Introduction
Magnetic resonance imaging (MRI) is commonly used to assess the knee; however, contraindications to MRI, such as periorbital metallic foreign bodies, cochlear implants, and cardiac devices, preclude the use of MRI. As a result, these patients often proceed to diagnostic arthroscopy, an invasive procedure requiring general anaesthesia, which is associated with higher risks to the patient and costs to the healthcare system [1,2]. Another alternative is computed tomography arthrography, which has been shown to have moderate sensitivity and high specificity for detecting meniscal and ligamentous pathology; however, it is associated with risks of infection and contrast reaction [3].
Dual-energy computed tomography (DECT) is based on the differential attenuation of tissues at 2 different energy levels, and it holds the potential to be a non-invasive alternative to assess intraarticular knee pathology in patients with contraindications to MRI [4-6]. DECT is used in musculoskeletal imaging in the assessment of crystal arthropathy, and it has been investigated for metal artifact reduction, bone marrow oedema detection, tendon assessment, and cruciate ligament injuries [6-11].
Various reconstruction methods have been used, including collagen-specific colour mapping, dual-energy bone removal, and virtual monochromatic images [6,9-11]. While hardware size and cost currently prohibit the routine clinical use of true monochromatic beams [7], virtual monochromatic images can be created by linearly blending low- and high-energy levels from DECT at different ratios to mimic a true monochromatic X-ray beam [8]. This provides an opportunity to take advantage of the potential diagnostic utility of an X-ray beam at a specific energy level. Studies have shown utility for DECT in the acute trauma setting and for detecting anterior cruciate ligament (ACL) rupture [5,6]. They also found that the optimal keV level for diagnosing ACL tears was 63 keV, and Gemstone Spectral Imaging was superior to bone removal or collagen-specific colour mapping [6].
Despite the promising results of using DECT in musculoskeletal imaging, no studies, to our knowledge, have assessed the potential of DECT to assess the menisci. We hypothesised that virtual monochromatic images would provide improved contrast resolution at specific energy levels. Thus, the objective of this study was to determine the feasibility of assessing the menisci using virtual monochromatic images obtained using DECT, and to determine which keV levels optimise contrast resolution.
Material and methods
Ethics approvals
Research Ethics Board approval was obtained from our local University Ethics Review Board (Bio 16-171), and patients’ consent was waived.
Patient selection
Patients were included in the study if they had a DECT scan performed of one or both knees. At our centre, the DECT protocol is used when there is a clinical question regarding crystalline arthropathy. Patients with imaging features of chondrocalcinosis and knee arthroplasty were excluded from the study. After applying the above inclusion and exclusion criteria, all patients were included in the analysis, forming a consecutive series.
Image acquisition and reconstruction
All DECT exams were performed on a Discovery CT750 HD system (GE Healthcare, Chicago, Illinois, United States). Gemstone Spectral Imaging, a dual-energy technique that uses rapid kV switching between 80 kVp and 140 kVp, was used for all exams [12]. Acquisition parameters were as follows: current, 375 mA; detector coverage, 20.0 mm; helical thickness, 0.625 mm; pitch, 0.531 : 1; speed, 10.62 mm/rot; coverage time, 8.0 s; coverage speed, 17.70 mm/s; and matrix size, 512. CTDIvol was 25.77 mGy for GSI-33 (Body – Large).
Virtual monochromatic images were reconstructed at 40 keV, 73 keV, 106 keV, and 139 keV using the Advantage Workstation Server 2, version 2.0-5.5 (GE Healthcare, Milwaukee, Wisconsin, United States). Images at each energy level were reformatted in sagittal and coronal planes.
Radiologist assessment
Sagittal and coronal reformats at each chosen monochromatic energy level were read by consensus by 2 fellowshiptrained musculoskeletal radiologists using K-PACS (IMAGE Information Systems, London, United Kingdom). Images at each monochromatic energy level were read in a random order to avoid bias. Two musculoskeletal radiologists assessed contrast resolution of the medial and lateral menisci on a 5-point scale, where 1 is lowest perceived contrast resolution and 5 is highest perceived contrast resolution. Contrast resolution was defined as how well the difference between the menisci and the subcutaneous fat of the knee is rendered [13]. Scores for contrast resolution were obtained separately for sagittal and coronal reformats.
Statistical analysis
Medians and interquartile ranges of contrast resolution were determined for each energy level. As patients were repeatedly assessed at different energy levels, Friedman’s test was used to detect the presence of any difference in median scores between the 4 energy levels. If a significant difference among energy levels was found, this was followed by pairwise Wilcoxon signed rank testing to determine which energy levels were statistically significantly different from each other. A Bonferroni correction was made to the alpha level (0.05/6 pairwise comparison = 0.008) for pairwise assessments. Statistical analysis was performed using SPSS, version 24 (IBM, Armonk, NY).
Results
Seventeen knee exams from 10 unique patients met the criteria for inclusion in the study. All patients included in the study cohort were males. The median age of patients was 46 years (interquartile range, 35-53 years). There were 9 left and 8 right knees. The clinical indication for all DECT studies was to assess for the presence or absence of crystalline arthropathy.
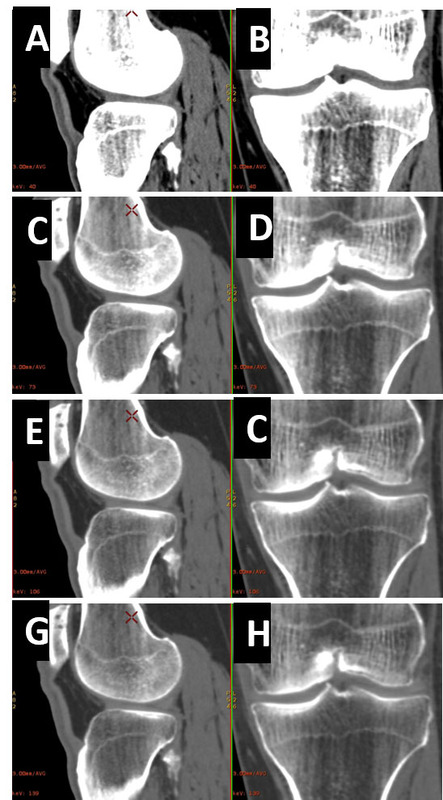
Representative images of the menisci at each keV level are provided in Figure 1. Virtual monochromatic images at 40 keV were scored highest for contrast resolution, with statistically significant difference assessments of contrast resolution at 40 keV and 76 keV (Table 1). Friedman test: p < 0.0001; pairwise comparisons: 40 keV vs. 73 keV, p = 0.0002; 40 keV vs. 106 keV, p = 0.0002; 40 keV vs. 139 keV, p = 0.0002; 73 keV vs. 106 keV, p = 0.001; 73 keV vs. 139 keV, p = 0.0003; 106 keV vs. 139 keV, p = 0.10.
Table 1
Score distribution at differing keV levels – contrast resolution
Figure 1
53-year-old male undergoing dual-energy computed tomography to assess for crystalline arthropathy. Representative virtual monochromatic images of the lateral meniscus at 40 keV in sagittal (A) and coronal (B) planes, 73 keV in sagittal (C) and coronal (D) planes, 106 keV in sagittal (E) and coronal (F) planes, and 139 keV in sagittal (G) and coronal (H) planes. Window width and level for all images is 569 HU and 105 HU, respectively. The X marks projecting over the distal femur represent reference levels at which coronal planes were centred

Discussion
Dual-energy CT has traditionally been shown to be a useful imaging technique in intraarticular calcium scoring and crystalline arthropathy [14,15]. There has been rapidly growing interest in the utility of DECT in bony and soft tissue imaging as an alternative to MRI, particularly in acute knee trauma [4,5], tendon imaging [16], cruciate ligament injuries [6,9,10,17,18], knee collateral ligament injuries [11,19], postoperative tendon graft surgery for knee ligament reconstruction [20], intervertebral disc herniation [21], and detection of post traumatic bone marrow oedema [22]. This is primarily due to the advantage that DECT offers regarding tissue composition, artifact reduction, and image optimisation [7].
Tissue decomposition can be obtained through DECT acquisitions such as dual source dual energy by Siemens Healthcare or rapid kilovoltage switching by GE Healthcare. Rapid kilovoltage switching is a DECT technology that utilises a single tube that rapidly switches energy levels, acquiring imaging data at each energy level per single rotation [23]. This was shown to provide useful tissue signature information [24,25].
This study revealed that virtual monochromatic images at 40 keV demonstrated the highest contrast resolution for assessment of the menisci, with a statistically significant difference between contrast resolution scores at 40 keV and 76 keV, Friedman test: p < 0.0001. These preliminary data demonstrated that meniscal imaging using DECT is feasible. There have been no previous studies exploring the utility of DECT in meniscal imaging. In a clinical setting, it may be advantageous for radiologists to use virtual monochromatic images at low keV levels (e.g. 40 keV) to take advantage of the improved contrast resolution of the menisci.
This study has a few limitations. First, the sample was small as the number of patients referred for DECT for crystalline arthropathy is relatively small, which was further hampered by our strict inclusion criteria. Second, the series of images assessed were separated by relatively wide energy levels of 33 keV; however, narrowing the energy level intervals may lead to subtle differences that may not be detectable. While 40-140 keV is the range that is commonly used in the DECT literature, assessing contrast resolution at further extremes may be an interesting additional avenue to explore.
Conclusions
The results of this study shed light on the emerging role of DECT in meniscal imaging. Improved contrast resolution at low KeV values could pave the way for further research in this field to determine its role in the future as an alternative option to MRI in a subset of patients who may have contraindications for MRI or in the context of a periarticular ferromagnetic foreign body obscuring the field of the view.