assessment in human patients and skulls. Exclusion criteria encompass pilot studies and conference papers. Additionally, studies exploring CBCT’s diagnostic accuracy relative to magnetic resonance imaging (MRI) or panoramic X-rays and those involving animal subjects have been excluded (Table 1). Considering the limited number of studies in this field, no publication date or language restrictions were imposed.
Table 1
Inclusion and exclusion criteria
Study selection
Two autonomous evaluators (M.S. and J.I.) meticulously examined the titles and abstracts of the gathered data in alignment with predetermined inclusive criteria, following a methodological pilot test. Subsequently, the prospective articles identified during the initial screening underwent further scrutiny as their full texts were independently subjected to detailed assessment by the reviewers, adhering to the established inclusive criteria. Any discrepancies between the 2 reviewers throughout the process were resolved through discussion. When necessary, the intervention of a third reviewer (M.D.K.) was sought to reach a consensus.
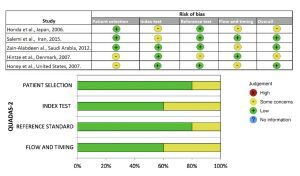
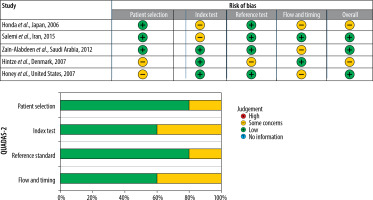
The risk of bias in the included studies was investigated using the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool [19].
Results
Search results
The outcomes of the search strategy are represented in the flowchart diagram (Figure 1) [20]. On 14 July 2023, a total of 3322 studies were retrieved from the searched databases. After deduplication, 1249 studies were excluded. The titles and abstracts of 2073 articles were assessed based on the inclusion and exclusion criteria, identifying 11 articles eligible for full-text assessment. Following a comprehensive evaluation, only 5 studies met the criteria for inclusion in the systematic review.
Study characteristics
The 5 selected studies were published between 2006 and 2015 (Table 2), each conducted in a different country: Japan [21], Iran [22], Saudi Arabia [23], Denmark [24], and the United States of America [25]. All studies employed CBCT and CT, with 2 additionally utilising panoramic radiology [22,25]. Four articles were ex-vivo studies, encompassing 863 TMJ scans across both modalities [22,23-25]. One retrospective article involved 42 TMJ scans, encompassing CT and CBCT modalities [21].
Table 2
Data extracted from included studies.
In the study by Honey et al. [25], CBCT was compared to panoramic X-ray and linear tomography. The tests were done on 30 human skulls using the iCAT (Imaging Sciences International, Hatfield, PA) and the Quint Sectograph (model QS 10-1627W, Denar, Anaheim, California), which gave a total of 37 scans for each modality. CBCT images underwent 2 assessments: the first involved static screen capture (CBCT-S), and the second allowed observers to navigate through axial and para-sagittal image slices (CBCT-I). Ten dentists participated as observers, including oral and maxillofacial radiologists, a TMJ specialist, general practitioners, orthodontists, and orthodontic residents.
Salemi et al. [22] used 3 types of imaging (panoramic radiography, CT, and CBCT) to evaluate 10 temporomandibular joints (TMJs) from 5 dried human skulls that had erosive and osteophytic lesions that were artificially made. Two oral and maxillofacial radiology specialists evaluated 144 CBCT and 144 CT scans, conducted using Cranex 3D (Soredex, Helsinki, Finland) and Cranextom (Soredex, Helsinki, Finland).
In the study by Zain-Alabdeen et al. [23], 5 dried human skulls were utilised. Two experienced oral and maxillofacial radiologists, each with over 5 years of experience, interpreted 660 images. During the gold standard observation session, TMJs were inspected for flattening, erosion, and osteophytes through a naked-eye examination. CBCT and CT scans were performed with ILUMA (IMTEC, Ardmore, OK) and Light Speed 2002 (General Electric Company, Fairfield, CA).
Hintze et al. [24] assessed the accuracy of detecting morphological changes in the TMJ using the NewTom 3G CBCT scanner (Verona, Italy) and the CT Cranex Tome X-ray system (Soredex, Helsinki, Finland). Three observers, including 2 oral radiologists and one general dentist in specialist training, performed naked-eye inspections of morphological changes and evaluated CBCT and CT scans several months later.
In the study by Honda et al. [21], 21 TMJ autopsy specimens were subjected to macroscopic observations, establishing them as the gold standard. The examinations used the 3DX (Morita Co., Japan) and the Lemage SXE helical scanner (GEYMS, Tokyo, Japan). Two oral and maxillofacial radiologists with 20-25 years of experience independently assessed the images, revisiting their evaluations in cases of discrepancies.
Risk of bias
Based on the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool, 3 studies demonstrated a low risk of bias. The detailed quality assessment is depicted in Figure 2.
Discussion
TMD represents a significant public health concern, impacting the well-being of affected individuals. The aetiology of TMD is multifactorial, with various risk factors playing an important role in the onset, progression, and exacerbation of TMD symptoms [26]. Recognising and understanding these factors is crucial in determining the most effective treatment strategies [4]. Radiological examinations are vital for comprehensively evaluating potential TMJ anomalies that may lead to dysfunction. Therefore, in addition to clinical assessments, radiological evaluations using techniques such as CT/CBCT and MRI are crucial for an accurate diagnosis of TMD [7,8]. The advent of CBCT has revolutionised dental practice, marking a significant shift with numerous advantages. These include notable reductions in exposure time, radiation dose, and overall costs, positioning CBCT as a superior imaging modality compared to other techniques [27]. These factors collectively establish CBCT as the gold standard for imaging in the oral and maxillofacial regions [28]. However, there remains a debate regarding the accuracy of CBCT compared to CT in detecting bony defects of the TMJ. This systematic review aims to evaluate the diagnostic validity of CBCT in the context of osseous changes in the TMJ.
In the included studies, the number of experts examining TMJ scans ranged from 2 to 10, including general dentists, oral and maxillofacial radiologists, TMJ pain specialists, orthodontists, and orthodontic residents in their final year of training. Results from each modality were compared. Only 2 studies [21,23] provided comprehensive data on true/false positive and true/false negative results. Sensitivity and specificity were reported in 4 studies [21-24], while one study [25] presented the receiver operating characteristic (ROC) area (0.6-0.81) and accuracy (CBCT-I 0.95 ± 0.04, CBCT-S 0.77 ± 0.17, CT 0.58 ± 0.15). Accuracy was also reported in 2 other studies [21,22]. Salemi et al. [22] noted CBCT accuracy ranging from 0.89 to 0.91 and CT accuracy from 0.56 to 0.58, while Honda et al. [21] reported CBCT accuracy at 0.9 and CT at 0.86. Sensitivity for CBCT varied from 0.15 to 0.91, and for CT it ranged from 0.11 to 0.7, while specificity for both CBCT and CT varied from 0.30 to 1.0.
In 3 out of 5 studies, CBCT demonstrated comparable outcomes to CT [21,23,24], while in 2 investigations, CBCT exhibited significantly enhanced accuracy compared to CT [22,25]. The authors [21,23,24] highlighted the limited effectiveness of both CT and CBCT in detecting condylar head flattening and minor to medium bony changes, which are typically challenging to visualise radiologically [29]. Two studies reported significantly lower sensitivity values than others [23,24]. CT and CBCT may not be as sensitive because they might miss small changes in the condylar bone [23,24] and because they simulate soft tissues for research purposes [23]. Zain-Alabdeen et al. [23] used water immersion of skulls to simulate soft tissues, which decreased sensitivity for both modalities. Image quality and interpretation differences arise between dry-scanned mandibles and those immersed in water [30]. Conversely, Salemi et al. [22], who also simulated soft tissues, reported a relatively high sensitivity of 88-91% for CBCT. However, their CBCT specificity was notably low at 30%, diverging from other studies in this review and presenting a unique case. Nonetheless, in their research, CBCT consistently demonstrated superior accuracy, sensitivity, and specificity compared to CT. Notably, in both remaining studies [22,25], where soft tissue simulation was performed, CBCT yielded superior results. This difference might stem from the fact that CBCT has inherently low soft-tissue contrast compared to traditional CT scanners, potentially enhancing image interpretation and defect detection [31].
Additionally, CBCT’s ability to create multiplanar images in the sagittal, coronal, and axial planes of the body, which can be reconstructed in different ways, improves the comprehensive evaluation of the condyle within the glenoid fossa [30].
Undoubtedly, all scientists concur on the greater detection sensitivity of CBCT compared to panoramic images. Panoramic images provide a two-dimensional representation of three-dimensional structures and do not fully depict the TMJ in all dimensions. This means that bony defects might not be adequately seen or are shown incorrectly because of heavy superimposition [4,28,32]. Furthermore, panoramic images may not allow for a focused assessment of specific TMJ regions, hindering the detection of localised defects [33]. CBCT, with its capability to reconstruct images in various planes, provides more detailed and targeted information about specific areas within the joint. Panoramic images are also susceptible to artifacts and distortions that compromise diagnostic accuracy. These artifacts may obscure or mimic bony defects, potentially misinterpreting the TMJ condition [34,35]. Honey et al. [25] and Salemi et al. [22] have demonstrated CBCT’s superiority over panoramic imaging in detecting TMJ bony defects. These studies highlight the higher sensitivity and diagnostic accuracy of CBCT for evaluating the bony structures of the TMJ. Therefore, a crucial issue in this field is determining whether CBCT is the preferred method for assessing the bone structures of the TMJ or whether CT remains the optimal choice.
CBCT, optimised for maxillofacial imaging, enables detailed visualisation of the TMJ’s bony structures. CBCT systems, including the TMJ, typically have a focused and smaller field of view (FOV) tailored to the maxillofacial region. This focused imaging allows for higher resolution and reduced radiation exposure compared to conventional CT, which often covers a broader body area [27,36]. Furthermore, the utilisation of AI-based algorithms enables noise optimisation in images, thereby enhancing the objective image quality of CBCT images [37].
CBCT also involves a lower radiation dose than conventional medical CT scans, a significant consideration in dentistry where repeated imaging may be necessary, and minimising radiation exposure is crucial for patient safety [27]. The design of CBCT machines specifically for dental and maxillofacial imaging, including the patient’s standing or sitting position during acquisition, is crucial for proper TMJ imaging. CBCT provides three-dimensional images, enabling a more comprehensive and accurate assessment of the TMJ, which is particularly valuable for evaluating complex anatomical structures, detecting changes in bone morphology, and assessing spatial relationships within the joint. While the cost-effectiveness of CBCT may vary based on location and equipment, and it was not analysed in our study, it is generally considered more cost-effective for dental and maxillofacial applications than conventional CT, making CBCT a practical choice for routine clinical use in dentistry [27].
It is imperative to acknowledge several limitations inherent in this review. Firstly, our study stems from a limited number of available studies, predominantly resulting from the pervasive use of a single diagnostic modality in research designs. The quantity of available research is further constrained by inclusion criteria exclusively focused on human studies, excluding a considerable volume of literature involving animal models. It is imperative to acknowledge that due to the limited number of studies included and the utilisation of non-standardised systems, the resultant findings and accuracy may exhibit considerable variability. Additionally, all incorporated studies exclusively employed human specimens, with a notable absence of investigations meeting the established criteria on actual patients. To address these limitations in future reviews, broader inclusion criteria should be implemented to encompass a wider range of diagnostic modalities and study populations.
Conclusions
The evidence from the included studies shows that CBCT provides comparable or superior accuracy in detecting osseous changes within structures of the TMJ. As a result of its lower radiation exposure, higher spatial resolution, and easier accessibility, CBCT is a preferred choice over conventional CT for evaluating the bony structures of the TMJ in dental and maxillofacial settings.