Introduction
Research has shown that child-seeking women aged 20-44 years in sub-Saharan Africa experienced higher rates of secondary infertility at 11.7% (9.9%, 13.4%) when compared to the international average of 10.5% (9.5%, 11.7%) [1].While secondary infertility rates have declined in sub-Saharan Africa from 14.3% in 1990 [1], infertility remains an urgent problem, causing severe social, economic, and psychological problems in many local communities [2].
Infertility is the failure to conceive after at least 12 months of regular unprotected sexual intercourse. Primary infertility occurs when a woman or couple has never been pregnant. Secondary infertility is the inability to conceive after having an earlier conception, regardless of whether it resulted in a live birth or not [3]. Subfertility is any form of reduced fertility with prolonged time of unwanted delay in conception [4]. Infertility in women is usually caused by disorders of the fallopian tubes, uterus, cervix, or ovaries. Fallopian tube disorders are the primary reason for infertility in about 35-40% of patients [5].
Hysterosalpingogram (HSG) is a valuable radiologic procedure utilised for assessing fallopian tube patency, as well as the morphology of the uterus and cervix [2]. HSG has a sensitivity of 94% and a specificity of 92% in detecting tubal blockage [6]. For diagnosing congenital uterine anomalies, HSG has a 78% sensitivity and 90% specificity [7]. HSG may additionally offer a therapeutic advantage through tubal flushing and the treatment of proximal obstruction [8]. Filling defects on HSG may signify synechiae, polyps, leiomyomas (submucosal), or endometrial hyperplasia [9]. Once detected by HSG, many abnormalities will require follow-up evaluation or treatment with laparoscopy, hysteroscopy, or pelvic ultrasound [10]. Recent studies utilising HSG to evaluate secondary infertility in Nigeria reported tubal pathologies as the predominant finding, seen in 30-35% of patients, with others reporting uterine cavity abnormalities as the predominant finding in 50.8% [2,11-13]. A prior study in the United Kingdom found an 8-24.5% frequency of uterine malformations in infertile and sterile patients compared to 5.5% in an unselected population [7].
In more developed countries, other imaging modalities are used for the work up of infertility. Magnetic resonance imaging (MRI) is non-invasive, does not utilise ionising radiation, and requires less reader subjectivity [14]. The disadvantages of MRI are its relatively high cost and longer examination time. MRI is also contraindicated in patients with pacemakers, cochlear implants, and certain metallic objects [14]. Hysteroscopy and laparoscopy are other useful methods for working up infertility but are more invasive and expensive procedures for fallopian tubes, uterus, and cervix evaluation [15]. In Nigeria and most of sub-Saharan Africa, HSG is still predominantly used over other modalities due to its being easily affordable, available, and simple to interpret [5]. Nigeria is of particular interest due to both the high prevalence of Nigerian immigrant communities across the Western world and being home to a significant portion of the global Black population.
This study aimed to describe the pattern of HSG findings in a population of women with infertility, as previously recorded by Nigerian researchers, and to explore relationships between abnormal HSG findings and the various types of infertility.
Material and methods
This was a retrospective cohort study of patients seen at Union Diagnostics and Clinical Services Plc, Lagos, Nigeria. We enrolled all consecutive patients who had HSG evaluation from 2016 to 2018. Biodemographic information and the indications for HSG evaluation were also obtained. Patients were referred for HSG evaluation due to various indications such as routine examination, primary infertility, secondary infertility, or subfertility.
The HSG was performed using standard procedures as stipulated by the American College of Obstetrics and Gynaecology (ACOG) [13].
The patient laid supine on the radiography table and the perineum was disinfected. Thereafter, a Cusco’s speculum was inserted into the vagina and secured. This enables the cervix to be visualised and cleaned. A vulsellum was then used to hold and stabilise the anterior wall of the cervix [13]. Next, a Leech-Wilkinson cannula or an appropriate-size Foley catheter was inserted into the cervical Os and contrast was introduced into the uterine cavity to outline the cervical canal, uterine cavity, and the fallopian tubes. X-ray films were taken as the contrast medium filled the uterus and tubes [2]. Standard views taken included an anterior/posterior (AP) view of the pelvis, right and left lateral obliques, and a delayed film after 30 minutes when necessary. After the images had been obtained, the cannula was removed [13].
One of the precautionary measures before the procedure was the “10-day rule”. The 10-day rule states that ionising radiological examinations and HSG should be confined within the first 10 days after the last menstrual cycle to avoid the possibility of accidentally irradiating the developing foetus and avoid the occurrence of an ectopic pregnancy [13]. One attending radiologist (the second author) interpreted all the images.
Statistical analysis
Descriptive statistics of the data were generated. Continuous variables were presented as medians and interquartile ranges, while categorical variables were described by frequencies and proportions. Univariate logistic regression evaluated individual associations between the presence of infertility and the presence of cornual tubal occlusion, hydrosalpinx, tubal occlusion, perifimbrial occlusion/tubal blockage, and age. Additionally, we performed multivariate logistic regression to explore the relationship between the presence of infertility and all the covariates estimated in univariate logistic regression analyses. For univariate and multivariate logistic regression analyses, the presence of infertility was defined as the presence of primary, secondary, or subfertility. Cornual tubal occlusion was defined as the presence of left, right, or bilateral cornual tubal occlusion. Hydrosalpinx was defined as the presence of left, right, or bilateral hydrosalpinx. Tubal occlusion was defined as the presence of left, right, or bilateral tubal occlusion. Perifimbrial adhesion/tubal blockage was defined as the presence of left, right, or bilateral perifimbrial adhesion or left, right, or bilateral perifimbrial blockage.
Analyses were conducted using Stata version 15.0 (StataCorp LLC; College Station, TX) via a logistic regression fit model. Alpha of 0.05 or less represented a statistically significant result.
Results
The radiology reports of 450 patients were analysed. Ages ranged from 21 to 51 years with a mean age of 34.6 ± 5.56 years. Out of the 450 total patients, 299 patients were referred on account of infertility. Primary infertility was seen in 79 patients (17.6%), secondary infertility in 211 patients (46.9%), and subfertility in nine patients (2%). Clinical indication for HSG was not stated by the requesting physician for 151 patients (33.6%) (Table 1). The frequency of the various forms of infertility by age are displayed in Table 2. Some patients had had previous gynaecological procedures: nine patients (2%) were post-myomectomy, and four patients (0.89%) were post-salpingectomy.
Table 1
Infertility status breakdown and corresponding percentages among 450-patient cohort
| Type of infertility | n (%) |
|---|---|
| Primary infertility | 79 (17.6) |
| Secondary infertility | 211 (46.9) |
| Subfertility | 9 (2.0) |
| Total | 299 (66.4) |
Table 2
Frequency of infertility among age groups
| Age category (years) | Presence of infertility, n (%) |
|---|---|
| 21-25 | 6 (1.33) |
| 26-30 | 70 (15.6) |
| 31-35 | 102 (22.7) |
| 35-40 | 70 (15.6) |
| 41-45 | 36 (8.0) |
| 46-50 | 11 (2.4) |
The frequencies of various structural abnormalities found on HSG are as follows. There were five patients (1.11%) found to have uterine fibroids/leiomyomas. One patient (0.22%) was found to have a uterine synechiae (Figure 1), and one patient (0.22%) was found to have a uterine leiomyoma (Figure 2). Patients with uterine fibroids/leiomyomas, uterine synechiae, and post-gynaecological procedures were not recorded to have any class of infertility. More specific HSG findings were reported across the entire patient cohort. There were 49 patients (10.9%) with cornual tubal blockage, of whom 36 (8.0%) had some form of infertility (Table 3). There were 57 patients (12.7%) who had perifimbrial adhesion and/or blockage. A form of infertility was recorded for 36 of such patients (Table 4).
Figure 1
Hysterosalpingogram AP pelvis spot film showing a persistent, irregular/ragged filling defect centrally within the uterine cavity, which is in keeping with uterine synechiae

Figure 2
Hysterosalpingogram AP pelvis spot film showing an enlarged, lobulated, and elongated/thinned-out uterine cavity, which is displaced cephalad. An oval filling defect is seen at the lower uterine segment while a linear filling defect is sighted in its mid-portion (cicatrisation from previous instrumentation and/or infection). Both uterine tubes are not demonstrated. The overall picture is suspicious for multiple uterine and cervical leiomyomata with bilateral tubal blockage

Table 3
Cornual tubal blockage cross tabulated against fertility status
Table 4
Perifimbrial adhesion and blockage versus fertility status crosstabulation
There were nine patients (2.0%) with tubal occlusion, and of such patients, three had infertility (Figure 3). Left tubal occlusion was seen in five patients (1.1%), right tubal occlusion was not seen in any patients, and bilateral tubal occlusion was seen in four patients (0.9%), (Table 5).There were 56 patients (12.4%) with hydrosalpinx, and 44 of such patients (9.8%) had a form of infertility (Figures 4A and B). Left hydrosalpinx was observed in 15 patients (3.3%), right hydrosalpinx in 26 patients (5.8%), and bilateral hydrosalpinx in 15 patients (3.3%) (Table 6). There were three patients who had an unspecified pelvic mass on HSG examination, which were likely to have been dermoid cyst, calcified myoma, or bladder calcification.
Figure 3
Hysterosalpingogram AP pelvis spot film showing rounding-off of both uterine cornua and extravasation into the periuterine veins (appearing like a necklace around the uterine cavity). Both Fallopian tubes were not outlined. This is indicative of bilateral tubal occlusion

Table 5
Tubal occlusion versus fertility status crosstabulation
Figure 4
A) Hysterosalpingogram AP pelvis spot film showing a normal uterine cavity with bulbously dilated distal portions of the uterine tubes bilaterally, without contrast spillage into the peritoneum. B) The 30-minute delayed film shows contrast retention/loculation with within the dilated distal Fallopian tubes. These findings are conclusive for bilateral hydrosalpinges with bilateral tubal occlusion
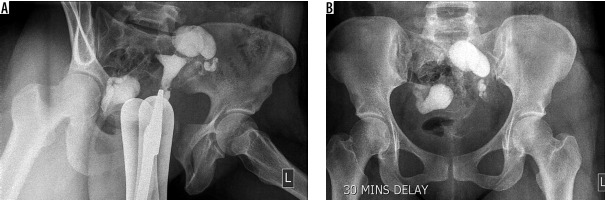
Table 6
Hydrosalpinx versus fertility status crosstabulation
We evaluated individual associations between cornual tubal occlusion, hydrosalpinx, tubal occlusion, perifimbrial occlusion/tubal blockage, age, and the presence of infertility by using univariate logistic regression. Under univariate analysis, women with hydrosalpinx were more likely to be infertile than those without hydrosalpinx (OR = 2.00, 95% CI: 1.02-3.91, p = 0.043), and women with tubal occlusion were less likely to be infertile than women without tubal occlusion (OR = 0.29, 95% CI: 0.06-0.99, p = 0.049). Cornual tubal occlusion, perifimbrial occlusion/tubal blockage, and age were not significantly associated with the presence of infertility under univariate analysis. Under multivariate logistic regression analysis, women with hydrosalpinx were 2.12 times more likely to be infertile than those without hydrosalpinx (95% CI: 1.02-4.36, p = 0.042) (Table 7).
Table 7
Multivariate logistic regression for explanatory variables and presence of infertility, odds ratio and 95% CI
Discussion
Hysterosalpingogram has been used to assess fallopian tube obstruction, pelvic inflammatory disease-related adhesions, masses, cornual tubal blockage, and uterine lesions. It reveals abnormalities in the cervix, uterus, and fallopian tubes, and due to its low cost and non-invasive nature it is the first-line modality in many developing countries [2]. HSG can also be used to localise missing intrauterine devices (IUCD) in resource-poor settings [16].
Among our cohort of patients, secondary infertility (70.6%) had the highest frequency followed by primary infertility (26.4%), with subfertility (3.0%) having the lowest frequency. A similar study at the King Fahad Military Medical City in Saudi Arabia found primary infertility to be the most prevalent among 303 patients [17]. At the Addis Ababa University in Ethiopia, primary infertility had the highest prevalence in a study of 331 patients [18]. Authors of similar studies in Nigeria, such as Abubakar et al. in Sokoto, also reported secondary infertility to be the most prevalent indication for HSG [3]. This higher incidence of secondary infertility in Nigeria could be due to puerperal and postabortal sepsis [19]. The shortage of standard healthcare facilities across various regions in Nigeria has forced many women to undergo delivery under unsanitary conditions. The shortage has additionally led to unsafe abortions and poorly managed spontaneous abortions, which result in tubal and pelvic infections followed by secondary infertility. Voluntary termination of unwanted pregnancy is illegal in Nigeria and is still largely viewed as taboo, forcing many to patronise quack abortionists.
The age group 31-35 years had the highest frequency of infertility, with 102 patients (22.7%) reporting at least one form of infertility. This finding agrees with the findings of previous studies. A study at the Korle-Bu Teaching Hospital in Accra, Ghana also found the highest frequency of infertility in the 30-34-years age group [20]. In some Nigerian communities, women tend to marry in their early twenties; therefore, having the highest frequency of infertility in the 31-35-years age group suggests that many of the women in our cohort had had previous conceptions and were having trouble conceiving subsequently. In our multivariate analysis, age was not a statistically significant predictor of infertility in our patient cohort.
Blockage of the cornual region of the fallopian tubes is a commonly seen abnormality on HSG examination. In our study, cornual tubal blockage was observed with higher frequency in patients referred for secondary infertility compared to those referred for primary infertility. A similar retrospective study in Oman found a higher prevalence in primary infertility compared to secondary infertility by a ratio of 11 : 1 [21]. It is important to highlight that in the Omani study, primary infertility had a significantly higher prevalence in their overall patient cohort, so any abnormal finding is more likely to occur among the patients with primary infertility. Multivariate logistic regression also showed that cornual tubal blockage did not predict female infertility among our patients.
Hydrosalpinx is another important abnormal finding on HSG examination among patients presenting with infertility. Among our patient cohort with hydrosalpinx on examination, secondary infertility had the highest prevalence in those with left hydrosalpinx, while primary infertility was slightly more prevalent in those with bilateral hydrosalpinx. Overall, in patients with all forms of hydrosalpinx, the prevalence of secondary infertility was twice the prevalence of primary infertility. Right hydrosalpinx was the most prevalent in our study, at 5.8%, compared to left hydrosalpinx, at 3.3%. This result agrees with some other studies in sub-Saharan African women. A study in Nigeria also found that the increased prevalence of hydrosalpinx on right side is probably due to the presence of the appendix [22]. The overall incidence of hydrosalpinx in our study was 12.4%, which is comparable to the incidence of 12.6% reported in Enugu, Nigeria [23]. A retrospective study in Nigeria examining infertile women reported a significantly higher incidence of hydrosalpinx over 10 years [24]. The widespread occurrence of hydrosalpinx in Nigeria and other parts of sub-Saharan Africa is due to the prevalence of pelvic inflammatory disease (PID) in the region. These infections cause adhesions commonly at the ampullary region of the fallopian tubes, which usually leads to blockage of the tubes [2]. The resulting blockage causes accumulation of secretions within these blocked fallopian tubes, which cause tubal dilation and the resulting hydrosalpinx.
Logistic regression under univariate analysis showed a statistically significant correlation between hydrosalpinx on HSG examination and some form of infertility. Even when we adjusted for possible confounding factors via multivariate analysis, women with hydrosalpinx were still twice as likely to develop infertility compared to women without hydrosalpinx. This correlation is congruent with the established notion in the literature that pelvic infections cause hydrosalpinx, which then leads to infertility [2].
Tubal occlusion is another abnormal finding on HSG examination found in our patient cohort. Bilateral and left tubal occlusion was seen in our patients, while right tubal occlusion was not present. This result is divergent from similar studies. A study in Sokoto, Nigeria found right tubal occlusion to be the most prevalent, while another study found bilateral tubal occlusion to be more prevalent [13,25]. The difference in our findings compared to theirs may have been due to the smaller number of patients with tubal occlusion in this study.
Tubal abnormality (blockage and dilatation/hydrosalpinx) had the highest prevalence in our study. This is analogous to patterns found in similar studies across the world. A retrospective study involving 4108 patients in Karachi, Pakistan also found tubal abnormalities to be the most common cause of infertility [26]. The high incidence of tubal abnormalities in our patient cohort may be explained by the recurring theme of prevalent pelvic infections in sub-Saharan Africa. A similar HSG study in Nnewi, Nigeria concluded that this finding could also be due to surgical interventions such as appendectomy and its subsequent complications [27]. Univariate logistic regression found a statistically significant inverse correlation between tubal occlusion and infertility. The small sample in our univariate logistic regression between tubal occlusion and infertility could have resulted in the odds ratio of < 1, which signifies an inverse relationship. Therefore, despite our finding, we still agree with the conclusions from other studies showing a direct correlation between tubal occlusion and infertility [1]. This is probably the result of higher rates of untreated pelvic infections due to Neisseria gonorrhoeae and Chlamydia trachomatis, as well as postabortal and post-delivery complications [1].
Perifimbrial adhesion and blockage have been widely reported as cardinal findings on HSG examination. A study at the Mulago Hospital in Kampala, Uganda found that 17.3% of their patient cohort had fimbrial end adhesions [19]. In Tunisia, tubal adhesions accounted for 23% of infertility [28]. In Enugu, Nigeria, perifimbrial adhesions were found to be prevalent at 29.8% [23]. Their results are higher than ours, with 6.8% of the patients in our study having perifimbrial adhesions. A retrospective study at the University Medical Centre of the Johannes in Mainz, Germany found a statistically significant correlation between adhesion and tubal pathology. They also found previous appendectomy to be a statistically significant risk factor for adhesions [29]. We found no statistically significant correlation between perifimbrial adhesions/blockage and the presence of infertility, which may be due to the relatively small number of such patients in our study. The study in Germany differed from ours in that the diagnoses were made surgically via laparoscopy and chromopertubation, and primary infertility was more prevalent in their patient cohort. Univariate and multivariate logistic regression was done on a perifimbrial adhesion and blockage as a combined explanatory variable because they occur in the same region of the fallopian tube, and perifimbrial adhesion probably leads to perifimbrial blockage.
Our study has several strengths. It is a large study exploring associations between infertility and several potentially modifying factors in the cosmopolitan environment of Lagos, Nigeria. Additionally, we were able to explore subcategories of covariates and their impact on different subtypes of infertility. While this study involves a population of Nigerian women with infertility, the findings from this study may be of use to physicians across the world, especially in western countries. The findings in this study may be helpful to clinicians as they encounter Nigerian patients or patients of African descent, wherever they practice internationally.
There were several limitations in our study. First, the number of cases for several of the explored covariates was relatively small, particularly with regards to women with tubal occlusion, so the measured associations might not be representative of all women seen in a private hospital setting in Nigeria. Second, this is a retrospective study of women, meaning we were not able to go back and confirm the presence of infertility and pelvic infections.
Conclusions
While having its inadequacies, HSG is a low-cost, easy to interpret, and readily available imaging modality for assessing infertility. Our study found secondary infertility to be more prevalent, and women in the 31-35-years age group presented with the highest rates of all classifications of infertility. The presence of hydrosalpinx was a significant risk factor in developing all types of infertility. Understanding the HSG patterns and their correlations with infertility will help physicians across the world when evaluating infertility in patients of similar background to our patient population.


