Introduction
The peroneal tubercle (PT) is a bony prominence located on the lateral surface of the calcaneus. The peroneal tubercle has been referred to by several names in the literature, such as the fibular trochlea, trochlear process, and peroneal trochlea. It is located anteriorly to the attachment of the calcaneofibular ligament and retro-trochlear eminence. It is flanked by 2 grooves, with the superior groove transmitting the tendon of the peroneus brevis muscle and the inferior groove transmitting the tendon of the peroneus longus muscle [1]. The PT has 3 functions: (a) to act as a fulcrum for the peroneus longus tendon; (b) to split the common peroneal tendon synovial sheath in 2 parts; and (c) as the insertion site for the inferior peroneal retinaculum, a fibrous band that extends over the tubercle and peroneal tendons, provides stability, and helps to maintain the position of the tendons during ankle movement [2]. The size and morphology of the PT varies among individuals. An enlarged PT may be the source of mechanical friction, which can eventually result in tenosynovitis [3]. The peroneus longus tendon is particularly susceptible to developing tenosynovitis because it uses the peroneal tubercle as a fulcrum during movement [4]. Understanding the normal values of the PT may be important for accurately diagnosing and preventing peroneal tendon injuries and disorders [5]. Ultrasound imaging could be a non-invasive method to measure the size of the PT [6]. The aim of this study is to investigate if ultrasound could be a useful tool to measure the size of the PT. Furthermore, this study will assess if ultrasound can be reliable, both intra- and inter-observer, when measuring the PT.
Material and methods
Study design
The inclusion criteria for this study consisted of patients who had presented themselves to the radiology department for a routine ultrasound examination of the foot or ankle. Patients were excluded from participation if they had a history of chronic injury or pain that was localised to the lateral aspect of the ankle, prior surgical intervention at the calcaneus or ankle, prior calcaneal fractures, or a diagnosis of a skeletal dysplasia. When available, prior anteroposterior (AP) radiographs of the foot were incorporated into the study. Permission was acquired from the local Ethics Committee, and informed consent was obtained from patients prior to the examination.
Measurement technique
High-end ultrasound machines (Philips Health Systems EIPQ5G) with high-resolution linear transducers (18 MHz) where used to measure the PT along the oblique axial and coronal plane.
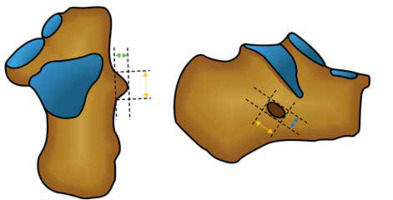
The measured planes were defined as follows (Figure 1):
oblique axial plane (OAP): 45° angulation toward the posterior aspect of the foot. The imaging plane captures the long axis of the peroneal tubercle.
oblique coronal plane (OCP): 45° angulation toward the anterior aspect of the foot. The imaging plane captures the short axis of the peroneal tubercle.
Figure 1
Clinical pictures of the position of the ultrasound transducer. A) The X on the lateral side of the foot represents the anatomical location of the PT.B, C) The position of the ultrasound transducer in oblique coronal and oblique axial position, respectively
Original figure from: Desimpel J, Posadzy M, Vanhoenacker F. Imaging features of symptomatic hypertrophic tuberculum peroneum. J Belg Soc Radiol 2017; 101 (Suppl 2): 7 [15].

The images were obtained by an attending radiologist with 33 years of experience, who acquired them in the predefined planes using 5-second image clips in the region of the peroneal tubercle moving from cranial to caudal in the oblique axial plane and from posterior to anterior in the oblique coronal plane.
The width (W) and height (H) of the PT were measured on oblique coronal images at the level of the peroneal tendons (Figure 2B). The width (W) and the length (L) of the PT were measured on oblique axial images (Figure 2C).
Figure 2
Schematic drawings of the peroneal tubercle (top down and lateral views) and its measurements. Width (green arrow) and length (yellow arrow) depicted on the top-down view. On the lateral view length (yellow arrow) and height (green arrow)
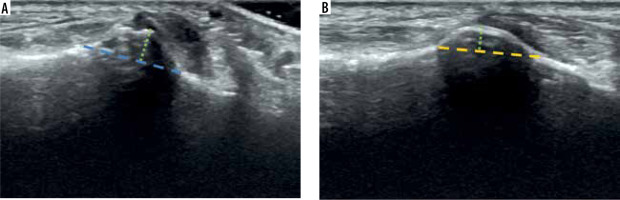
To minimise variability and increase the likelihood of obtaining reliable measurements of the peroneal tubercle, a predetermined methodology was established using both the morphology and retro acoustic shadowing to define the borders of the tubercle (Figure 3). The observers also agreed to utilise the image with the greatest measured dimensions for their respective measurements.
Figure 3
Ultrasound images of the peroneal tubercle. A) Oblique coronal view with consensus measurement techniques for width (green arrow) and height (blue arrow). B) Oblique axial view with length (yellow arrow) and width (green arrow) measurements
The acquired ultrasound images were evaluated twice by 2 radiologists. Reader 1, a resident with 3 years of experience, and reader 2, an attending with 33 years of experience. Both readers evaluated their sets of images independently with a minimum of 2 months between the 2 assessments.
On AP radiographs both width and length measurements of the PT were determined by consensus. Height measurements were omitted on plain radiographs due to its alignment parallel to the direction of the X-ray beam.
Results
Demographics
The study population consisted of 100 subjects, with even distribution of genders, consisting of 52 females and 48 males. The age distribution of the participants was normally distributed. Among the study population, 80 right feet (53.3%) and 70 left feet (46.7%) were analysed. Three patients had no measurable PT peroneal tubercle, and 30 patients had prior radiographs the feet.
Peroneal tubercle measurements
Averaged measurements for both observers are summarised in Table 1.
Table 1
Averaged measurements for both observers
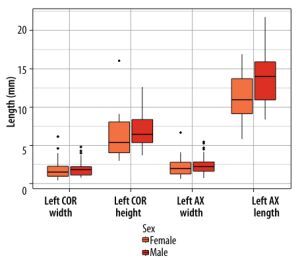
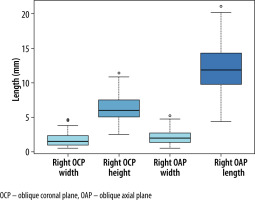
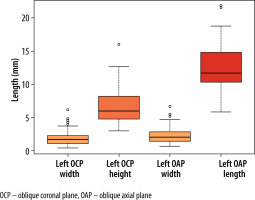
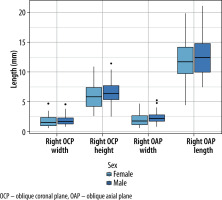
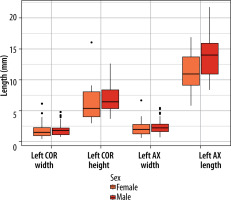
The mean width of the right PT measured in the OCP was 1.8 mm (SD 0.9), in comparison the width measured on the OAP, which had a mean of 2.1 mm (SD 1.0). The mean height of the right PT was 6.3 mm (SD. 2.1), and the mean length was 12.2 mm (SD 3.5) (Figure 4). On the left side the mean width in the OCP was 1.7 mm (SD 1.2); in comparison, the width on the OAP had a mean width of 2.3 mm (SD 1.3). The mean height of the PT was 6.5 mm (SD 3.0). The mean length was 12.6 mm (SD 3.4) (Figure 5).
Analysis of differences between genders
In 7 of the 8 measurements, no significant differences were seen between male and female subjects in both the right (Figure 6) and left feet (Figure 7). However, in the left length measurements, a statistically significant difference (p < 0.00437) between male and female measurements was found. It should be noted that there was a considerably higher degree of deviation (SD 3.4) in these length measurements, which suggest that this difference can be attributed to measurement errors. There appears to be a trend suggesting that females exhibit slightly smaller PT measurements than males, but this trend was not statistically significant.
Intra-rater reliability of measurements
Rater 1: Observer 1 had intraclass correlation coefficients (ICC) values ranging from 0.886 (good) to 0.984 (excellent), indicating a high degree of consistency when measuring the peroneal tubercle (Table 2). The 95% confidence intervals (CI) for each measurement were relatively narrow, indicating a high level of precision.
Table 2
Intra-observer reliability, rater 1
Rater 2: Observer 2 had reliable measurements with ICC values ranging from 0.710 (moderate) to 0.911 (excellent) (Table 3). However, some measurements, such as the length and height had lower ICC values compared to other measurements. The 95% CI for the length and to a lesser extent height measurements were wider, which indicates that the precision of the measurements varied to some degree.
Table 3
Intra-observer reliability, rater 2
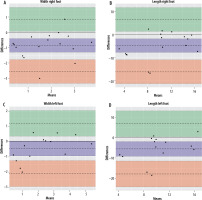
Differences in width measurements between 2 planes
The Pearson product moment correlation test shows a significant correlation of 0.81 between the 2 sets of measurements, indicating that the 2 width measurements in different planes (right side) are linearly related (Table 4). The p-value of less than 2.2 × 10–16 indicates that the correlation is highly statistically significant. Bland-Altman plots were used to visually assess the agreement of right width measurements in the OCP and OAP, showing acceptable levels of agreement between the raters. Similar results were observed for the left foot measurements (Supplementary Figures S1-S4).
Table 4
Correlation and agreement of right width measurements in the OCP and OAP
Inter-rater reliability of the measurements
Statistical analysis suggests that there is moderate to excellent inter-rater reliability between rater 1 and rater 2 when measuring the tuberculum peroneum, with ICC values ranging 0.636-0.930 (Table 5). However, the ICC values in both feet for height (0.757-0.818) and especially length (0.636-0.757) are lower compared to width (range 0.807-0.930). The 95% CI for most of the measurements were relatively narrow, indicating a high level of precision in the measurements between rater 1 and rater 2.
Table 5
Inter-observer reliability, rater 2
Differences between ultrasound and radiographic measurements
The difference in measurements between ultrasound and AP radiographs are summarised in Table 6.
Table 6
Difference between measurements on plain films compared to ultrasound in millimeters after subtraction (radiographs – ultrasound)
Both the mean and median values of differences between width and length have a negative value, which indicates that the measurements on plain films are smaller than those on ultrasound. Width measurements of both right and left feet were closer to zero (mean values of –0.8569 mm and –0.4482 mm, respectively) compared to the length measurements (mean values of –4.786 mm and –5.507 mm, respectively).
The Pearson product moment correlation test shows a significant correlation of 0.7 and 0.9 between width measurements of the right and left foot, respectively, indicating a strong correlation between the width measurements on both ultrasound and radiographs (Table 7). The respective p-values of 1.532 × 10–3 and 1.75 × 10–5 indicates that the correlation is highly statistically significant.
Table 7
Correlation and agreement of width and height measurements on ultrasound and radiographs (radiographs – ultrasound)
However, for both the right and left foot, correlation between length measurements from X-rays and ultrasounds was not statistically significant.
Bland-Altman plots (Figure 8) were used to visually assess the agreement of width and length measurements. While width measurements showed acceptable levels of agreement, the length measurements exhibited considerable variability.
Discussion
Prevalence, size, and demographics
The prevalence of a PT varies widely in the literature. Pfitzner [7] reported an incidence of 39.9%, Laidlaw [8] 36.5%, Burman and Oertl [9, 10] both reported 68%, and Edwards [1] reported 44%. A study by Agarwal found that the incidence of peroneal tubercle was 97.6% in one region of India (Lucknow) and 57.5% in another region (Agra), which was attributed to genetic differences [11]. In our population 97% of patients had a measurable PT. Besides differences in ethnicity and genetics, the different methods used to assess the presence of a PT varied across studies, which may contribute to differences in the reported prevalences.
There is a lack of consensus in the existing literature regarding the normal size of the PT. Maximum ranges reported in previous studies for the width, length, and height of the peroneal tubercle are: (a) 0.1-10 mm, (b) 2-26 mm, and (c) 3-23 mm, respectively [1, 3, 7-10]. Comparing these values to the findings from our study shows that ultrasound measurements of the width, length, and height of the peroneal tubercle are consistent with reported values in the literature (Table 1), and this is an accurate technique to measure the PT. Overall, there was no significant size difference between male and female PT measurements.
Similar to the normal size, a clear cut-off value defining “a hypertrophic PT” is also lacking in the literature. Arbitrarily, a width greater than 5 mm is typically considered to be hypertrophic by some authors [12-14]. Furthermore, this value has been found in symptomatic patient populations [15]. In our study, only 6 patients had a PT width greater than 5 mm, with 6.7 mm being the maximum measured value. The pathogenesis of a hypertrophic PT remains a matter of debate. Some authors propose that a hypertrophic PT may be a pre-existing congenital abnormality [16]. Our results seem to agree with this hypothesis, confirming that there is no significant difference in size between the PT after the age of 14 years. This is in agreement with prior research concerning the normal development of the calcaneus, where ossification to the main calcaneal body occurs at from 10 to 12 years in females and 11 to 14 years in males [17, 18]. Another hypothesis is that hypertrophy results from repetitive and excessive traction on the peroneal tubercle [16]; while there is a visible trend, no significant difference was found between ages after 14 years (Supplementary Figures S5, S6). Our sample size of only 100 patients might not provide sufficient statistical power to detect significant differences in peroneal tubercle size across age groups, especially after the age of 14 years. Increasing the sample size and including more patients from various age groups is necessary to further examine this trend.
Intra- and inter-rater reliability of the ultrasound measurements
Rater 1 and 2 demonstrated reliable intra-rater reliability across all measurements, with ICC values ranging from good to excellent (0.886–0.984) for rater 1 and moderate to excellent (0.710-0.911) for rater 2. These results suggest that that both raters are able to consistently measure the peroneal tubercle on ultrasound. The relatively narrow 95% CI of rater 1 (Table 2) indicates that there is a low likelihood of random measurement error. While the 95% CI of rater 2 (Table 3) was higher for some measurements, the precision of rater 2’s measurements are still acceptable. A more robust standardisation of measurement protocols could be useful to further improve the precision of the measurements. Some measurements, such as the length and, to a lesser extent, height, had lower ICC values in both raters compared to other measurements. This finding was not unexpected because both raters agreed that accurately defining the length and height of the PT on ultrasound was more difficult than the width.
Inter-rater reliability ICC values (Table 5) for width measurements on both the OCP and OAP fall within the good to excellent range (0.807-0.930), indicating a high level of agreement between rater 1 and rater 2. These results suggest that both raters were able to consistently measure the width of the peroneal tubercle in the oblique coronal plane. The ICC values regarding length and height ranged from moderate to good (0.636-0.818), indicating a lower level of consistency between rater 1 and rater 2 compared to the width measurements. In particular, the measured length in the OAP demonstrates the lowest inter-rater reliability with an ICC value of 0.636. The 95% CI for length and height measurements were also generally wider compared to those for width measurements, suggesting a higher degree of variability in inter-rater reliability. These results indicate that the width measurements of the PT were more consistent and precise than length and height measurements between raters.
Differences between ultrasound and radiographic measurements
For the width measurements, Bland-Altman analysis indicated a mean difference (bias) of –0.86 mm for the right foot and –0.45 mm for the left foot. This implies that the X-ray measurements were, on average, less than 1 mm lower than those obtained from ultrasound. For the clinical purpose of measuring the PT this could be regarded as generally within clinically acceptable limits. Regarding the length measurements, the observed bias was –4.79 mm for the right foot and –5.51 mm for the left foot. This consistently showed that X-ray measurements were significantly lower than those from ultrasound. This disparity can be attributed to the distinct plane in which measurements were taken on ultrasound as opposed to plain films. On plain films the PT length appears foreshortened due to the inclination of the X-ray beam. Consequently, direct comparisons of length measurements between ultrasound and plain films are not feasible.
Limitations
Several limitations should be acknowledged regarding our approach to measuring the PT on ultrasound. First, our study involved only 2 observers, and future research should consider incorporating a larger number of observers to enhance the accuracy and generalisability of the findings. Second, potential bias may have been introduced because the ultrasound “cinematic loop” images were acquired by a single radiologist and subsequently used for all measurements. To mitigate this, future studies could consider having multiple radiologists independently acquire images to minimise potential bias. Regarding the sample size, the 100 patients included in our study may not provide sufficient statistical power to detect significant differences in PT size and development across age groups, particularly after the age of 14 years. Increasing the sample size and including a more diverse age distribution is important in future research to better elucidate these relationships. This study focused solely on measuring the PT, without taking into account potential influences from the surrounding soft tissue structures. Additional research is essential to clarify any confounding factors. Furthermore, due to concerns about radiation exposure, we only used previous AP plain films of the feet for comparison. The authors did not conduct individual measurements of the peroneal tubercle on radiographs; instead, consensus-based reference measurements were agreed upon. Ideally, a CT scan would have been used to accurately assess the PT’s size and morphology. Lastly Bland-Altman plots only provide a visual representation of agreement but might not capture all aspects of bias or systemic errors.
Conclusions
In this study, the prevalence and size of the peroneal tubercle were assessed using ultrasound in a sample of 100 patients. The results showed ultrasound could be a useful modality to measure the size of the peroneal tubercle. Width, length, and height measurements were generally consistent with values reported in the literature. Compared to plain radiographs, width measurements showed reasonable agreement within 1 mm limits. Both intra- and inter-rater reliability of the examined measurements on ultrasound had good to excellent intra-rater reliability for both raters and moderate to excellent inter-rater reliability. Width measurements showed the highest level of consistency and precision between raters, while length and height measurements exhibited a slightly lower reliability. A more robust standardisation of measurement protocols might be helpful in improving the precision of these measurements.