Introduction
Mediastinal and hilar lymphadenopathy is usually diagnosed by computerised tomography (CT) scan, which is also used for staging, with accuracy and specificity of 57% and 82%, respectively [1]. In surgical staging approximately 18% of patients with a negative CT scan develop metastatic mediastinal disease [2]. However, all lymph nodes may not be detected. In these cases, usually thoracoscopy and anterior mediastinoscopy are used [2]. But all these methods for staging are mainly invasive and would result in high costs [3,4]. However, the positron emission tomography (PET) scan may develop high applicability for staging of metastatic lung cancer with lymph node involvement [5], but it is less frequently used due to high costs [6]. Endoscopic ultrasound-guided fine needle aspiration (FNA) was also introduced; the main limitation for this method is the impossibility for airway assessment [7-10].
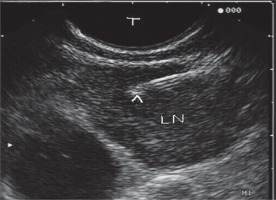
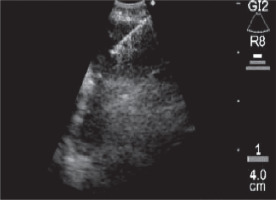
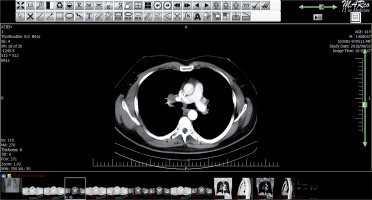
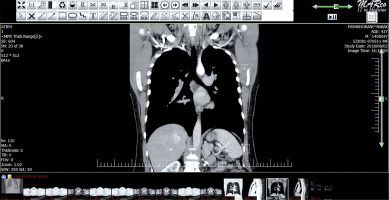
In this era some studies have reported highest applicability in cases using endobronchial ultrasonography (EBUS) with high accuracy in false negative CT scan [11-14]. However, there are some controversies about the role of the EBUS (Figures 1 and 2) versus spiral chest CT scan (Figures 3 and 4) to differentiate between infiltrated and none-infiltrated lymph nodes.
Hence, for improvement in diagnostic approaches, the purpose in this study was to determine the diagnostic accuracy of endobronchial ultrasound and spiral chest CT scan in the prediction of infiltrating and non-infiltrating lymph nodes in patients undergoing endobronchial ultrasound.
Material and methods
In this observational prospective study, 40 consecutive patients with infiltrating and non-infiltrating lymph nodes in Masih-Daneshvari Hospital, Tehran, Iran in 2017 and 2018, who had positive pathology results by biopsy or EBUS but with non-diagnostic spiral chest CT scan, were enrolled. The exclusion criterion was incomplete data.
The study was approved by the local Ethical Committee. Data were collected by existing medical documents and checklist among understudy patients. Also, the pathological findings including benign and malignant status were recorded in the patients. The size and location of the lymph nodes were also determined.
Data analysis was done with SPSS software (Version 25.0), and mean plus standard deviation were calculated for numerical variables, and the frequency and percentage were reported for categorical factors. Kappa test was used to determine the congruence, and the sensitivity, specificity, and accuracy was calculated. P values less than 0.05 were considered statistically significant.
Results
The patient’s age was under 50 years in 17 cases (42.5%). The gender was male in 15 patients (37.5%). The CT scan results were positive in 33 patients (82.5%), and the EBUS was positive in 35 cases (87.5%). According to the pathological results, 31 cases (77.5%) were benign. The mean lymph node size was 10.7 mm in CT and 11 mm in EBUS without difference between benign or malignant lesions (p > 0.05). Also, the total range was from 6 to 25 mm.
The results in this study (Table 1) show that the congruence between EBUS and CT scan was 80.5% (p = 0.0001). The sensitivity, specificity, and accuracy for CT scan was 100%, 22.6%, and 40%, respectively (Table 2) and the sensitivity, specificity, and accuracy for EBUS was 100%, 16.1%, and 35%, respectively (Table 3).
Table 1
Congruence between computed tomography scan and endobronchial ultrasound results
Table 2
Computed tomography scan sensitivity, specificity, and accuracy
Table 3
Endobronchial ultrasound sensitivity, specificity, and accuracy
The congruence did not differ according to age, and patients younger and older than 50 years had good congruence between EBUS and CT scan. Also, the congruence did not differ according to gender, and both male and female patients had good congruence between EBUS and CT scan. The congruence was good in benign cases (p = 0.0001), but it was not determined according to the location, malignancy, and stage of the malignancy (p > 0.05).
Discussion
The main utilised method to diagnose mediastinal lymphadenopathy is CT scan, but it would show low accuracy. The highest applicability point is related to EBUS. However, there are some controversies. Because CT scan is a non-invasive method, in this study the accuracy of EBUS and spiral CT scan was assessed. The congruence of methods was 80.5% and significant. The sensitivity for methods was 100% and the specificity was near to 20% with accuracy rate of 35 to 40%. Age and gender subgroups both had good equal concordances. The congruence was higher in benign lesions. It is not clear in malignant lesions. Also, the location and stage effects were impossible to determine. Udoji et al. [15] reported that lymph nodes had larger size in EBUS versus CT scan assessment. In our study, despite a lack of difference between benign and malignant lesions, it was larger in EBUS evaluation.
Helmy et al. [16] assessed 11 patients who were suspected of having lymph node malignancy without CT scan positive results. The malignancy was reported in 54.4% of cases under bronchoscopy, 18.2% under EBUS-TBNA, and 27.3% under CT-guided biopsy. From 11 cases with negative CT scan the EBUS was positive in four patients [16]. In our study the malignancy rate was lower, but similarly EBUS had good applicability.
Nakajima et al. [17] showed that among 106 patients with metastatic lung cancer the sensitivity and specificity were 92% and 100%, respectively. Their sensitivity and specificity were lower and higher than ours, respectively. Memoli et al. [18] reported malignancy in lymph nodes in 22.5% of cases and reported good diagnostic applicability for both CT scan and EBUS method as well as our study.
Jhun et al. [19] reported sensitivity and specificity of 92% and 99%, respectively, for EBUS, which was related to lymph node location. However, in our study, due to the small number of hilar samples, a comparison was impossible. Lee et al. [20] assessed 247 patients with hilar and mediastinal lymphadenopathy and reported that older age and pathological results were related to higher false negative rates. In our study the benign status had some effects on congruence between methods, but there was no difference for age.
According to the obtained results it may be concluded that CT scan and EBUS results have good congruence and high sensitivity to differentiate infiltrating and non-infiltrating lymph nodes. Hence, these methods are useful for screening methods, but due to their low specificity and accuracy their use for a confirmative approach is not beneficial. However, regarding its accessibility and less invasive nature, the use of chest CT scan is more rational and is recommended in these patients. However further studies with larger sample sizes and controlling for confounding factors would develop more definite results.