Introduction
So far, no publications have focused specifically on metastases to the reproductive system in girls. There is also scant literature focusing on metastases to the reproductive organs in women in general, except for ovarian metastatic cancers [1]. An overview of these few articles is included in Table 1. In one of the studies 325 women with metastases to the genital tract were described, of which one case was a 10-year-old girl with metastasis of a parotid gland rhabdomyosarcoma (RMS) to the ovary [2]. This is different in the case of primary RMS, for which genitourinary location is the second most common site of origin (25%) after head and neck regions (35-40%) [3,4].
Table 1
The revised literature
The breasts, although located far from the other female reproductive organs, are considered accessory organs of the female reproductive system because they contain the mammary glands. As for breast metastases, they are extremely rare from extramammary carcinomas in adults [5] and infrequent in the paediatric population – according to the literature, their incidence is approximately 6% in children [6]. In girls, they most often arise from tumours of the haematopoietic system and of the soft tissues, especially RMS [7].
In this review we describe the more and less common metastases to the female reproductive system and to the breast and illustrate them with 4 cases of girls with metastases of soft tissue or bone sarcomas from the tertiary referral centre. By including these case reports, we aimed to make a wider readership aware of the fact that such metastases can also be encountered in the youngest female patients and can derive from different sources than those in adults.
Review
Metastases to the female reproductive organs
Within the reproductive tract, the ovaries and vagina are considered as the organs most commonly affected by metastatic disease [8,9].
Ovaries are a relatively common site of metastatic disease in general, and up to 30% of ovarian tumours in adults are metastatic [1]. Their incidence is influenced by geographic differences in primary neoplasms occurrence; for instance, gastric cancer is more common in Asian countries and metastatic disease to the genital tract is more prevalent there [8]. The primary malignancies are located in the gastrointestinal tract in a broad sense (most often in the colon/rectum and stomach, but including biliary tract, pancreas, etc.), breast, lung, bladder, and cutaneous melanoma [1,8,10].
A well-known term: Krukenberg tumour, means a metastatic signet-ring cell adenocarcinoma of the ovary, often bilateral, originating from a gastrointestinal primary in 70% of cases, or from the breast and biliary tract [11] (Figure 1).
Figure 1
A 66-year-old woman with gastric carcinoma (poorly cohesive ca) after total gastrectomy with lymphadenectomy, postoperative chemoradiotherapy with 45 Gy radical radiotherapy to the gastric area and regional lymph nodes. Follow-up magnetic resonance imaging – Krukenberg tumours (arrows) confirmed after surgery: within the ovaries metastases of signet ring cell gastric cancer. Upper row: inhomogeneous abnormal ovaries on T2-weighted image (T2WI) (A), STIR (B) with inhomogeneous diffusion restriction (C). T1WI before (D) and after contrast medium administration (E, F) – very inhomogeneous contrast enhancement of the affected ovaries
In children and adolescents these metastases are extremely rare – in the literature, we have found one case report in a 16-year-old girl with a gastric primary [12].
While considering the metastatic character of ovarian lesions one must take into account synchronous endometrial and ovarian cancer (SEOC), which is a relatively rare entity with a better prognosis compared to metastatic malignancy of each organ (Figure 2).
Figure 2
A 52-year-old woman with the absurd suspicion of adenomyosis, put forward after ultrasound. Multiple tumours in the uterine body and cervix as well as in both ovaries. After surgery: synchronous G1 endometrioid carcinoma of the uterus and ovaries, most likely on the basis of endometriosis. The arrows point at the smaller lesion in the left ovary. A, B) T2WI, C) STIR, D-F) post-contrast T1WI
In these cases, pathological evaluation is required to distinguish SEOC from metastatic disease [13].
In the vagina, metastases account for as much as 80% of malignant tumours, and approximately two-thirds of those derive from cervical (mainly) and endometrial primary cancers [14] (Figure 3).
Figure 3
A 71-year-old woman with a diagnosis of endometrial carcinoma (A-D). Magnetic resonance imaging shows the additional findings: metastasis to the vagina (A, D-F, arrows) and to the right ovary (B, C). A, B, E) T2WI, C, D, F) post-contrast T1WI
Metastases to the uterus are rare and derive from breast, colon, stomach, pancreas, gallbladder, lung (Figure 4), cutaneous melanoma, urinary bladder, and thyroid [15].
Figure 4
A 54-year-old woman with adenocarcinoma of the left lung with known metastases in both lungs and adrenal glands. Magnetic resonance imaging (MRI) showed metastases to the uterine corpus (as a whole) and focally to the cervix (A, D), to the vagina on the left side (B, C, F), to the urinary bladder on the left side (A-D, F), and to the urethra (E). Bone metastases were also depicted on pelvic MRI (not shown here). A, B, E) T2WI, C) T1WI, D, F) post-contrast T1WI
Understandably, these changes are mainly described in adult women and mainly in non-sarcoma cases.
Sarcomas as a primary
Sarcomas are a very diverse group of malignancies of mesenchymal origin. In the young adult group of patients (aged 20-39 years) sarcomas represent 4% of all malignancies [16]. It is estimated that in children, they constitute approximately 10% of all solid tumours [17,18]. They are broadly divided into soft tissue and bone sarcomas. They are further delineated into RMS, the most common paediatric soft tissue sarcoma primarily affecting younger children, and nonrhabdomyosarcoma, which is more frequently observed in adolescents. The most prevalent types of bone sarcomas include osteosarcoma (OS) and Ewing sarcoma (ES) [17]. OS and ES metastases to the reproductive system are extremely rarely reported [19,20] (primary primitive neuroectodermal tumours (PNET)/ES of the ovary has been reported in some adult cases while secondary involvement of the ovary is rare [20]).
Rhabdomyosarcoma
Approximately 16% of newly diagnosed RMS patients present with metastases [17]. Typically, these metastases spread through the bloodstream, less frequently through the lymphatic system, and the most frequent metastatic stations are the lungs, followed by lymph nodes, bone marrow, and bones.
The frequency of RMS metastases to the reproductive system in girls is not well-established. There are notably fewer documented cases in the available literature regarding metastases to the genital tract compared to the cases involving the breasts. All cases reported so far exclusively depict metastases to the ovaries, with no mention of secondary involvement of the uterus or vagina [2,21,22]. In the literature large studies can be found in which not a single case is described (both of the reproductive tract and of the breast metastases) [23].
In our material, we only had one patient with RMS and metastasis to the ovary detected at the time of diagnosis, which is even rarer. In most cases, metastases to the ovaries are a late manifestation of the disease [21].
Case 1
A 6-year-old girl presented at the oncology clinic with a tumour in her left foot, in the I/II intermetatarsal space. The initial magnetic resonance imaging (MRI) of the left foot outside our institution revealed a tumour of approximately 46 × 54 × 46 mm, predominantly situated on the plantar side, penetrating between the metatarsal bones. There was central necrosis, peripheral diffusion restriction, and contrast enhancement. A biopsy was performed, and atypical alveolar RMS was diagnosed.
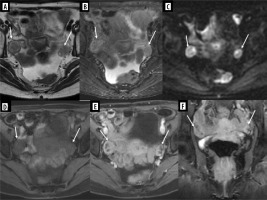
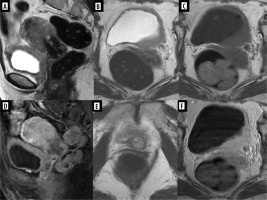
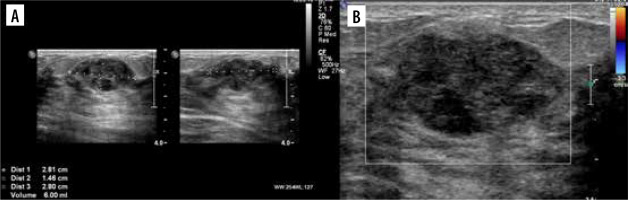
Ultrasound (US) at our institution identified 2 solid lesions with suspected metastatic characteristics alongside the primary foot tumour: one in the right ovary (oval, relatively homogeneous, with medium-high echogenicity, approximately 20 × 16 × 16 mm – Figure 5A) and the other one in the right fifth intercostal space (hypoechoic, with slightly polycyclic outlines, about 14 × 11 × 7 mm). Pelvic MRI corroborated the presence of these findings and additionally detected metastasis in the left gluteus maximus muscle and a suspicious left inguinal lymph node. The ovarian metastasis exhibited peripheral diffusion restriction and contrast enhancement (Figures 5B-F).
Figure 5
Exams of the right ovary metastasis in Patient no. 1. A) Initial ultrasound; axial and sagittal plane. B-F) Pelvic magnetic resonance imaging. B) FSE/T2, axial plane, C) STIR, coronal plane, D) WATER/T1 post-Gd, axial plane, E) DWI, axial plane, F) corresponding ADC map
Whole-body MRI (WB-MRI) did not reveal any other metastatic lesions. The patient underwent chemotherapy as per the Children’s Oncology Group (COG) guidelines and radiotherapy targeting the primary lesion. A gradual regression of both the primary and metastatic lesions was observed throughout the treatment course. Due to the inoperability of the primary foot lesion (high risk of mutilation) and the initial advancement of the disease, the patient additionally receives targeted treatment with pazopanib. The patient continues systemic treatment, and no disease progression is observed.
In the available literature, in most cases the patients also had alveolar RMS of the limbs. Only in 3 case reports of RMS was metastasis to the ovary the primary tumour not located in the extremities but in the presacral region, nasopharynx, and parotid gland [2,21].
RMS metastases to the ovary rarely cause symptoms [22]. In our patient, a lesion in the right ovary was incidentally detected during abdominal US before the initiation of treatment. Both US and MR images did not show specific features. However, with the knowledge of the primary tumour in the foot, the nature of the focal lesion in the ovary became evident.
Patients with RMS and distant metastases at the time of diagnosis are classified into the highest-risk group according to Intergroup Rhabdomyosarcoma Study (IRS) – group IV. Their multidisciplinary treatment consists of systemic therapy (multiagent chemotherapy) and local therapy (surgery with or without radiotherapy).
Our patient initially received systemic treatment (standard chemotherapy including a three-drug combination – vincristine, dactinomycin, and cyclophosphamide/ifosfamide – VAC) [24]. Due to the inoperability of the primary lesion in the foot (high risk of mutilation) and the initial advancement of the disease, it was decided to qualify the patient for targeted treatment with a multi-tyrosine kinase inhibitor - pazopanib, which is currently undergoing clinical trials for treatment of large unresected intermediate- to high-grade soft tissue sarcomas [25].
Chondrosarcoma
Chondrosarcoma is a malignant tumour of bone that forms cartilage. It occurs more often in adults, with the peak incidence in the 5th-7th decade of life and is the second most common primary bone tumour after OS. It is rare in children [26]. The most common sites of chondrosarcoma metastasis are the lungs, soft tissues, lymph nodes, and bones [27].
The case of our patient with chondrosarcoma is quite unique because it represents secondary tumour involvement of the uterine venous plexus as part of the female reproductive system. It was not a limited tumour, which we usually associate with metastasis, but extensive tumour plugs with calcifications filling most of the pelvic veins, as well as the main venous vessels of the abdominal cavity. We have not found similar cases in the available literature.
Case 2
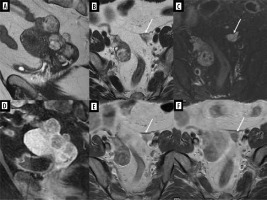
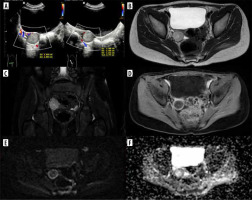
A 15-year-old patient was admitted to our institute for further diagnosis and treatment of a sacral bone tumour. A few days earlier, she was admitted to another centre with shortness of breath, blueness of the fingers, and coldness of the left lower limb. Computed tomography (CT) of the chest, abdomen, and pelvis performed at that time revealed the following: 1) pulmonary embolism with infarction of the lower segments of the left lung; 2) partially sclerotic tumour of the sacrum with aggressive periosteal reactions, extensive periosteal masses with calcifications surrounding the sacrum, infiltrating dorsal and piriform muscles, spreading paraspinally, penetrating the spinal canal through the left intervertebral foramina L2/L3, L3/L3, and L4/L5 and metastatic foci in the L4 and L5 vertebrae; 3) tumour plugs in the vessels – inferior vena cava to the level of the right atrium, common iliac veins, internal iliac veins, left external iliac vein, smaller pelvic veins, including uterine venous plexus, and massive collateral circulation with tumour plugs (Figure 6).
Figure 6
Exams of Patient no. 2 with tumour plugs in the vessels. A, B) Computed tomography (CT) shows partial sclerotic tumour plugs in many vessels, including uterine venous plexus. A) Coronal plane, B) axial plane. C) CT scan shows chondrosarcoma of the sacrum; axial plane. D) MRI study; STIR, coronal plane
After the biopsy low-grade central chondrosarcoma was diagnosed.
In case of chondrosarcoma, the metastatic disease has limited treatment options due to the poor sensitivity of the tumour to chemotherapy and radiotherapy. No standard chemotherapy regimens exist for advanced and metastatic disease [28]. Our patient with unresectable, metastatic chondrosarcoma of the sacrum initially received systemic treatment (chemotherapy), and then she was qualified for and received targeted therapy. The complicated chemotherapy regime in her case was as follows: cycle 1 – ADM (adramycin), cycle 2 – AP (doxorubicin + cisplatin), cycles 3-4 – AI (doxorubicin + ifosfamide), cycles 5-6 – ifosfamide, cycles 7-9 – AI, and cycles 10-11 – IFO (ifosfamide); between cycles 10 and 11 pazopanib was introduced. Subsequently, second-line chemotherapy was initiated – VP (etoposide + carboplatin). Radiotherapy of the primary tumour was also performed between cycles 5 and 6. During the treatment, pulmonary embolism occurred, with a massive embolus filling the left pulmonary artery and the right atrium. Initially, conservative treatment was started (Clexane), but due to lack of clinical improvement, it was decided to evacuate the clots surgically. The embolic material was found to be chondrosarcoma. Positron emission tomography–computed tomography (PET-CT) revealed metabolic reactivation of metastatic foci in L4 and L5 vertebral bodies. The patient was given 2 new targeted drugs - pembrolizumab and cabozantinib, but shortly after starting this treatment the patient suddenly died.
To the best of our knowledge, only one case of secondary involvement of the reproductive system by chondrosarcoma has been described so far. It was an 18-year-old patient with chondrosarcoma of the ribs and metastasis to the left ovary [22], while interestingly in the context of this manuscript, a few cases of primary breast chondrosarcoma have been published [29]. Even more interestingly, we found a case report of intravascular pulmonary tumour embolism 3 years after complete resection of sternal chondrosarcoma, in a way resembling our case, but without calcifications [30].
Metastases to the breast
Breast cancer is the most common malignant tumour in women. Metastatic involvement of the breast, on the other hand, is relatively rare, with a contralateral breast carcinoma being the most frequent primary. Lymphoma and leukaemia are the most common extra-mammary source [31]. Of solid tumours, the commonest malignancies that metastasise to the breast are malignant melanoma, lymphoma, lung and ovarian carcinoma, soft tissue sarcoma, and gastrointestinal and genitourinary tumours (prostate cancer is considered as the most frequent primary site in men). Besides these, metastases from OS and thyroid tumours have been sporadically reported in the literature [32].
RMS as a primary
RMS metastases to the breast are rare, with an incidence of approximately 6%. There is a strong correlation between alveolar RMS localised in the extremities and the occurrence of breast metastases [6]. The analysis of the cases described so far confirms this correlation: in most of them, the primary tumour was alveolar type and was located in the extremities. A similar situation was observed in 2 of our patients, in whom the primary tumour exhibited alveolar architecture on histopathological examination and was located in the right hand and left foot, respectively.
Case 3
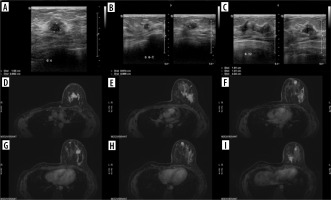
A 14-year-old patient had a lump in her right hand for 7 months, between the first and second metacarpal bones, which was initially assessed as a ganglion. The lesion was finally resected, and histopathological results revealed embryonal partial alveolar RMS. The girl was transferred to our centre for qualification for treatment. In the meantime, she felt a lesion/lump in the right breast. US revealed a nodular lesion 28 × 15 × 28 mm at 12 o’clock with irregular outlines and heterogeneous echostructure (Figure 7), as well as one larger hypoechoic lymph node and several smaller ones in the right axilla.
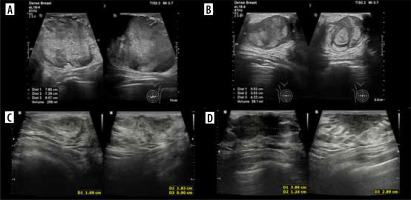
Figure 7
Ultrasound of right breast metastasis in Patient no. 3. A) Axial and sagittal plane. B) Colour Doppler, axial plane
On PET-CT, the breast lesion and the larger axillary lymph node showed increased tracer uptake. A biopsy was performed, which confirmed the metastatic nature of these lesions. During treatment (chemotherapy regimen CEVAIE, i.e. alternating cycles of CEV [carboplatin, epirubicin, vincristine], IVA [ifosfamide, vincristine, actinomycin], IVE [ifosfamide, vincristine, etoposide]; the patient was switched from vincristine to vinblastine after cycle 1 due to neurotoxicity of vincristine) remission of metastases was achieved. The patient was qualified for a right mastectomy with lymphadenectomy followed by radiotherapy (on the tumour bed in the right hand and the lymph nodes of the right axilla – a total of 5000 cGy/t in 25 fractional doses of 200 cGy/t) and maintenance chemotherapy. After approximately 5 months, new lumps were found in the left breast, which turned out to be further metastases. US (Figures 8A-C) and MRI revealed numerous focal contrast-enhancing lesions (Figures8 D-I); the biggest one (35 × 15 mm) was located at 12 o’clock.
Figure 8
Exams show the progression of the disease in Patient no. 3 with metastases in the left breast. Ultrasound: A) nodule at 4 o’clock, axial plane; B) nodule at 6:30 o’clock, axial and sagittal plane; C) nodule at 12 o’clock, axial and sagittal plane. D-I) Breast MRI. Status after right mastectomy. Numerous lesions in left breast. D-I) VIBRANT/T1 post-Gd, axial plane
Second-line treatment consisting of CBDCA (carboplatin) and Topo (topotecan) was initiated; however, progression of breast lesions was detected. The patient was qualified for a left-sided mastectomy with resection of the pectoral muscle and lymph nodes. Histopathological examination confirmed RMS. Despite further treatment (PACE: cisplatin, Adriamycin, cyclophosphamide, etoposide), metastasis in the paravertebral area at the T9-Th10 level was found. Ultimately, the patient died due to complications of chemotherapy – pulmonary mycosis, after 3 years of disease.
Case 4
The parents of a 10-year-old girl noticed a painless lump about 1.5 cm in diameter on her left foot. Over the next 5 months, the lesion gradually enlarged, and lumpy lesions appeared in both breasts. An outpatient US of the left foot was performed showing a tumour of 45 × 24 × 30 mm at that time, with solid-cystic structure; breast US confirmed nodular lesions. MRI of the foot was performed next, less than a month after US, which revealed a mass of size 90 × 45 × 35 mm, located in the plantar muscles of the foot. Histopathological examination confirmed alveolar RMS.
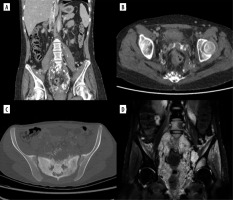
The patient was admitted to our centre for further diagnosis and treatment. On US almost complete involvement of both breasts by heterogeneous, irregularly vascularised nodules was described; in the left breast, the largest ones were located centrally, and had approximately 78 × 73 × 86 mm on the left and 50 × 35 × 42 mm on the right (Figures 9A and B). Additionally, numerous enlarged lymph nodes and a metastasis in the mastoid attachment of the right sternocleidomastoid muscle were found. WB-MRI revealed multiple lesions consistent with metastases throughout the body. On PET-CT, all of them showed increased metabolism of 18F-FDG.
Figure 9
Two ultrasound (US) examinations of breast metastases in Patient no. 4. A, B) Initial examination in our centre. A) The largest nodule in the left breast. B) The largest nodule in the right breast. C, D) The second US after the 4th cycle of chemotherapy. Partial regression of the lesions. C) Nodule in the left breast. D) Nodule in the right breast
The patient was qualified for chemotherapy (VAC), and partial regression of the metastatic and primary lesions was initially achieved (Figures 9C and D).
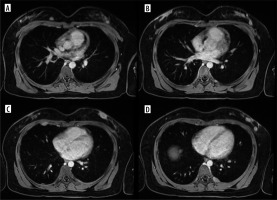
Subsequently, the decision was made to excise metastases from the breasts and administer radiotherapy to the primary tumour. Despite treatment, progression occurred, with new lesions in the breasts and numerous metastases in bones, lymph nodes, lungs, pleura, and soft tissues of the head, chest, right thigh, and left shin (Figure 10).
Figure 10
Magnetic resonance imaging study shows the progression of the disease in Patient no. 4 with new lesions in both breasts and nodules in the pleura. A-D) WATER/T1 post-Gd, axial plane
The patient’s parents declined further treatment, and the patient passed away.
The increased risk of RMS metastases to the breasts is associated with their increased vascularity during adolescence [33]. This is supported by the age range of patients with described RMS metastases to the breast, falling between 11 and 21 years. Our patients also fall within this range – almost 11 and 14 years old.
Secondary involvement of the breasts is often bilateral [6]. In one patient, metastases appeared simultaneously in both breasts as numerous, large masses in all quadrants with accompanying involvement of the left axillary lymph nodes. In the second patient, there was initially a single metastasis in one breast, but later multiple ones appeared the other breast.
In our patients, initial systemic chemotherapy was followed by surgical removal - mastectomy or excision of the lesions; one of the patients additionally underwent radiotherapy.
A summary of our patients’ data is shown in Table 2.
Table 2
Summarized patients’ data
Imaging
Metastases to the reproductive organs are so rare that papers devoted to staging bone and soft tissue sarcomas do not even address them, focusing mainly on bone and lung metastases [34]. Nevertheless, PET-CT, mentioned in these papers in the context of looking for bone and lung metastases (in the lungs considered as less effective than CT alone) is predestined to detect these lesions as well as PET-MRI, the use and usefulness of which are the least described due to its high cost and low availability [35].
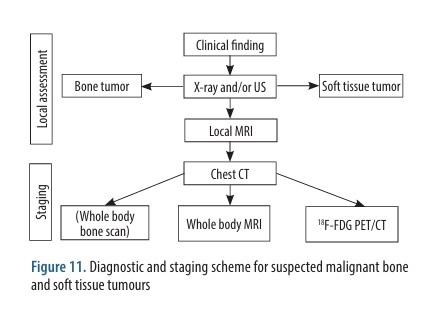
Whole-body MRI enables the investigation of systemic spread of malignant neoplasms and is cautiously recommended in their diagnostics and staging in children as well as in the surveillance in cancer predisposition syndromes [36]. In our centre WB-MRI is used routinely in children with ES, RMS, neuroblastoma, and Langerhans cell histiocytosis. The diagnostic and staging scheme for suspected malignant bone or soft tissue tumours is shown in Figure 11.
Ultrasonography is the initial imaging modality in the local assessment of focal changes in the reproductive tract in all age groups and in breasts in young women. Being strongly dependent on the operator’s skills and experience (and on the quality of equipment), it rarely allows for full assessment and is followed by MRI. According to the recommendations of European and American scientific societies (ESUR – European Society of Urogenital Radiology, ACR – American College of Radiologists) and the ALARA principle (as low as reasonably achievable), computed tomography – as a method having too low tissue resolution and burdening the patient with ionising radiation, which is particularly important in children and women of childbearing age – is not applicable to the local evaluation of the reproductive organs, and even more so in the case of breast. Characterisation of indeterminate adnexal masses, and evaluation of infiltrations of the uterus and vagina and of breast lesions are the domain of MRI, which demonstrates higher specificity [37-39]. Some authors emphasise the utility of breast MRI in patients with sarcomas, especially when the primary tumour is in the upper extremity, even if there are no clinical features of secondary breast involvement [40]. However, this has not been turned into an official recommendation.
CT is used in special cases, as in our patient (no. 2), in whom countless calcium plugs would not have been appreciated without this method of imaging.